KEY ACTIVITY #9B:
Implement Suicide Risk Assessment and Response Protocol
This key activity involves the following elements of person-centered population-based care: operationalize clinical guidelines; behavioral health integration.
Overview
This key activity outlines considerations for implementing a suicide risk assessment plan or protocol to respond to patient reports of suicidal ideation. This activity focuses on a protocol for patients aged 18 and over.
Suicide is a leading cause of death in U.S. adults, accounting for over 48,000 deaths in 2021. Rates of suicide attempts and deaths vary by sex, age, and race and ethnicity. Primary care providers are in a unique position to prevent suicide. Research suggests that people who die by suicide are more likely to have seen their primary care provider shortly before their death than any other healthcare professional.[1]
Question nine of the PHQ-9 asks, “In the last two weeks, have you had] thoughts that you would be better off dead or of hurting yourself?” Suicide risk assessment protocol development aids teams in preparing to appropriately respond to positive responses to this screening. Clinicians and healthcare teams may worry about their ability to respond to such complaints in the primary care setting and may suggest this as a reason for not consistently implementing depression screening.
Additionally, suicide risk assessment training and education may improve the quality of care and utilization of services across the healthcare system by training staff to identify the appropriate level of care for patients who present with a psychiatric emergency, such as the need for crisis services.
Veterans, tribal or indigenous populations, LGBTQ+ youth, and people with disabilities are at greater risk for death from suicide due to historical discrimination.[2] In addition, adults in rural areas have the greatest rates of death and those employed in certain occupations and industries, such as construction, mining, or oil and gas extraction, may be at higher risk.[3] A systematic approach to screening all patients may increase the rates that individuals will be engaged in care and may decrease the secrecy and shame that surround this topic.
Considering the different ways that patients and their families may express suicidal concerns is a person-centered response. For all patients, clear messaging and response to thoughts of suicide may decrease feelings of shame or secrecy and contribute to lowering the rate of death by suicide.
Technology can support screening for behavioral health conditions by delivering structured guidelines, protocols, and clinical decision support to care team members responsible for carrying out assessments. It can also help by incorporating standardized screening tools into EHRs and care management and care coordination applications. These screening tools can also be made available directly to patients through patient outreach and screening technologies.
Understanding the prevalence of behavioral health conditions assists in program and resource development to track impact on health outcomes and to incorporate into risk stratification. Health information technologies used to track referrals are also important in care management.
Action steps and roles
1. Develop a workflow for suicidal ideation.
Suggested team member(s) responsible: Designated IBH implementation team member.
The risk of suicide can surface in many ways, including the systematic administration of a mental health screen, including a "Yes" response to item nine in the PHQ-9 or other screening tool, individual patient reports of suicidal ideation during a visit or over the phone, or reports by concerned family members or friends. The workflow should account for the possibility of any staff member (e.g., clinical, reception, security) encountering a patient with suicidal ideation.
