PHMI Equity Framework and Approach
©️ 2024 Kaiser Foundation Health Plan, Inc.
This brief outlines an approach and underlying framework for use by the Practice Transformation (PT) Partners and participating Community Health Centers (CHCs) to center equity in the Population Health Management Initiative (PHMI). The approach includes feedback from Kaiser Permanente, the California Department of Health Care Services (DHCS) and other stakeholders involved in PHMI.
It serves as a basis for the curriculum materials and Learning Action Network (LAN) activities that are being developed and implemented by the PT Partners.
A. Working Definitions
For the purposes of this work, we will use the following definitions:
- Health equity: Everyone has a fair and just opportunity to be as healthy as possible. To achieve this, we must remove obstacles to health, such as poverty, discrimination and deep power imbalances.[1]
- Racial equity: As an outcome, we achieve racial equity when race no longer determines socioeconomic outcomes or the quality of protection of human rights. As a process, we apply racial equity when those most impacted by structural racial inequity are meaningfully involved in the creation and implementation of the institutional policies and practices that impact their lives.[2]
- Inequities: Differences or disparities between people or groups that are systematic, avoidable and unjust.[3]
- Implicit bias: The attitudes or stereotypes that affect our understanding, actions and decisions in an unconscious manner. These biases, which encompass both favorable and unfavorable assessments, are activated involuntarily and without an individual’s awareness or intentional control.[4]
Please note that to align with more recent equity nomenclature, the term “health-related social needs” is used instead of “social determinants of health” and the term “inequities” is used instead of “disparities” throughout most of this brief. The two former terms are still used in sections A and B because the working definitions and frameworks we reviewed utilize them.
B. Framework Development
Many frameworks that center the needs of communities being served have been developed both in California and across the United States to inform equity work within healthcare settings. Within this existing body of work, we reviewed the five equity frameworks below to guide the creation of a draft PHMI Equity Framework:
- Dr. Marshall Chin’s Framework for Advancing Health Equity.[5]
- The Institute of Healthcare Improvement’s (IHI’s) Framework for Health Care Organizations to Achieve Health Equity.[6]
