KEY ACTIVITY #11:
Provide or Arrange for Cancer Screening
This key activity involves the following elements of person-centered population-based care: operationalize clinical guidelines; pre-visit planning and care gap reduction; care coordination.
Overview
This activity provides guidance for setting up a cancer screening test for colorectal cancer, breast cancer and/or cervical cancer for any patient eligible and due for screening who agrees to complete the recommended screening. This includes patients who agree to get screened during a patient visit, in response to a screening reminder, or in response to an outreach activity. This includes guidance on the following screening methods:
- Screening at the practice.
- Providing screening materials during the visit to take at home.
- Providing screening modalities outside of the practice (e.g., mailed FIT, self-referred mammogram, or setting up an appointment for colonoscopy).
- Utilizing community linkages for screening (e.g., providing patients with contact to a mammography center or an outpatient surgical center for colonoscopy or sigmoidoscopy).
This activity includes tailored messaging and a choice in screening modalities, where feasible, to increase the likelihood that populations who have historically had lower cancer screening rates, higher rates of certain cancers and/or higher mortality rates, complete the recommended screening. Initiating a screening recommendation provides an opportunity for a dialogue with patients that may uncover barriers to beliefs about screening and the ability and interest in undergoing screening, including the opportunity to identify unmet social needs that are a barrier to getting screened. Our guidance for this activity, therefore, includes assessing social needs and addressing them.
As discussed in Key Activity 3: Use Care Gap Reports or Registries to Identify All Patients Due for Cancer Screening, Key Activity 6: Conduct Proactive Outreach to Patients Due for Screening, and Key Activity 8: Refine and Implement a Pre-Visit Planning Process, technology can support care teams in their efforts to address cancer screening. Each modality will draw upon similar technical enablers to facilitate cancer screening for adults. The format in which planning is done needs to consider the workflow and staffing model.
Also, as discussed elsewhere, linkage to other sources of screening or follow-up is ideally facilitated by direct data connection to EHR and care coordination applications to support referral and follow-up, but where this is not possible a more manual process ought to be accompanied by a registry like function. (See the next section.) Relevant HIT capabilities to support this activity include care guidelines, registries, clinical decision-making support, care dashboards and reports, outreach and engagement, and care management and care coordination.
Action steps and roles
1. Plan for the cancer screening.
Suggested team member(s) responsible: Multidisciplinary team for cancer screening.
Planning and preparation are covered in the following key activities:
- Key Activity 2: Develop or Update the Practice’s Cancer Screening Protocols.
- Key Activity 3: Use Care Gap Reports or Registries to Identify All Patients Due for Cancer Screening.
- Key Activity 5: Develop and Implement Standing Orders.
- Key Activity 8: Refine and Implement a Pre-Visit Planning Process.
- Key Activity 9: Partner with Patients to Discuss Cancer Screening During Patient Visits.
2. Provide or arrange for the selected cancer screening.
Suggested team member(s) responsible: Designated care team member, based upon the test and the practice’s standing orders.
This is always based on your practice’s clinical practice guidelines and cancer screening protocols (See Key Activity 2: Develop or Update the Practice’s Cancer Screening Protocols).
- Based upon the screening indicated and the option selected by the patient, if choices are available, the appropriate care team member will implement the practice’s cancer screening protocol and standing orders.
- If the selected screening test can be done during the visit, the clinician will implement the screening process, such as a Pap smear or fecal testing.
- If the selected screening procedure is to be conducted by the patient at home using a self-collected sample (e.g., FIT kit), the clinician will explain and demonstrate the proper collection techniques and the process to return the specimen for testing.
- If the screening requires further appointments (e.g., mammogram, colonoscopy, Pap Smear), the medical assistant or appropriate care team member may schedule the patient in the practice or initiate the referral, per protocol, and schedule the necessary follow-up appointments or provide referrals using preestablished community linkages.
- If the screening test requires laboratory analysis (e.g., Pap smear, fecal testing), the clinician will explain when the patient can expect to receive the results and what to do next.
3. Document the screening.
Suggested team member(s) responsible: Medical assistant.
