KEY ACTIVITY #9:
Proactively Reach Out to Patients Due for Care
This key activity involves all seven elements of person-centered population-based care: proactive patient outreach and engagement, pre-visit planning and care gap reduction.
Overview
Conducting proactive outreach can ensure patients follow through on recommended care. Outreach activities for the pediatric population will almost always be directed towards the parent, legal guardian, or foster parent or caregiver. There may be incidences where a practice outreaches to an older teen, but that would depend on individual or unique circumstances.
As part of pre-visit planning (PVP) and other clinical workflows, your practice should be conducting some level of outreach to provide patients with information they may need to prepare for upcoming visits or engage in follow-up care plans determined during the visit. In addition, most electronic health records (EHRs) can be integrated with an automated reminder system for upcoming appointments and for patients who appear to have gaps in care. Patient outreach also occurs as a part of care coordination, especially around supporting patients to engage in external referrals and in follow-up to a hospital admission or discharge. See Key Activity 11: Coordinate Care for further information.
Proactive outreach to patients due for care focuses on identifying subpopulations among the patients assigned to a care team that may benefit from additional outreach and implementing more personalized reminders and touches for them to engage in care. Of note, multiple outreach modalities exist, including but not limited to phone, text, mail, email, and patient portal, and different modalities may be preferred or more effective with different subpopulations. Consider learning from others (e.g., research, campaigns, AAP recommendations), from your practice’s own experience and from testing various approaches in your QI work.
Outreach to people who are not yet actively engaged in care goes beyond this foundational activity. See going deeper Key Activity 15: Strengthen Community Partnerships for more about identifying trusted messengers in your community.
Proactive outreach ensures that patients remain engaged in care and provides an opportunity for their health needs to be identified and connected to appropriate care in a timely manner. As untreated health needs can lead to worse outcomes, proactive outreach may improve health outcomes. In addition, frequent outreach using multiple approaches can keep the practice front of mind and reinforce the practice’s concern for each patient’s well-being. Outreach and education to caregivers can boost caregivers’ sense of agency, and thereby lead to improved engagement in preventive care and better health outcomes for their children.
Additionally, in California, MCPs are expected to perform at a minimum performance level on multiple pediatric measures related to this activity. Therefore, they may incentivize and/or support practices working on pediatric care.
Focus on equity by using data to identify which populations, subpopulations or groups are experiencing disparities in gaps in care or that the current outreach and education efforts don't reach. When possible, co-designing outreach strategies with community partners and current patients promotes cultural humility and sensitivity.
Health-related social needs (e.g., income insecurity, transportation issues, and health literacy) can result in no-shows and deterioration of patient health status. Proactive outreach, coupled with awareness of clues to health-related social needs, can connect patients to community resources and establish trust in the care team.
Recognize that trauma and its sources can lead to lower engagement. Consider identifying a staff member or peer leader who is very skilled in empathic listening to reach out to caregivers and families to learn what gets in the way of children participating in well-child visits and being immunized, as well as the supports that they would most appreciate and would be most effective. This could be through email or text, phone or in-person conversation, or in focus groups.
This activity relies on similar capabilities as care gap management, utilizing population views and registries to track the pediatric population against the schedule of well-child care. These registries can be utilized to generate outreach lists for appointment schedulers and/or care managers and other care team members who might be tasked with contacting patients due for services. Many EHRs are capable of storing next appointment data that can also be used to generate lists and may link to automated appointment outreach workflows. Patient-facing outreach and engagement technologies can be utilized to deliver appointment reminders and for patient self-scheduling. These applications can include a variety of channels, such as text messaging and chatbots, to provide proactive anticipatory guidance to promote patient engagement and efficient use of visit time. Care managers might use care management applications to track and prompt well-child visits.
Other relevant HIT capabilities to support this activity include electronic access to care guidelines, clinical decision support, including patient-facing clinical decision support and care dashboards and reports. Some health centers may focus extra resources on children and families identified as high risk through risk stratification algorithms. See Appendix D: Guidance on Technological Interventions.
