KEY ACTIVITY #7:
Use Care Gap Reports or Registries to Identify All Patients Eligible and Due for Behavioral Health Screening and Follow-Up
This key activity involves the following elements of person-centered population-based care: operationalize clinical guidelines; implement condition-specific registries; address social needs.
Overview
This key activity provides detailed guidance on how to reliably and efficiently develop and use a regularly updated list of all patients eligible for recommended or standard screenings or interventions (e.g., behavioral health screening and documentation of follow-up) through a care gap report or registry. Note that this activity focuses on behavioral health services, but many other preventive and maintenance services are needed to provide comprehensive preventive care. See the Pre-Visit Planning: Leveraging the Team to Identify and Address Gaps in Care resource for a more complete list.
Care gaps are gaps between the recommended care that a patient should receive according to clinical guidelines and protocols and the care a patient has actually received. Most EHRs already have a module that identifies what services are due for each patient, including behavioral health screens.
Rather than put the responsibility for searching through charts or remembering which patients need further preventive care or follow-up on the individual care team member, this activity provides guidance for how the practice can efficiently leverage electronic health records (EHRs) for all its patients.
Care gap reports are essential for practices to understand and continually improve consistency and reliability for screening for behavioral health needs. At the care team level, care gap reports focus on gaps for patients assigned to your care team and help your team understand which patients you are responsible for. These lists can be used to:
- Support improvements to the pre-visit planning process, develop standing orders, and improve other routine clinical workflows designed to systematically identify and address gaps in care.
- Prioritize patients for whom care teams should provide proactive inreach and reminders for engaging in care.
- Support quality improvement efforts with an equity lens.
In integrated care teams, care gap reports can be especially helpful in supporting the team to leverage all patient encounters toward reducing care gaps. For example, when a patient is seen by a behavioral health specialist and the care gaps report indicates missing chronic care screens or interventions, the behavioral health specialist can connect the patient to the medical assistant to ensure that chronic care activities are initiated.
Actively identifying and acting on care gaps ensures all eligible patients assigned to your practice receive timely screenings and other preventive services. This reduces the burden on the healthcare system by preventing more severe health issues in the future. Furthermore, reducing missed or delayed diagnoses using care gap reports during pre-visit planning is important to support reliable integration of behavioral health screenings into primary care, which can help to identify and address issues early. Early identification of depression or anxiety can prompt further exploration of the impact of these needs and begin to explore the relationship of behavioral health and chronic disease management, including how behavioral health needs may complicate patients’ engagement in preventative care and chronic disease management.
Many practice patients experience barriers in accessing care due to structural and historical racism, homophobia, xenophobia, and other biases that have historically disadvantaged individuals and groups from receiving equitable services. Defining clear criteria and gaps for patients due for specific screenings or preventive services helps to illuminate groups that have not had historically had equitable access and combats biases by standardizing expectations for who is due for what care, providing a starting point for ensuring reliable and equitable access.
Mental health disorders, such as depression, continue to be underdiagnosed among patients of color. Research suggests that African American Medicare patients have a significantly lower rate of screening and treatment than non-Hispanic white patients.[1] Staff can identify potential barriers to patients accessing and engaging in care by using enhanced care gap reports to filter and display the data alongside demographics, social needs, behavioral health needs, and communication preferences. This information can be used to promote a person-centered approach across the care journey, from conducting inreach in the patient’s preferred language to co-creating the care plan, supporting their engagement in community-based care provision, and fostering self-care behaviors.
Furthermore, care gap reports that segment the data into cohorts based on demographics and other personal information may help the team identify inequities in care, access and outcomes, which can inform improvement efforts.
Care gap reports can be used during pre-visit planning to identify people for whom social needs screening has not yet been completed. This creates an opportunity to identify unmet social health needs and connect patients with resources that address their social needs.
Many EHRs already have a module that identifies what services are due for each patient, while others do not. Where this functionality is available, it may not be configurable to align with the health center’s specific protocol or be able to incorporate outside data. Other options for developing registries include supplemental applications, population health platforms, and freestanding customized databases that draw data from the EHR and other sources.
