KEY ACTIVITY #21:
Provide Care Management
This key activity involves all seven elements of person-centered population-based care: operationalize clinical guidelines; proactive patient outreach and engagement; care coordination; behavioral health integration; address social needs.
Overview
What is care management? How does it differ from care coordination?
Led by a care manager (a licensed clinician or a non-licensed trained individual), care management is an intervention intended to support the highest-need individuals within your practice. The services are more focused, require the development of a person-centered care plan, and are of higher intensity than care coordination services. A patient must consent to participate in care management activities. A care manager works directly with the patient and multidisciplinary care team members to identify, plan and implement person-centered goals and care. The care manager supports the individual in identifying and coordinating resources and referrals as well as supporting self-management activities to attain optimal wellness.
Care management provides a higher level of support to individuals who have medical, behavioral health and/or social needs that impact their ability to access appropriate levels of care. Individuals may be receiving frequent emergency room and hospital care that could be avoided with care management activities, and/or patients may have significant social barriers (housing, food, substance use) that prevent them from accessing preventive and wellness care.
As part of care management, the patient’s medical, behavioral health and social health needs are directly addressed as part of their health assessment and prioritized according to the patient's goals. For example, supporting the patient's concerns around securing stable housing may be a first step to achieving better health. Addressing health-related social needs helps in reducing health inequities among different populations. Individuals with lower socioeconomic status or limited access to resources can be provided with resources to support these areas.
What type of patients are eligible for care management?
Individuals eligible for care management have high levels of need in one or more of the domains of medical, social or behavioral health. Some examples of populations who may be eligible for care management include:
- Individuals with complex medical needs (also known as complex care management).
- Example: a patient with congestive heart failure and advanced kidney disease with a history of frequent hospitalizations for shortness of breath.
- Goal of care management: support optimal diet and medication management to minimize hospitalization; address social needs that may impact the patient’s ability to manage their conditions, such as housing stability, food security, etc.
- Individuals who require intensive support after hospital discharge (care transitions).
- Example: a patient who had a stroke resulting in left-sided weakness and mobility issues. They will require additional support – including home nursing, physical therapy/occupational therapy, medical equipment and medication monitoring – as they make the transition to the home environment.
- Goal of care management: coordinate medications, medical equipment and follow-up care to support optimal recovery and minimize risk of rehospitalization.
CalAIM: ECM and Community Supports
In California, Medi-Cal beneficiaries who have high care management needs may be eligible for a Medi-Cal benefit known as Enhanced Care Management or ECM. ECM can be provided to eligible Medi-Cal beneficiaries at risk of poor outcomes due to high levels of medical, social and behavioral health needs. ECM delivers person-centered, trauma-informed care management services. Patients can also access additional services known as Community Supports to help achieve their medical and social health goals.
DHCS ECM and Community Supports[1] are foundational parts of the transformation of Medi-Cal, which focused on:
- Breaking down the traditional walls of healthcare, extending beyond hospitals and healthcare settings into communities.
- Introducing a better way to coordinate care.
- Providing high-need patients with in-person care management where they live.
If your practice has a lot of patients who are eligible for ECM (based on descriptions below), you can contact your Medi-Cal managed care plan (MCP). Your MCP can provide you with details on patient eligibility and the requirements needed to provide ECM services to your patients. Some clinics also provide Community Supports services depending on their patient population.
ECM is available to specific groups of Medi-Cal patients (called “ECM Populations of Focus”):[2]
- Adults, unaccompanied youth and children, and families experiencing homelessness.
- Adults, youth and children who are at risk for avoidable hospital or emergency department care.
- Adults, youth and children with serious mental health and/or Substance Use Disorder needs.
- Adults living in the community and at risk for long-term care institutionalization.
- Adult nursing facility residents transitioning to the community.
- Children and youth enrolled in California Children’s Services or its Whole Child Model with additional needs beyond their California Children’s Services condition(s).
- Children and youth involved in child welfare (foster care).
- Adults and youth who are transitioning from incarceration.
- Pregnant and postpartum individuals; birth equity population of focus (starting in 2024).
Medi-Cal patients can also be connected to Community Supports services to help address their health-related social needs, such as access to healthy foods or safe housing to help with recovery from an illness. If your clinic wants to provide Community Supports, contact your Medi-Cal managed care plan for information. Available Community Support Services include:
- Housing transition navigation services.
- Housing deposits.
- Housing tenancy and sustaining services.
- Short-term posthospitalization housing.
- Recuperative care (medical respite).
- Day habilitation programs.
- Caregiver respite services.
- Personal care and homemaker services.
- Nursing facility transition/diversion to assisted living facilities.
- Community transition services/nursing facility transition to a home.
- Environmental accessibility adaptations (home modifications).
- Medically tailored meals/medically supportive food.
- Sobering centers.
- Asthma remediation.
How does an eligible individual get connected to ECM and Community Supports services?
The Medi-Cal Managed Care health plans are responsible for identifying their patients who are candidates for ECM and meet eligibility requirements. In addition, practices, clinicians and community-based organizations have the ability to refer patients for ECM services. Community-based organizations, such as homeless services clinicians, are a particularly valuable source of referrals into ECM, as they often have trusted relationships with individuals who may not have sought or received medical care and are therefore not “known” to the MCP because they have had little or no utilization of healthcare services.
