KEY ACTIVITY #6:
Develop or Refine and Implement a Pre-Visit Planning Process
This key activity involves the following elements of person-centered population-based care: operationalize clinical guidelines; pre-visit planning and care gap reduction; care coordination; address social needs.
Overview
This activity provides guidance for how the care team can effectively and efficiently implement a pre-visit planning process (PVP).
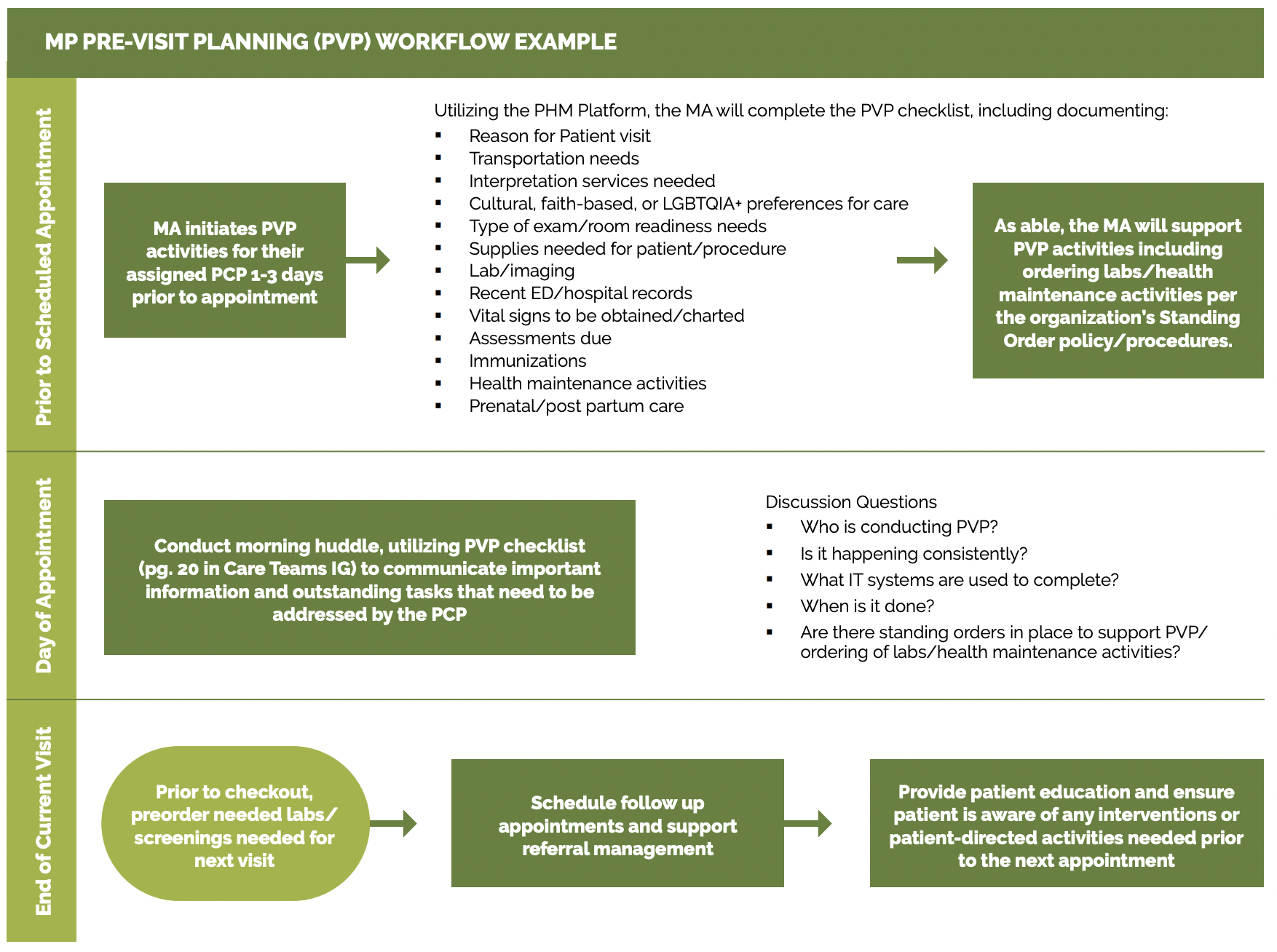
Pre-visit planning is typically driven by the medical assistant with help from other care team members and includes steps taken:
- At the end of the current visit to ensure the patient understands any actions they need to take and to schedule for any follow-up.
- Prior to a scheduled appointment, to “scrub” the chart and identify any pre-visit tasks per the pre-visit checklist.
- The day of an appointment, during the daily huddle and before the patient sees the obstetric provider.
The average prenatal care visit at California practices lasts just 10 to 15 minutes, and many patients come to these visits with multiple needs. Pre-visit planning works towards optimizing a team-based approach so patients receive comprehensive care in alignment with the latest clinical guidelines and their own needs and preferences.
