PHMI leaders explain how the Implementation Model was created, who the initiative focuses on and why, and what success looks like long-term.
Let’s start with why this initiative is so important. What’s the need you are addressing?
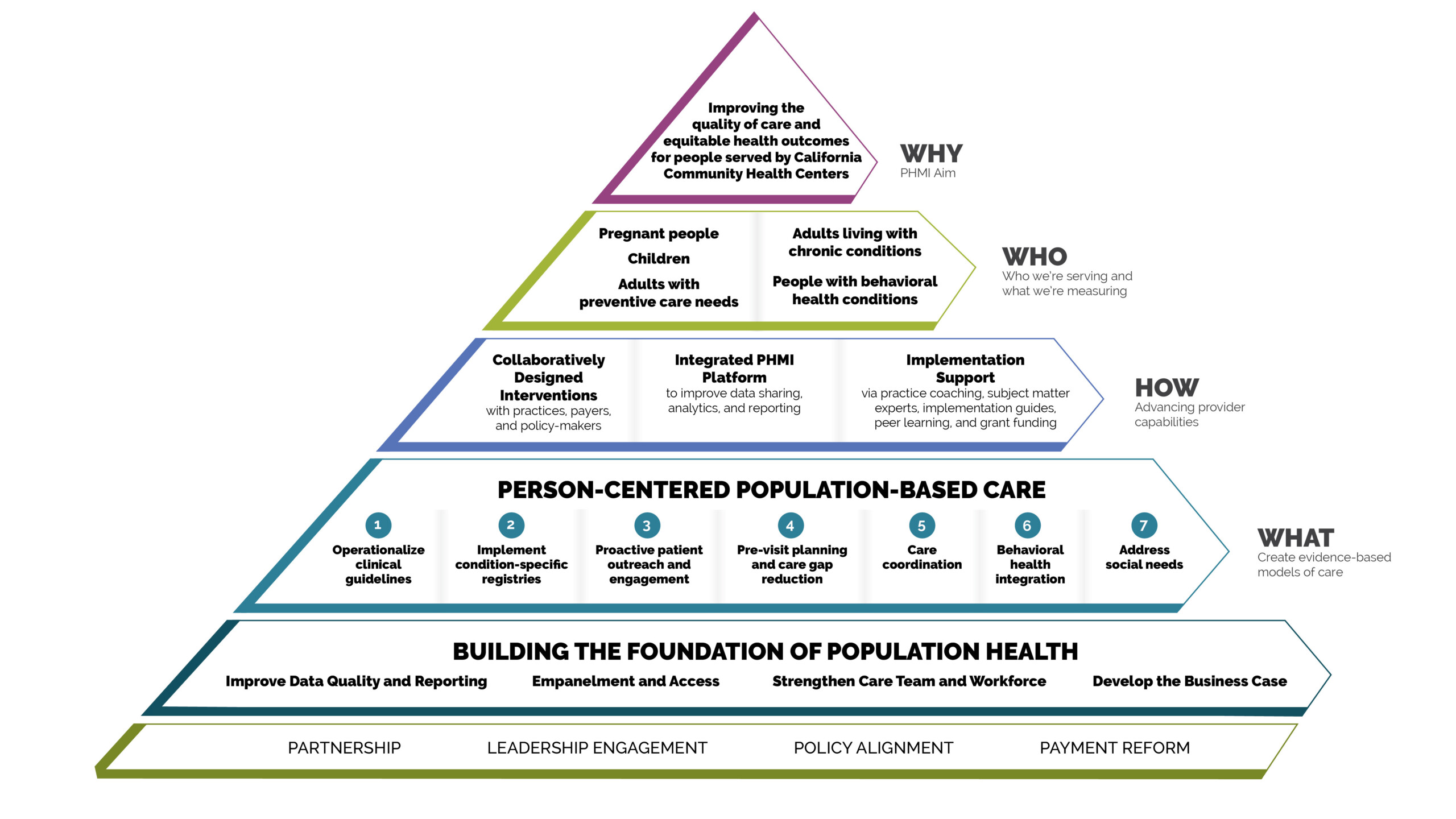
CHC’s are such a vital and vibrant part of the Medi-Cal safety net system, we’re focusing on helping them build better care models, improving care, and fostering growth in key areas. We’re also looking systemically, including at the evolving policy level, thinking about vertical integration at a time health plans fundamentally need to do something different. By working through barriers that exist at different levels of the system, we serve as a catalyst for clinical and care-model change and help prepare CHCs both for CalAIM and benefits transformation. A lot of the work is about coordinating different partners, for example helping CHCs get data from their health plans, but it’s also thinking holistically about the populations the CHCs serve and what upstream enablement needs to happen in communities.
Can you share how the initiative design came into being?
From the beginning, the initiative has been collaboratively designed by CHCs, California Department of Health Care Services (DHCS), and Kaiser Permanente, with a focus on aligning payment structures with equity-based population health. We looked at the real life experiences at CHCs, the evidence base, and Kaiser Permanente’s knowledge as an integrated delivery system, along with doing a lot of testing. A big part of this is acknowledging there is a lot we don’t know. We’re all on a learning journey together.
What foundation are you building from?
We know there are a set of common standards everyone needs to meet to establish core population health management competence. They include understanding who the CHCs’ patients are, who isn’t coming in for care, and who is going to take point with certain patients. They also need to ensure patients know their care team. Key is making patients the primary focus rather than focusing on models that don’t necessarily match the needs of patient populations, along with looking at the business case and growth models that factor in care improvement. Without data, it’s impossible to know who patients are and track their needs, so health information technology is essential.
Who will the initiative be focused on and why?
Our current focus is on the established populations in the MediCal program, patients with distinct disparities and a lot of variability in care across the state. We’re aligned with DHCS’s population health goals and we’re collaborating closely to improve outcomes and reduce disparities in these populations over the next four years.
How are you going to be building capacity in the clinics?
We’re providing highly customized tools, guides, and workflows that have been developed collaboratively with CHCs, practice coaches, and a group of subject matter experts. The customization piece is important to support advanced improvement across CHCs that begin at very different starting points. We heard from many CHCs that they don’t want coaches who don’t understand their world, so we identified a coaching team that knows the CHC environment, complemented by subject matter experts who can go deep. Peer network support is also an important part of the design, with CHCs innovating and learning together. It’s a multi-level intervention.
How do the elements of your implementation work with the clinics support each other?
One interesting piece is that in the work with CHCs we didn’t focus on measures first, instead we invested in the collaborative design process to build foundational capabilities. This established a foundation from which teams can build, linking to specific HEDIS measures. Working with the individual CHCs, we’re focused on better data, a solid business case, and identification of champions who carry the work forward. This is combined with a shared learning cycle that includes best practices and tools to provide both definition and direction.
How will you know what’s working? What will you be measuring?
We’re keeping a close eye on levels of interest and engagement, knowing that no one is forced to participate. Right now, we’re in the process of working with the CHCs to understand what everyone hopes to do with their care model and care delivery, and what capacities they’ll need to build to do it. It will be a good sign when roles and responsibilities within care teams are clear—when teams know their patients and vice versa. We’ll also be making measurable progress with specific sub-populations, seeing positive metrics and favorable responses from patients about their care. Ultimately, we’ll know we’re making progress when providers are carrying forth the care delivery model they helped design and patients are receiving the care they need.