- IHI’s Community of Solutions Framework.[7]
- The DHCS’ Framework for Health Equity.[8]
- The California Improvement Network (CIN), its Racial Health Equity Workgroup, and HealthBegins’ “ A Toolkit to Advance Racial Equity in Primary Care Improvement.”[9]
An overview of each equity framework is included below.
Dr. Marshall Chin’s Framework for Advancing Health Equity
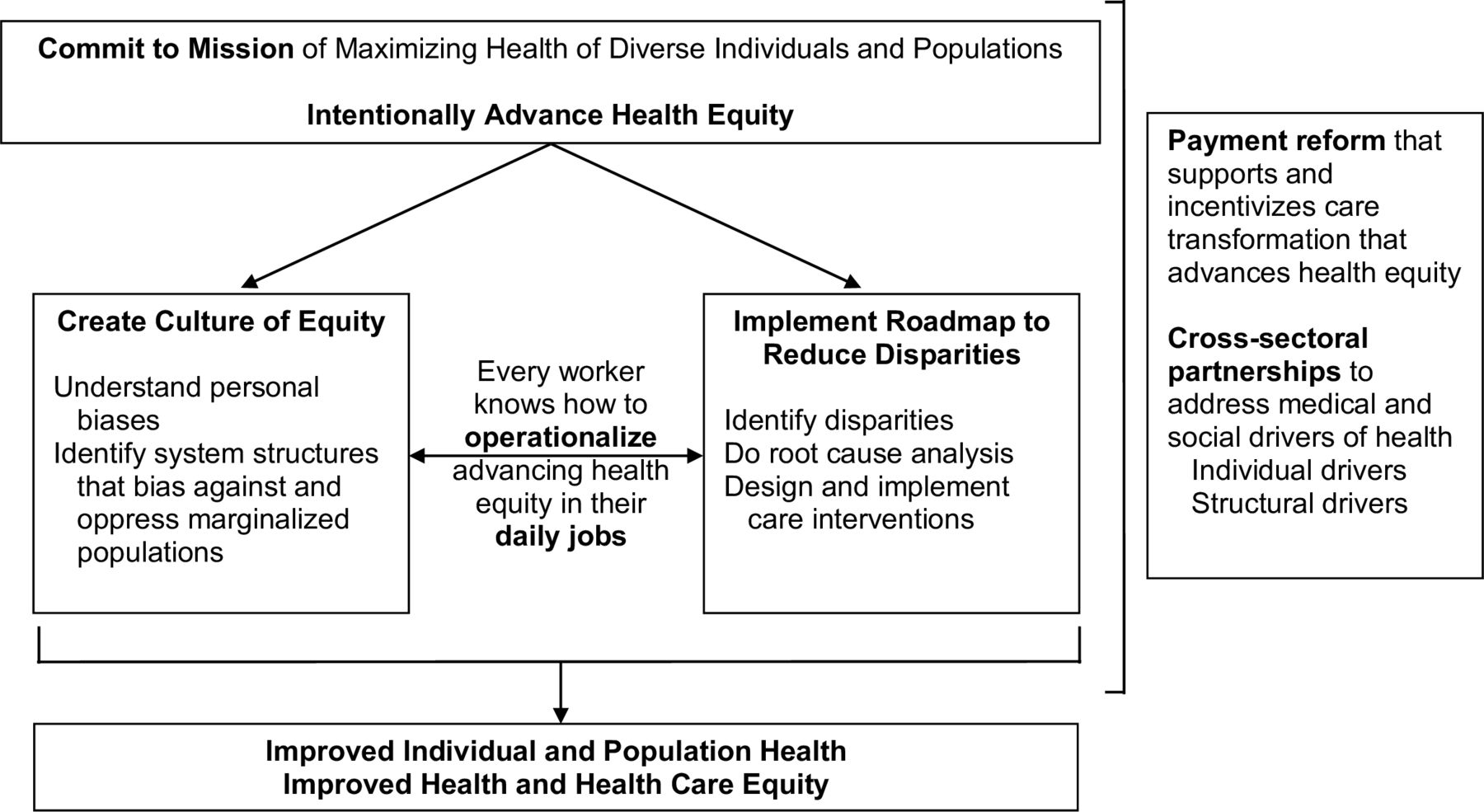
Reprinted from BMJ Quality & Safety, 2021.
The goal of this framework is that “individuals and organizations commit to the mission of maximizing the health of diverse individuals and populations.” There are two simultaneous tracks for this:
- Create a culture of equity in which the whole organization buys into the mission. This requires understanding personal biases and identifying systemic structures that oppress marginalized groups.
- Implement a road map to identify and reduce disparities by collecting data and input, conducting a root cause analysis and implementing care interventions that address the root causes.
IHI’s Framework for Achieving Health Equity

Reprinted from “Achieving Health Equity: A Guide for Health Care Organizations,” 2016.
This IHI framework informs healthcare organizations on how to reduce health disparities related to characteristics historically linked to discrimination. The five key components of this framework are listed below:
- Make equity a strategic priority: Demonstrate leadership commitment to improving equity
at all levels of the organization. - Build infrastructure to support health equity: Establish a governance committee to oversee and manage equity work across the organization. Dedicate resources in the budget to support equity work.
- Address multiple determinants of health: Focus on healthcare services, socioeconomic status, physical environment and healthy behaviors.
- Eliminate racism and other forms of oppression: Reduce implicit bias within organizational policies, structures, norms and inpatient care.
- Partner with the community: Leverage community assets to work together on community issues related to improving health and equity.
IHI’s Community of Solutions Framework

Reprinted from “100 Million Healthier Lives: Case Studies From Around the Globe,” 2020.
IHI’s Community of Solutions Framework focuses on the capabilities, skills and behaviors needed to achieve an equitable environment. These include:
- Leading from within: Develop one’s inner journey as a leader by reflecting, learning from mistakes and valuing differences.