Pre-visit planning allows for better coordination of care. This can be particularly beneficial for patients with complex, higher risk pregnancies, ensuring they receive comprehensive and equitable care. As your practice works to reduce any identified equity gaps, pre-visit planning is often a powerful activity for ensuring relevant care as the care team partners with the patient to discuss important screening or testing due at the time of the visit.
The PVP should incorporate your practice’s process for screening and responding to social needs, including checking whether social needs screening is due. When social needs are identified the team should be clear on the pathways, both during and after visits, to address and follow up on those needs.
Pre-visit planning draws upon similar technical enablers as care gap reporting, and likewise can be facilitated at the individual patient level and at the level of groups of patients coming for care by a specific team in an appointment schedule block. The format in which planning is done needs to consider the workflow and staffing model.
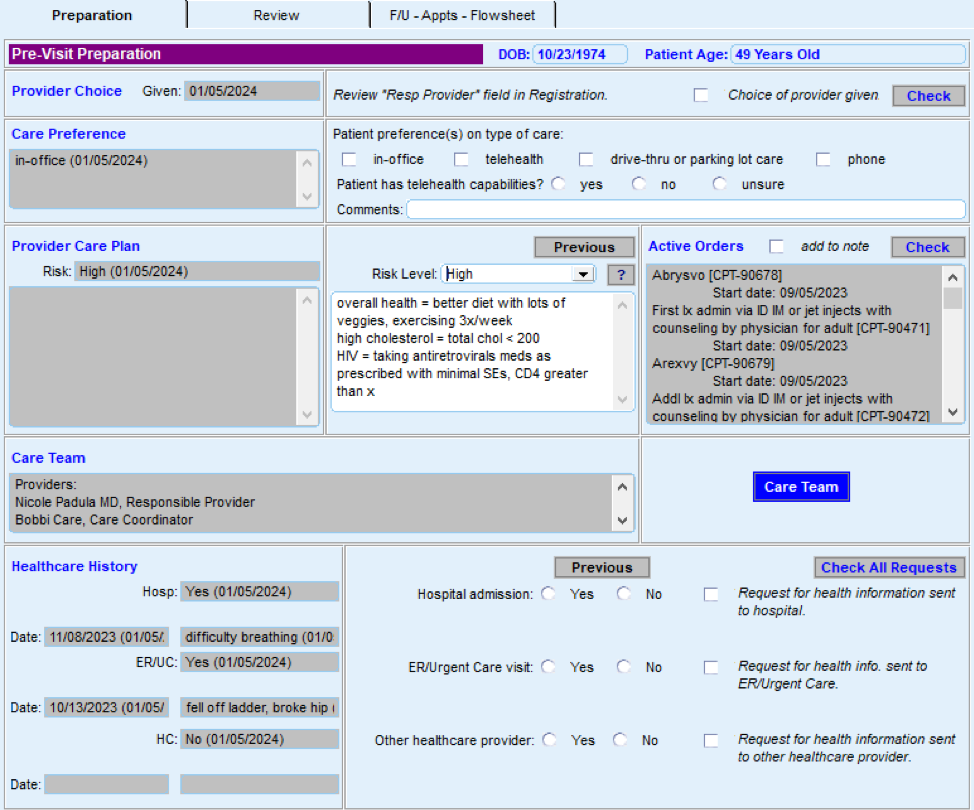
Individual patient level pre-visit planning would optimally be enabled within the EHR, provided the EHR is able to store relevant information such as assessments, plans, orders and notes outside of a visit note. Pre-visit planning might also include use of patient-facing applications such as portal reminders, questionnaires and self-completed screenings and assessments, which ideally would be available to the provider and care team in the EHR.
Engagement of the expanded care team in pre-visit planning requires access by all relevant members of the care team to contribute to and view relevant information. This may require coordination with technology additional to the EHR, such as care coordination and population management applications where relevant information might be stored.
Huddle reports, in which individual patient information can be visualized in summary views across all patients within a session, can require use of technology outside the EHR, but might also be supported by developing reports populated by data from the EHR. Ideally, internal practice and EHR data should be supplemented with external data where such information completes the patient’s current status. Establish access to local hospital systems to obtain prior pregnancy and delivery records. Standardize where these records are inputted into the EHR. If such electronic access is not possible, workflow should include manual reconciliation by history from the patient. Relevant HIT capabilities to support this activity include prenatal care guidelines, registries, clinical decision support, care dashboards and reports, outreach and engagement, and care management and care coordination.
See Appendix D: Guidance on Technological Interventions.
FIGURE 12: AN EXAMPLE OF HOW TECHNOLOGY CAN HELP WITH PRE-VISIT PLANNING
Action steps and roles
1. Assess the current state of the pre-visit planning (PVP) process across your practice.
Suggested team member(s) responsible: Implementation team or QI team.
Understand how the process currently works for prenatal and postpartum care in light of your practice’s performance on core and supplemental measures. Compile existing paperwork and process documentation into one place and talk to medical assistants and other members of the care team to understand their questions and challenges around the pre-visit planning process.