How do we refer a patient who we think would benefit from ECM?
If you have a patient who may be a candidate for ECM or Community Supports services, you should contact the Medi-Cal managed care plan to inquire about services available through the patient’s health plan.
Action steps and roles
How can we provide care management services, including ECM services, in our practice?
Community practices are often well situated to provide care management services as they are the site where patients seek or can be connected to care. Clinics may decide that they want to provide care management services, including ECM services. The following resources can help assess your capacity to provide care management services within your clinic structure.
Care management in primary care
This resource from AHRQ is a helpful guide when considering implementing a care management program. It addresses the following areas:
- What is care management and why would my practice want it?
- Selecting the right care manager and clarifying the care manager role.
- Training the care manager and practice team.
- Structuring care management.
- Implementation and sustainability issues: getting care management started and making it continue to work well.
- Resources.
- Data collection, management and analytics.
- Paying for care management.
- Evaluation: How is your care management program working?
Care management for complex populations
A resource on starting a care management program for individuals with multiple medical, behavioral health and social needs is available from the Camden Coalition. This resource addresses the following areas:
- Program design – tools to support the understanding and identification of a complex care population, plan a care model and workflow, and anticipate legal/business needs.
- Program operations – tools to support the implementation of a complex care model, including triage, outreach, engagement, intake and clinical support.
- Data and process improvement – tools to support metric identification, data collection and analysis, and process improvement.
- Team and leadership development – tools to support the recruitment, training and management of a complex care team.
- Community mapping and collaboration – tools to support multisector and community coordination.
- Communication and growth of success – tools to support broad communication and program scaling.
Care transitions
This Care Transitions Toolkit from the Indiana Patient Safety Center focuses on processes to support care management for individuals transitioning between healthcare settings.
ECM services
Aurrera Health Group’s Enhanced Care Management Provider Toolkit provides a detailed description of the services that are required to become an ECM clinician. In this guide, the requirements of ECM clinicians are outlined in detail.
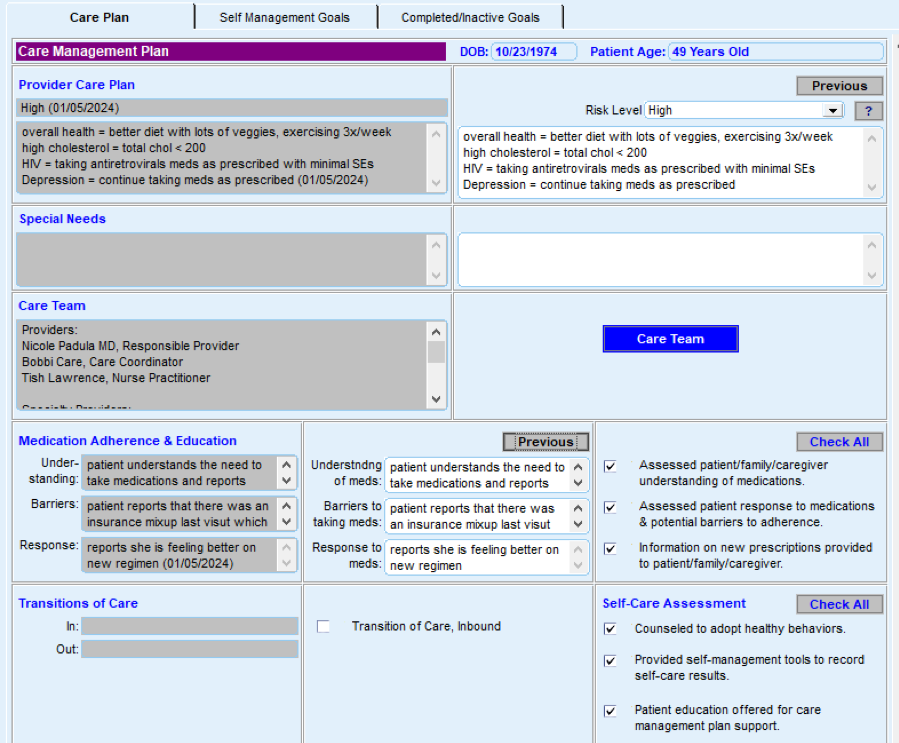
FIGURE 21: EXAMPLE OF HOW AN EHR CAN ASSIST WITH CARE MANAGEMENT
Resources
Evidence base for this activity
- Chuang E, Pourat N, Haley LA, O’Masta B, Albertson E, Lu C. Integrating Health And Human Services In California’s Whole Person Care Medicaid 1115 Waiver Demonstration. Health Affairs. 2020 Apr 1;39(4):639–48.
- Tomoaia-Cotisel A, Farrell TW, Solberg LI, Berry CA, Calman NS, Cronholm PF, et al. Implementation of Care Management: An Analysis of Recent AHRQ Research. Medical Care Research and Review. 2016 Oct 23;75(1):46–65.
Endnotes
- Enhanced Care Management and Community Supports [Internet]. [cited 2024 Jan 12]. Available from: https://www.dhcs.ca.gov/CalAIM/ECM/Pages/Home.aspx
- Medi-Cal Transformation: Enhanced Care Management [Internet]. DHCS; [cited 2024 Jan 12]. Available from: https://www.dhcs.ca.gov/CalAIM/Documents/CalAIM-ECM-a11y.pdf