Action steps and roles
1. Identify subpopulations who may benefit from outreach.
Suggested team member(s) responsible: Population health staff, care managers, data analysts, community health workers.
- Start with frequent no-show patients and seek to understand their root causes, which may be related to social health-related needs or health literacy issues.
- Ask your care teams to identify patients they consider high-risk patients who have been lost to care.
- Use care gap reports to identify patients who are behind on screening or who have missed a follow-up visit. See Key Activity 3: Use Care Gap Reports or Registries to Identify All Patients Eligible and Due for Care.
2. Establish the outreach model for your practice.
Suggested team member(s) responsible: Practice leadership.
One outreach model commonly used is to hire dedicated staff as population health specialists. This person would be responsible for using care gap reports to conduct proactive outreach to patients and schedule needed follow-up. See more about this in the care team duties and recommended education resource.
However, different teams may adjust this role to fit their context. An alternative model ensures each care team includes staff with knowledge of the local environment and available resources to conduct telephonic outreach to higher needs patients and their families.
Train all outreach staff in cultural humility, motivational interviewing skills, and in the use of trauma-informed care. See Key Activity 10: Implement Trauma-Informed Care Approach Across the Patient Journey.
3. Supplement your reminder system for contacting various subpopulations.
Suggested team member(s) responsible: Population health specialist with guidance from implementation team and IT staff.
Reminders should be sent to all persons with an upcoming scheduled appointment. The clinic scheduling system will likely have a function for generating automated reminders with an option for patients to cancel or reschedule if they cannot keep the appointment. Reminders should also be sent to all patients who appear to have gaps in care and missed appointment reports. See more about updating your See Key Activity 3: Use Care Gap Reports or Registries to Identify All Patients Eligible and Due for Care to learn more about enabling setting up automated reminders.
Automated reminder systems can support efficiency and reliability. However, more intensive reminders where the patient receives a personalized telephone call from their care team may help patients who are at higher risks of nonattendance or being lost to care.[1]