- Leading together: Perceive the community as a dynamic network of interacting people, organizations, structures and systems that are related to a place.
- Leading for outcomes: Support communities in applying the range of skills needed to achieve equity. These skills can include systems thinking, design thinking, sciences of improvement and implementation skills.
- Leading for equity: Apply the three previous skills with a lens toward equity.
- Leading for sustainability: Develop an ongoing process of transformation within a community as opposed to maintaining programs as they are.
Department of Health Care Services’ (DHCS) Framework for Health Equity

Reprinted from “Comprehensive Quality Strategy,” 2022.
This framework focuses on three primary domains, which are listed below:
- Data collection and stratification: Complete and accurate data on Medi-Cal patients’ race, ethnicity, disability, language, and sexual orientation and gender identity (SOGI) will be utilized to illuminate and address healthcare inequities across DHCS programs.
- Workforce diversity and cultural responsiveness: The Medi-Cal workforce, at all levels, should reflect the diversity of the Medi-Cal population. It also should always provide culturally and linguistically appropriate care.
- Elimination of healthcare disparities: Support policy efforts to eliminate disparities, driven by social drivers of health, between Medi-Cal members and commercial or other Medicaid populations.
CIN & HealthBegins’ Toolkit to Advance Racial Equity in Primary Care Improvement

Reprinted from “A Toolkit to Advance Racial Health Equity in Primary Care Improvement,” 2022.
This toolkit is designed to help those who provide, pay for or support primary care to translate their commitment to racial health equity into reality. It includes a road map (listed below) to reach an equitable, high-quality primary care practice. The toolkit also mentions that shared understanding, norms and commitment to becoming a multicultural, anti-racist organization are foundational to this work.
- Organize teams: Form and revise improvement teams dedicated to incorporating racial health equity in care improvement
- Collect data on race, ethnicity and language: Collect race, ethnicity and language (REAL) data from all patients, align reporting with emerging standards, and focus on strategies to improve collection of direct self-identified race/ethnicity
- Identify measures to stratify by REAL data: Choose performance measures to disaggregate and stratify using REAL data, including clinical performance and patient experience
- Analyze and identify root causes of identified inequities: Engage key stakeholders, patients and community members to review inequities in care and outcomes; use additional data as filters to better define patterns of inequity; and identify potential root causes of these
- Identify and collaboratively design improvement efforts: Collaboratively design improvement efforts with key stakeholders, patients and community members to incorporate and advance racial health equity in primary care
- Guide and monitor improvement efforts: Develop or update performance dashboards to guide and monitor racial health equity-focused care improvement
- Inform and accelerate institutional transformation and community action: Learn from and leverage equity-focused care improvement efforts to identify barriers, inform institutional transformation and accelerate community action to advance racial health equity.
*HealthBegins has also created the Compass for Health Equity Transformation tool, which provides “a practical and rigorous approach to the design and management of a portfolio of multi-level interventions.”[10]
C. Crosswalk of Frameworks
After reviewing each framework, we conducted a crosswalk analysis to identify similar themes among four of the five frameworks. The crosswalk looked at how the frameworks’ domains and strategies for making equity-related changes at the organizational and ecosystem levels aligned or did not align with one another (see Table 2). Creating the crosswalk assisted in determining the main themes to incorporate into our proposed PHMI Equity Framework and Approach. The main themes are:
- Commit to equity as an organization and make it a strategic priority.
- Build capacity to support health equity work.
- Understand and address internalized, personally mediated and institutionalized racism.[11]
- Promote workforce diversity.
- Partner with community and other value-aligned organizations.
- Build data infrastructure, and collect and analyze accurate REAL, SOGI and other sociodemographic data, including income, age and geographic data.
- Address and eliminate healthcare inequities identified by the data.