Care gap reports may be embedded in electronic health records or made available through other technology channels and are useful both at the individual patient level and aggregated to identify groups of patients to facilitate population-level management through registries. See Appendix D: Guidance on Technological Interventions.
A registry can be thought of as a list of patients sharing specific characteristics for tracking and management. Both care gap reports and registries should have the capacity to segment patients by age, gender, race and ethnicity, and language.
Other relevant HIT capabilities to support or relate to this activity include care guidelines, care dashboards and reports, quality reports, inreach and engagement, and care management and care coordination.
Access to outside data may be a consideration (e.g., data from other practices) as services received outside the practice may be part of compliance. While claims data may be helpful in this regard, lag time may impact its usefulness. Patient-facing applications should be strongly considered to assure they are informed and appreciative of the nature and importance of recommended care. In California, many healthcare organizations are required or have chosen to participate the in California Data Exchange Framework (DxF), which can facilitate data sharing between clinics, MCPs and other partners.
FIGURE 5: EXAMPLE CARE GAP REPORT FOR AN INDIVIDUAL PATIENT
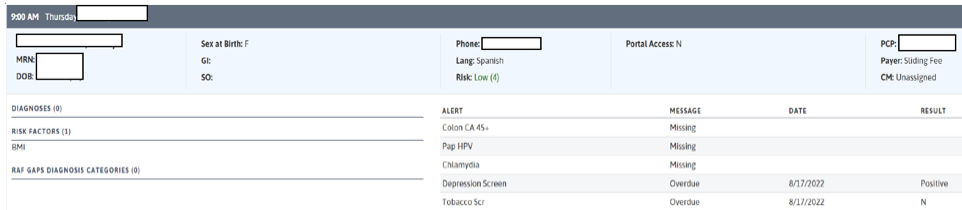
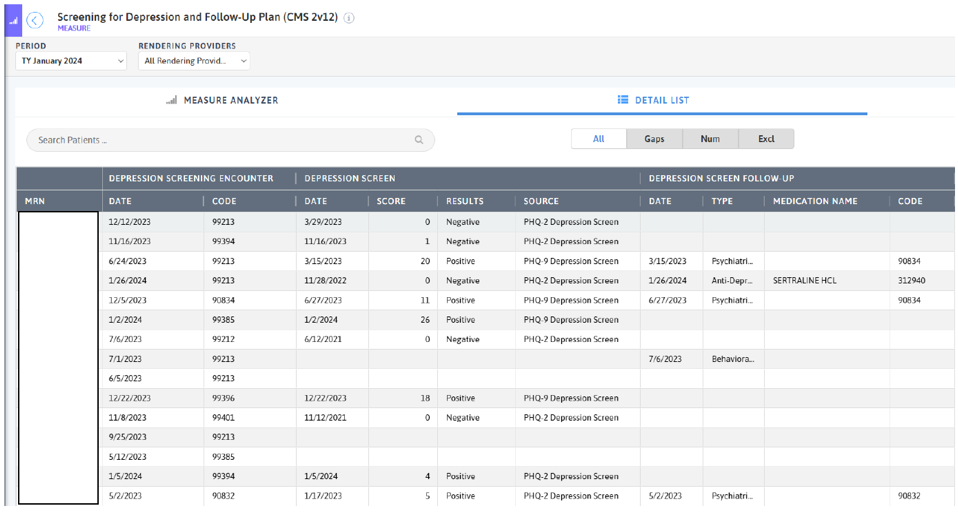
FIGURE 6: EXAMPLE CARE GAP REPORT AT THE POPULATION LEVEL
Action steps and roles
1. Plan the care gap report.
Suggested team member(s) responsible: Panel manager or data analyst. If it is not clear how the report can be produced, this step may involve one or more people from the practice who work on the EHR and, possibly, the EHR vendor.
As a team, decide what screenings or treatment guidelines are appropriate for your population of focus and prioritize the most important care gaps to run reports on. Start with the core and supplemental measures and any process measures your practice is tracking, and consider if there are any other gaps, clinical guidelines or measures your practice feels important to prioritize.