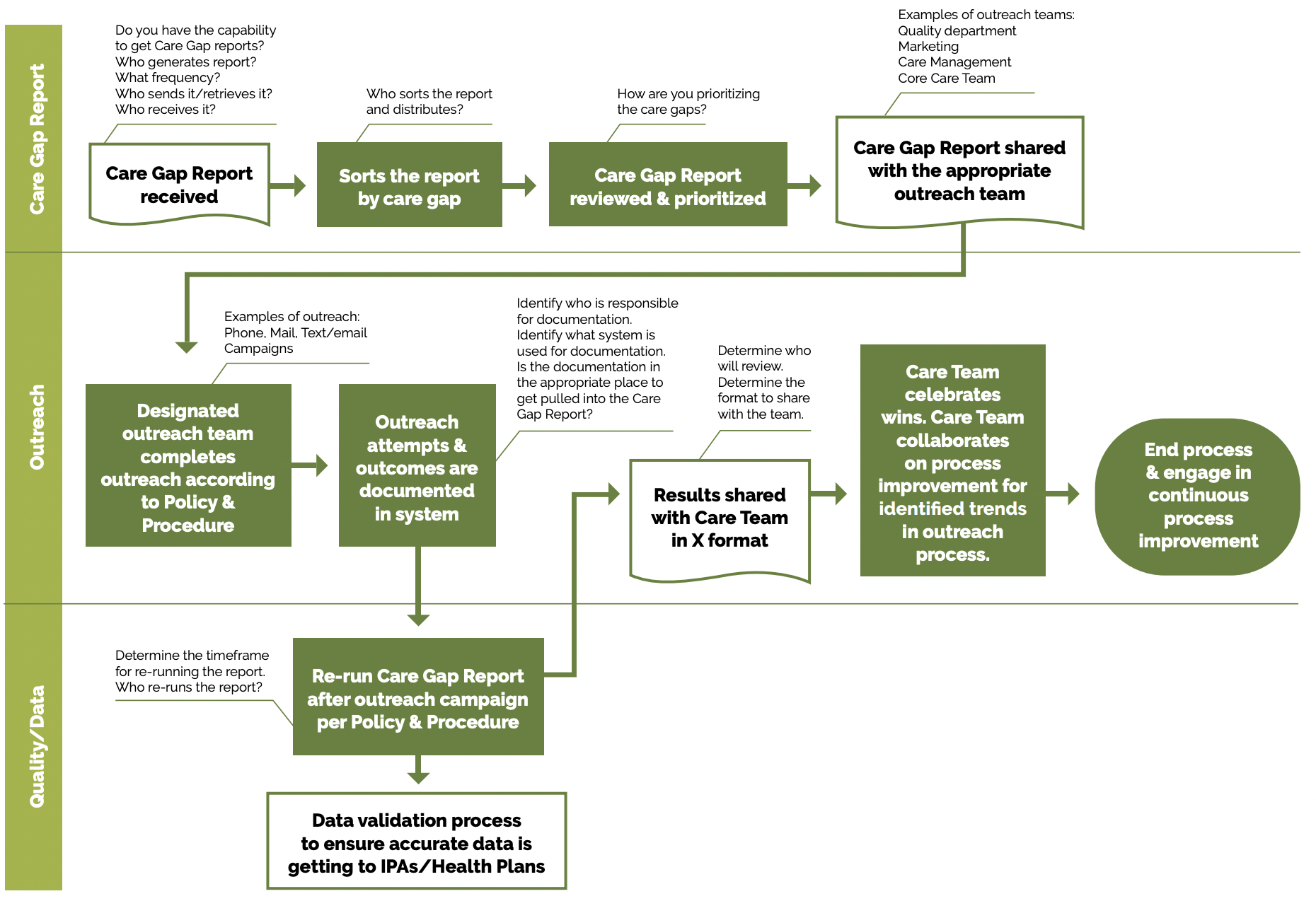
FIGURE 14: EXAMPLE OF PROACTIVE OUTREACH AND ENGAGEMENT
Peer example – outreach call script: San Francisco Health Network’s primary care provider visit call script for pediatric care. This script can be adapted or used to make outreach calls to schedule patient appointments.
Utilize multiple pathways to reach and engage patients. For example, a Swiss clinic used sequential appointment reminders consisting first of a phone call and, secondly, of an text massage, if patients did not answer the phone after three attempts. If the patient had no phone number listed, they received a reminder by mail two days prior to their appointment. The reminder system significantly reduced the rate of missed appointments and allowed the clinic to reallocate 28% of the canceled appointments.
Tip: Consider scheduling these outreached patients on days when you might experience a lower volume of activity in order to level the demand on the care team.
- Whether automated or manual, reminders should accommodate language requirements, as well as stated patient communication preferences (text, email, mail or phone). Reminders that include more than date, time and place and also include an orientation about what to expect and supporting clinical information may be more effective.[2]
4. Use touches that provide alternatives to the traditional office visit.
Suggested team member(s) responsible: IT staff, care coordinators, care team members.
Assess what types of interaction or care can be provided outside this setting and collaborate with patients as part of initial care planning to understand their preferences for communication and care team interactions. Examples include:
- Virtual visits with a provider or nurse.
- Group visits.
- Pharmacy visits.
- Digital communication through emails, texts and patient portals.
- Newsletters focusing on a specific condition.
- Social media that includes discussion groups relative to the management of conditions of focus.
- Home visits for high-risk, historically marginalized or mobility-challenged patients.
- Other technological solutions, such as apps focused on patient conditions which provide a vehicle for ongoing engagement.
5. Establish a process for engaging patients assigned to your practice by their managed care team who have not yet been seen by the practice.
Suggested team member(s) responsible: Multidisciplinary implementation team.