FIGURE 1. FRAMEWORK CROSSWALK
Themes |
Dr. Chin’s Framework for Advancing Health Equity |
IHI’s Framework for Achieving Health Equity |
DHCS Framework for Health Equity |
A Toolkit to Advancing Racial Equity |
|---|---|---|---|---|
Commit to equity as an organization and make it a strategic priority. |
Commit to mission of maximizing the health of diverse individuals and populations. |
Make equity a strategic priority:
|
See “Getting Grounded” section in Toolkit and Associated Resources. |
|
Build capacity to support health equity work. |
Build infrastructure to support health equity:
|
Organize teams:
|
||
Understand and address internalized, person- mediated and institutional racism. |
Create culture of equity:
|
Eliminate racism and other forms of oppression:
|
Promote Workforce diversity and cultural responsiveness:
Eliminate health disparities:
|
Analyze and identify root causes of identified inequities:
|
Promote workforce diversity. |
Eliminate racism and other forms of oppression:
|
Eliminate racism and other forms of oppression:
|
||
Partner with community and other value-aligned organizations. |
Implement road map to reduce disparities:
|
Partner with the community:
|
Identify and collaboratively design improvement efforts:
|
Inform and accelerate institutional transformation and community action:
|
Build data infrastructure, and collect and analyze accurate REAL, SOGI and other sociodemographic data, including income, age and geographic data. |
Implement road map to reduce disparities:
|
Build infrastructure to support health equity:
|
Improve data collection and stratification:
|
Collect data on race, ethnicity and language:
Identify measures to stratify REAL data:
|
Address and eliminate healthcare inequities identified by the data. |
Implement road map to reduce disparities:
Build Cross-sectoral partnerships to address medical and social drivers of health:
|
Address multiple determinants of health:
|
Eliminate healthcare disparities:
|
Identify and collaboratively design improvement efforts:
Guide and monitor improvement efforts:
|
D. PHMI Equity Framework
Based on the crosswalk, we determined three priority domains, which encompass the themes above, for CHCs to consider as they continue to build on their existing equity work. These domains are to reduce inequities for populations of focus (PoF), create a culture of equity, and build and strengthen cross-sectoral partnerships (see Figure 2).
FIGURE 2: DOMAINS FROM CROSSWALK
Domains |
Themes from Crosswalk |
|---|---|
Reduce inequities for populations of focus. |
|
Create a culture of equity. |
|
Build and strengthen cross- sectoral partnerships. |
|
Dr. Marshall Chin’s Framework for Advancing Health Equity, the DHCS’ Framework for Health Equity, IHI’s Framework for Achieving Health Equity and CIN and HealthBegins’ Toolkit to Advance Racial Equity all provide specific strategies and actions for CHCs to implement to center equity in their population health management efforts; such work can lead to the aim of reducing health inequities. IHI’s Community of Solutions Framework supports these strategies and actions by focusing on the capabilities, behaviors and skills of leaders within the organization to commit to equity and allocate the needed resources to implement and sustain determined milestones to contribute to the overall aim.