Consider making current-state process maps that communicate the major steps in the PVP process and acknowledge pain points or challenges in the process. Pain points are places where the process isn’t working well for patients, staff or specific subpopulations or demographic groups for which your data analysis has revealed equity gaps. In addition, pay attention to places where staff are creating workarounds to the process. The presence of workarounds indicate that the process might need further clarification or refinement to support the care team to reliably implement it.
Your team may find it helpful to compile process maps for both the high-level pre-visit planning as detailed in Figure 13 in addition to more detailed documentation for specific clinical workflows.
FIGURE 13: PRE--VISIT PLANNING (PVP) WORKFLOW EXAMPLE
2. Identify where to update the PVP process to more consistently and reliably address care gaps.
Suggested team member(s) responsible: Implementation team or QI team. May include the data manager to assist with identifying patients through EHRs.
Examine where you can further incorporate or streamline your practice’s clinical protocols and standing orders into PVP, including via the PVP checklist, daily huddles and other key clinical workflows. Examples and considerations for updating the PVP process are included below.
Patient provider continuity is associated with better patient and provider satisfaction. Determine if the PVP process can be leveraged to improve provider continuity for perinatal patients.
Clinical guidelines and care gaps: Consider which preventive and maintenance services could be addressed more reliably using PVP, including those in your EHR’s care gap module. The Pre-Visit Planning: Leveraging the Team to Identify and Address Gaps in Care resource provides a more complete list of preventive services for adults and children.
PVP checklist: A generic PVP checklist to be completed by the MA or licensed vocational nurse (LVN) at least one to three days before the appointment is provided in Figure 14. Most EHRs will have a health maintenance module that identifies what preventive care is due, but a printed or digital checklist provides a starting point for ensuring key steps aren’t missed. For prenatal or postpartum care, the PVP checklist should include checklist items directly relevant to obstetric services. One approach is to create trimester-specific checklists to guide the MA or LVN in identifying key information.
FIGURE 14: PRENATAL AND POSTPARTUM PVP PLANNING CHECKLIST
Checklist Domain |
Checklist Item |
|---|---|
General |
|
Room readiness |
|
Pregnancy history and current problem list |
|
Medical record review |
|
Assessments needed |
|
Care gaps |
|
For postpartum visits |
|
Daily huddles: Design or redesign the team’s daily huddle so the care team can review prioritized action items for the list of patients scheduled to come and any further follow-up for patients seen in the previous days. For more information, see the Care Team and Workforce Guide Resource 4: Daily Huddles Overview and Process.
The Center for Excellence in Primary Care resource on healthy huddles includes tools, a video and examples around how pre-visit planning flows into the daily huddle process, including a healthy huddle warm-up, which can help MAs prepare for huddles.
Patients requiring special considerations: Ensure that the PVP includes a process to flag for the care team:
- Patients requiring special attention, such as those with:
- Chronic conditions impacting their pregnancy.
- Conditions that require increased coordination with specialty care or other services (e.g., patients with gestational diabetes).
- Complex psychosocial needs.
- Recent hospitalizations.
- Patients who need extended time or additional services during their visit (e.g., translation services, mobility assistance, screenings).
Detailed clinical workflows: Clinical workflows should be updated to describe at which step in PVP or the patient visit a care team member will address a specific gap in care with the patient. This may include the following details:
- Who will initiate the discussion with the patient based on the needs (e.g. preferred language) and preferences of the patient.
- How and when the care team member will plan to have the discussion before, during or after the visit.
- How they will be prepared to address common barriers or concerns the patient may have.
- Educational materials available for use that are relevant to the patient.
Planning for care after the visit: Effective PVP includes scheduling pre-visit labs and other diagnostics at the end of the current visit and coordinating care and referrals for services not available at the practice. See Key Activity 13: Coordinate Care for more information. Confirm the patient understands the purpose of any follow-up care.
The American Medical Association (AMA) has an online guide for implementing pre-visit planning, which includes forms, templates and other resources.
3. Test planned changes to the PVP workflows and support care teams in implementing the workflow.
Suggested team member(s) responsible: Implementation team or QI team.
Test and refine important changes to the PVP process with one or two care teams before considering rolling out the change more broadly at the practice.
Implementing the change includes updating documentation and creating a staff training schedule or training refresher for staff to sustain workflow changes. For example, train MAs every six months on the PVP. If they have difficulty, have them retake training with a different highly effective MA and monitor closely until competency in the task is reached.
For further streamlining of the process, practices can customize EHR templates to align with PVP workflows. Be sure to account for potential costs associated with creating new templates, staff training and IT.
4. Establish a process to review and update PVP workflow.
Suggested team member(s) responsible: Care team with quality improvement manager.
Identify staff responsible for reviewing and updating the PVP process at least annually to incorporate the latest clinical guidelines and check for any workarounds that have developed.