Depending on your agreement with the health plans, it is important for practices to make a proactive plan to build capacity to accommodate assigned-but-not-yet-seen patients in the clinic. Practices should develop strategies for outreach and engagement with these populations in order to shift them from not yet seen to fully engaged in primary care, as well as a process for not-yet-seen patients for whom outreach may be unsuccessful. These patients may be getting their pediatric care elsewhere though still assigned to the practice.
6. Continuously reassess outreach approaches with a goal of improvement.
Suggested team member(s) responsible: Community health workers, outreach workers and navigators, community partners.
- Test your co-designed outreach approaches and measure the effectiveness of your approaches. Review data (e.g., missed appointments, numbers lost to follow up, etc.).
- Survey patients to obtain retrospective and prospective feedback on outreach efforts.
- Regularly update outreach strategies based on community feedback and changing demographics.
Implementation tips
- Providing more intensive outreach: For high-risk patients or patients with complex health and social needs, consider care management as a more intensive approach for facilitating ongoing communication and coordination. See Key Activity 19: Provide Care Management for more information.
- Exploring one-time outreach efforts: Where there is a backlog of patients due to address a gap in care, consider a campaign where you bring in all patients due or overdue for similar screenings, labs or vaccines.
- Back to school: For children and adolescents, certain times of the year create predictable demands on clinics (e.g., back-to-school forms, sports clearance forms). Clinics can use proactive and frequent outreach to help manage these demands by encouraging early action by caregivers and families.
- Going deeper with community partners: For going deeper in this area, consider Key Activity 15: Strengthen Community Partnerships to provide outreach to others outside of your patient population. Community partners can support outreach and health literacy efforts, participate in co-design by providing insight around a particular patient population, and provide resources and supports for patients. Practices can provide education, interventions, outreach and programs in partnership with schools, local youth programming, churches, sports organizations, arts clubs, and other community organizations.
Examples from other organizations:
- West County Health Centers (WCHC) developed and refined workflows for WCVs and immunizations to improve efficiency and streamline outreach.
- The team created outreach lists for patients due for well-child visits using a Tableau dashboard based on claims and encounter information for ages three to six and patient-specific alerts in the EHR for children ages zero to three and over six years to create outreach lists for patients due. The front office staff conducts outreach (letters and calls) to these patients to schedule their well-child visits when due. Once an appointment is scheduled, the MA will conduct pre-visit planning chart preparation to determine and document what is due.
- A separate workflow for childhood immunizations outreach was led by the immunization coordinator. If a parent requests an exemption letter, an immunization committee comprised of medical directors follow guidelines to approve or decline the request and a standard form letter is completed. This process reduces pressure on the provider to approve exceptions when requested.
- Partnership Health Plan and Mountain Valleys Health Centers partnered to improve adolescent immunization rates. Some of the changes they tested included conducting adolescent immunization clinics early in the calendar year to allow for multiple doses required for measure compliance, distribution of gift cards, and accessing gap list members for focused outreach and more.
- Mountain Valleys Health Centers aimed to increase the rate of children and youth who complete WCVs. They tested grocery gift card incentives for completing WCVs and had population health advocate reached out by phone to 180 families to schedule visits alongside a social media campaign.
Endnotes
- McLean SM, Booth A, Gee M, Salway S, Cobb M, Bhanbhro S, Nancarrow SA. Appointment reminder systems are effective but not optimal: results of a systematic review and evidence synthesis employing realist principles. Patient Prefer Adherence. 2016 Apr 4;10:479-99. doi: 10.2147/PPA.S93046. PMID: 27110102; PMCID: PMC4831598.
- Perron NJ, Dao MD, Kossovsky MP, Miserez V, Chuard C, Calmy A, Gaspoz JM. Reduction of missed appointments at an urban primary care clinic: a randomised controlled study. BMC Fam Pract. 2010 Oct 25;11:79. doi: 10.1186/1471-2296-11-79. PMID: 20973950; PMCID: PMC2984453.