KEY ACTIVITY #8:
Develop or Refine and Implement a Pre-Visit Planning Process
This key activity involves the following elements of person-centered population-based care: operationalize clinical guidelines; pre-visit planning and care gap reduction; care coordination; address social needs; behavioral health integration.
Overview
This activity provides guidance for how the care team can effectively and efficiently embed behavioral health screenings and considerations into the practice’s pre-visit planning process (PVP). Pre-visit planning is typically driven by the medical assistant with help from other care team members and includes steps taken:
- Prior to a scheduled appointment, to scrub the chart and identify any pre-visit tasks per the pre-visit checklist.
- The day of an appointment, during the daily huddle and before the patient sees the PCP.
- At the end of the current visit to ensure the patient understands any actions they need to take and to schedule for any follow-up.
The average medical visit at California practices lasts just 15 to 20 minutes, and many patients come to these visits with multiple needs. Pre-visit planning works towards optimizing a team-based approach outside of these short primary care visits so patients receive comprehensive care in alignment with the latest clinical guidelines and their own preferences. Pre-visit planning is an important tool for the integrated care team to leverage all of its relationships and touch points with the patient to close gaps in care. For example, if a patient arrives at the practice for a grief counseling visit with the behavioral health specialist and the pre-visit planning summary indicates gaps in chronic care, the behavioral health specialist provides grief counseling and links the patient to the medical assistant, who then uses a standing order to provide necessary screens (e.g., foot check, etc.).
Pre-visit planning allows for better coordination of care. This can be particularly beneficial for patients with complex health needs, ensuring they receive comprehensive and equitable care. As your practice works to reduce any identified equity gaps, pre-visit planning is often a powerful activity for ensuring culturally relevant care as the care team partners with the patient to discuss follow-up actions.
The PVP should incorporate your practice’s process for screening and responding to social needs, including checking whether social needs screening is due. When social needs are identified, the team should be clear on the pathways, both during and after visits, to address and follow up on those need
Pre-visit planning draws upon similar technical enablers as care gap reporting and likewise can be facilitated at the individual patient level and at the level of groups of patients coming for care by a specific team in an appointment schedule block. The format in which planning is done needs to consider the workflow and staffing model.
Relevant HIT capabilities to support this activity include care guidelines, registries, clinical decision support, care Dashboards and reports, outreach and engagement, and care management and care coordination. See Appendix D: Guidance on Technological Interventions.
Individual patient-level pre-visit planning would be optimally enabled within the EHR, provided the EHR can store relevant information, such as assessments, plans, orders and notes outside a visit note. Pre-visit planning might also include the use of patient-facing applications, such as portal reminders, questionnaires, and self-completed screenings and assessments, which would ideally be available to the clinician and care team in the EHR.
Engagement of the expanded care team in pre-visit planning requires access by all relevant members of the care team to contribute to and view relevant information. This may require coordination with technology additional to the EHR, such as care coordination and population management applications where relevant information might be stored.
Huddle reports, in which individual patient information can be visualized in summary views across all patients within a session, can require use of technology outside the EHR, but might also be supported by developing reports populated by data from the EHR. Ideally, internal practice or EHR data should be supplemented with external data where such information completes the patient’s current status. If such electronic access is not possible, the workflow should include manual reconciliation by history from the patient.
Action steps and roles
The steps below are specific to the integration of behavioral health approaches at different steps in the PVP. Note that behavioral health is only one of many other preventive and maintenance services that can be planned for during PVP; the resource: Pre-Visit Planning: Leveraging the Team to Identify and Address Gaps in Care provides a more complete list. In general, PVP activities should include BH activities, such as depression, anxiety and unhealthy substance use screening.
1. Prior to a visit.
Suggested team member(s) responsible: Medical assistant and/or BH staff.
The medical assistant determines whether a patient is due for any BH screenings or would be best served by rescreening before the indicated time frame.
Examples include:
- Identifying that a patient is due for universal depression screening with the PHQ-2.
- Identifying that a patient has an active diagnosis of depression and has not had a repeat PHQ-9 for more than12 months and, therefore, it would be appropriate to administer the PHQ-9 rather than the PHQ-2.
- Considering whether the screen should be administered in a different form, such as in a language other than English or adolescent-specific language.
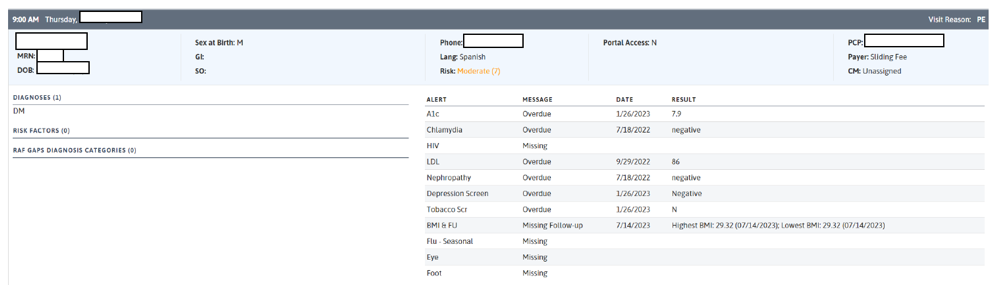
Figure 7 provides an example of how your EHR might be able to support flagging any patient overdue for depression screening.
FIGURE 7: PRE-VISIT PLANNING REPORT DETAILING OVERDUE DEPRESSION SCREENING
2. During the daily huddle.
Suggested team member(s) responsible: All team members, MAs or BH staff.
Identify patient-specific ways to tailor care delivery, including:
- Whether there need to be deviations from the typical screening flows to best serve the patient's needs.
- Whether the patient may benefit from an introduction or warm handoff to the behavioral health staff. If yes, note any necessary alterations to schedules to facilitate a real-time introduction to the BH staff.
3. Post visit.
Suggested team member(s) responsible: Medical assistants or BH staff.
Medical assistants or BH specialists establish and follow a process for checking BH screens to ensure that they were scored. The BH specialist initiates and documents appropriate and necessary follow-up.
Implementation tips
Teams that are farther along the behavioral health integration care continuum often develop methods to:
- Include BH staff in morning huddles, even though it requires creative scheduling. This may require shifting huddles to the end of the session or the end of the day to prepare for the next day.
- Make BH staff aware of clinical care gaps. While BH staff are not dispatched to complete medical screens or order missing tests, they can be another source of support and coordination for the team to help ensure that the patient completes such tasks (e.g., screening for smoking cessation or encouraging a patient to complete their Cologuard screening).