Depending on the size of the practice, practices should identify two or three individual staff members who can provide immediate follow-up and further assessment for any patient who raises suicidal ideation to serve as crises responders. Typically, this person is a behavioral health staff or medical provider. This may necessitate assigning a specific staff person each day to be accessible in a timely manner for more urgent warm handoffs. Staff will need to consider what this might look like in the setting of a virtual or hybrid BH team. The practice should also identify the local crisis response phone number that staff should call, if all three identified crises response staff are not available or on site.
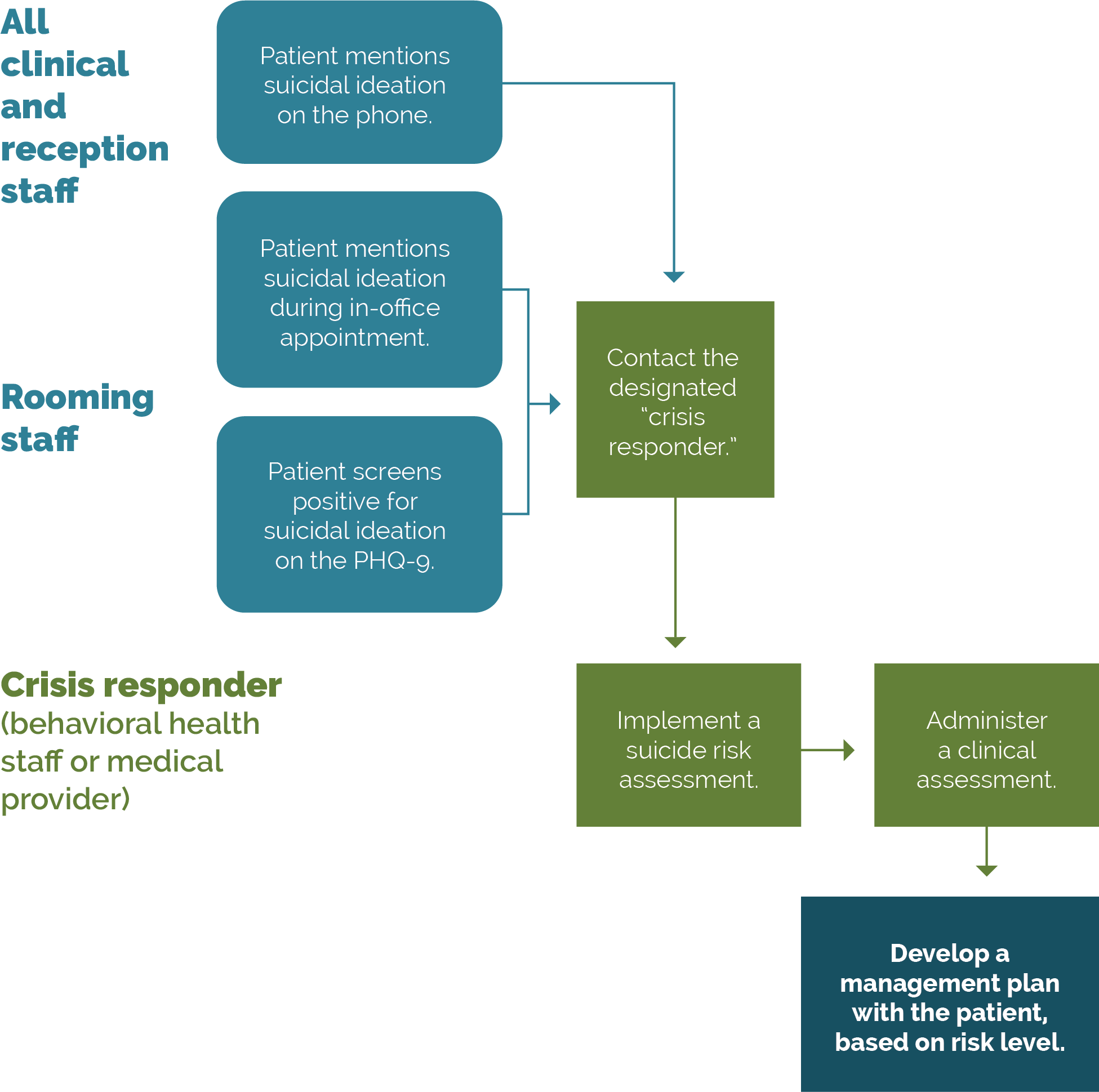
A simple example workflow is provided below and pictured in Figure 8.
To respond to suicidal ideation that is expressed during a visit, either through screening or in discussion:
- Screen for depression with the PHQ-9 (question nine). The tool may be administered by rooming staff, BH staff, or PCPs.
- Ensure a clear workflow is in place for alerting the provider of a patient’s positive suicide screening question, in addition to the designated internal resource for responding to those reporting suicidal ideation.
- Note that if a patient discloses suicidal ideation during the visit, it is likely that the PHQ-9 would be skipped or administered after the suicide risk assessment.
- Implement a suicide risk assessment. Suicide assessment tools include:
- Conduct a clinical evaluation of level of acuity.
- Work with the patient to develop a management plan with appropriate referrals and/or follow-up.
In responding to suicidal ideation over the phone, the patient service staff member contacts the designated crisis responder in the practice who implements the workflow described in the steps above.
FIGURE 8: EXAMPLE WORKFLOW FOR RESPONDING TO SUICIDAL IDEATION
2. Support staff in preparing for how to respond.
Suggested team member(s) responsible: Designated IBH implementation team member.
Post a worksheet with recommendations of what to do if a patient presents with suicidal ideation and/or requires hospitalization for suicidal thoughts in a visible or accessible place for key office staff. The Suicide Prevention Resource Center offers a template that can be used for this purpose, which is linked in the resource list below. Learn and clearly list community-based resources, including contact information for:
- Local crisis services.
- Local emergency psychiatric services.
- Transportations options for patients in crisis.
Consider running mock drills to support the staff’s comfort in responding to reports of suicidal ideation, especially for patient service representatives or triage staff who may receive calls related to this topic.
3. Conduct regular training for staff.
Suggested team member(s) responsible: BH provider or leader.
Conduct regular training for call centers, receptionists, MAs, and primary care providers on responding effectively to patient endorsement or disclosure of suicidal thoughts. While none of the processes described in this guide are simple, developing a smooth process around responding to urgent or crisis mental health situations is complex and may require practice and multiple iterations over time. Regular training can help make the process more familiar for staff and provide thoughtful responses to barriers or difficulties in implementing the process.
Resources
Endnotes
- Ahmedani BK, Simon GE, Stewart C, Beck A, Waitzfelder BE, Rossom R, et al. Health Care Contacts in the Year Before Suicide Death. Journal of General Internal Medicine. 2014 Feb 25;29(6):870–7.
- Preventing Suicide Requires a Comprehensive Approach [Internet]. cdc.gov. Available from: https://www.cdc.gov/suicide/pdf/2023_CDC_SuicidePrevention_Infographic.pdf
- Preventing Suicide Requires a Comprehensive Approach [Internet]. cdc.gov. Available from: https://www.cdc.gov/suicide/pdf/2023_CDC_SuicidePrevention_Infographic.pdf