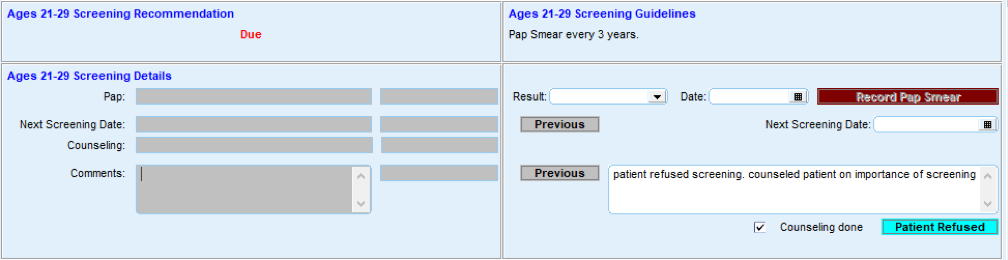
The medical assistant documents the cancer screening test(s) selected, including test type(s), date(s), and any relevant notes, in the patient's electronic health record (EHR).
FIGURE 19: EXAMPLE OF SCREENING DOCUMENTATION
4. Conduct ongoing quality assurance of the cancer screening process.
Suggested team member(s) responsible: QI lead or their designee(s).
The QI lead or their designee(s) should develop and implement a process to review a subset of records each month to ensure that this practice is in compliance with the practice’s cancer screening protocols, standing orders and any other of the practice’s relevant policies and procedures. In cases where policies and procedures are not being followed, the QI lead should initiate corrective action.
Sample workflow for colorectal cancer screen using FIT test
- Assure that the patient is eligible for fecal-based testing by referencing your organization’s screening protocols outlined in Key Activity 2: Develop or Update the Practice’s Cancer Screening Protocols.
- Provide culturally and linguistically appropriate education materials and decision aides to the patient to ensure that they understand the benefits, risks and follow-up schedule for fecal-based testing (see Key Activity 10: Use Culturally Appropriate Education Materials for Cancer Screening). Best practices include:
- Informing patients about the ability of different tests to detect colon cancer.
- Noting the frequency of each test type.
- Providing the patient with testing materials and instructions for the test of choice.
- Highlighting the time frame to return the sample.
- If the patient is available on site, review the sample procurement technique, return system and time frame with the patient while at the practice.
- Using culturally and linguistically appropriate materials and providing graphic diagrams where possible.
- If the patient is receiving the testing materials by mail, provide culturally and linguistically appropriate educational materials with an emphasis on graphic instructions and include information and materials for returning the test to the practice. Invite the patient to contact a specific person at the practice, if they have any questions.
- Document the delivery of materials for testing in the EHR.
- Process the sample or send the sample for processing within 24 hours of receipt and record the results in the EHR.
- Document results and instructions in the EHR. Assure that the EHR cancer screening report notes the patient as having received a fecal-based test in order for the eligibility roster to be generated in accordance with the USPSTF testing frequency guidelines.
- Contact the patient to inform them of the test results and the recommended follow-up (see Key Activity 12: Develop and Implement a Follow-Up System for Those Who Have Been Screened).
- If the patient cannot be reached to communicate positive test results, the team should design and implement alternative methods to reach patients, such as deploying community health workers to attempt to reach the patient and/or sending written communications.
Sample workflow for use of a mobile Pap screening clinic
- Front office staff contact the patient by phone or in person to establish an appointment for a Pap smear and affirm the patient’s knowledge that the appointment is for the mobile unit. The front office staff confirm the patient’s understanding of the date and location of the appointment and how the mobile unit can be identified.
- Front office staff send the patient confirmation of the appointment by mail or text message with the date, time, and location and a reminder of the appearance of the mobile unit. They provide a number to call for questions or changes ahead of the appointment.
- The front office staff or mobile unit staff confirm the patient’s availability by text message the day before the appointment.
- At the mobile unit site, the clinical support personnel, such as an MA, greet the patient and invite the patient to enter the unit for pre-visit information gathering and confirmation of the appointment purpose and prepare the patient for the exam.
- The clinician conducts the exam, secures a Pap Smear, and addresses other clinical needs of the patient.
- The clinician and/or clinical support inform the patient of when the result is expected and how the patient will be informed of the result.
Tips
- Where applicable, it is critically important to guide the patient in how to obtain and return the sample based on the type of test selected. Timing of the sample’s return is of the greatest importance and going outside the return time frame may render a sample to be invalid.
- Where multiple test modalities are offered, be sure to note the frequency of retesting, based on the method selected by the patient.
- Work with community representatives to develop messages and tools that are culturally relevant and understandable by the population.
- Test the message with community members to assure relevance and cultural accuracy.
- Review the use of the testing materials while the patient is in the practice, if possible, and encourage them to ask questions and review the testing and return technique.
- Encourage patients to complete the test in a brief time frame so that it remains top of mind.
- See also Appendix D: Peer Examples and Stories from the Field to learn about how others are implementing this activity.