Identify the inclusion criteria for each report, such as age, any exclusion criteria, and factors that make someone high risk.
Care gap reports should include, at a minimum, for patients 12 years and older:
- Patients with an absence of a depression screen using a validated tool within the past year. For patients previously diagnosed with depression, the care gap report can also indicate that they are due for a repeat PHQ-9 to monitor their symptoms. A smaller time interval between PHQ-9 administration may be set by the practice for patients who have a depression diagnosis.
- For HEDIS compliance, ensure that a gap report is available to identify patients who screened positive for depression but have no documented follow-up care within 30 days. See the PHMI Clinical Practice Guidelines for Key Medi-Cal Populations of Focus for more information defining follow-up.
- Practices also use gap reports to track follow-up in patients who screened positive for depression and are not showing remission within six months, as they may require additional follow-up.
2. Build the report.
Suggested team member(s) responsible: Data analyst.
Determine whether the EHR has an existing report or one that can be modified to fit the inclusion criteria. You should talk to staff who are familiar with the electronic record; in some cases, it may be necessary to consult with the EHR vendor to confirm this information and how to run the report.
The care gap format should include:
- Criteria for inclusion in the report.
- The overall compliance rate for the care gap being measured.
- All patients eligible for the screening and their addresses and phone numbers.
- The last date the screening was performed and any follow-up recommendations or next steps.
- Preferred method of communication (e.g., phone, email, text).
Reports should be able to display and/or disaggregate the data based on:
- Race, ethnicity and language (REAL) as well as sexual orientation and gender identity (SOGI).
- Any known social or behavioral needs.
- Communication preferences or other preferences that would inform the screening modalities offered, such as documented declination of prior screenings.
- Data on any other characteristic, including insurance data, that could pose a barrier to completing screening.
3. Standardize the data format.
Suggested team member(s) responsible: Panel manager or data analyst.
Standardizing the data format and where it is entered is critical to ensuring accuracy in the resultant report. Once you know that a report can be produced, understand the specific data elements that are needed to produce the reports.
Document how each data element must be entered into the EHR in order to populate the fields needed for reporting. In some cases, data on completion of screening must be entered by hand. Doing this will require a decision on the part of the practice as a whole and may require staff training and reinforcement on an ongoing basis. Where issues or apparent confusion are identified, regular discussion at team huddles or staff meetings will help in maintaining a standard approach.
Tip: Assign responsibility for the initial review of the reports to confirm data integrity.
4. Develop workflows to support improved patient screening and preventive care completion rates.
Suggested team member(s) responsible: Panel manager, care team.
At the patient level, ensure that the care gap report can be used for or linked with reminders or alerts for clinicians as well as for sending reminders to patients who are due for screening.
Depending on communication preferences that have been expressed by patients, the patient care gap report may be exported to an automated reminder system that can trigger reminders by phone, text, email or postal mail.
In addition, as part of the practice’s pre-planning process, patient care gaps should be reviewed and flagged as part of the daily huddle. See Key Activity 8: Develop or Refine and Implement a Pre-Visit Planning Process for more details.
5. Develop a process for review of gaps at the population level.
Suggested team member(s) responsible: Panel manager.
Set a report frequency to review care gap reports at regular care team meetings or huddles in order to develop a plan for improvement at the population level. See Key Activity 11: Use a Systematic Approach to Address Inequities within the Population of Focus for more.
6. Monitor the care gap report for accuracy and completeness.
Suggested team member(s) responsible: Panel manager or data analyst.
It is critical to have bidirectional feedback with the practice’s care team about any real or potential errors in the care gap report, such as:
- Errors in how the data is entered, compared to what is required under the new standardized data format.
- Patients who are eligible for and due for screening who are missing from the report.
- Patients who have recently been screened who are still listed as due for a screening.
Errors should be investigated through a chart review. If errors in the report specifications are discovered, the care gap report or process for producing the report should be modified. If the issue is incorrect documentation, staff training and reinforcement of documentation standards will be required.
Additional consideration for sustainability: Ensure there is an internal process for updating the criteria included in the EHR for care gap reports as clinical guidelines change.