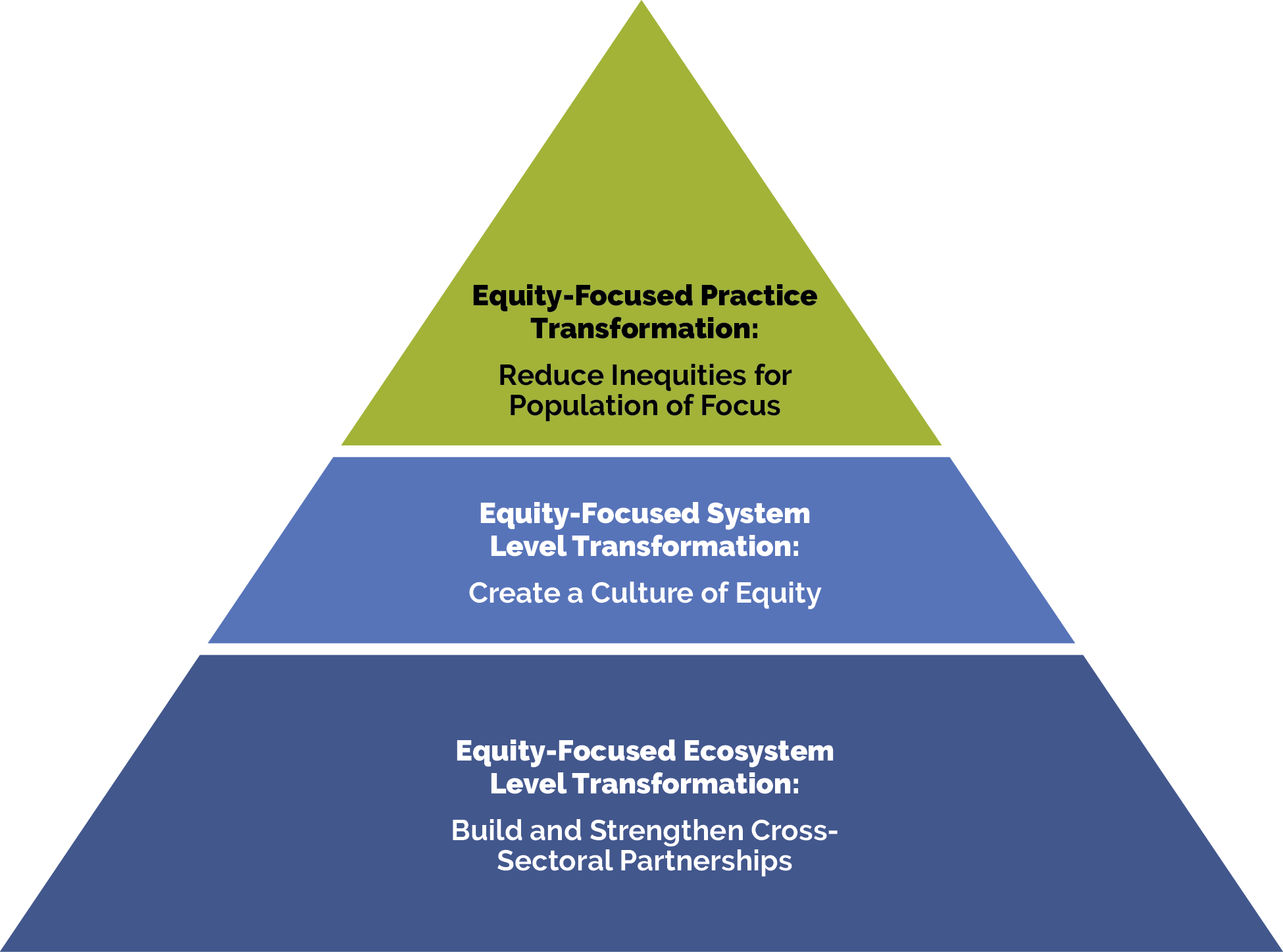
The priority domains that CHCs can work on have been categorized into three levels of equity- focused transformation: (1) equity-focused practice transformation, (2) equity-focused system-level transformation and (3) equity-focused ecosystem-level transformation (represented in Figure 3).10 The first level falls within the “reduce inequities for populations of focus” domain, and levels two and three are included within the “create a culture of equity” and “build and strengthen cross-sectoral partnerships” domains.
FIGURE 3: EQUITY-FOCUSED MAP
The PT Partners are including these efforts within the curriculum tools and resources. They also will support CHCs in implementing them through the Learning Action Network (LAN) activities, including coaching and peer-learning activities, collaborating closely with existing efforts led by regional consortia and the California Primary Care Association (CPCA). It is important to keep in mind that equity work is a journey and every health center will be at a different point in this journey. The driver diagram in Figure 4 below illustrates the priority domains as the “primary drivers” and includes actions CHCs can take as the “secondary drivers” to further their equity work and contribute to the overall aim.
FIGURE 4: PHMI EQUITY DRIVER DIAGRAM
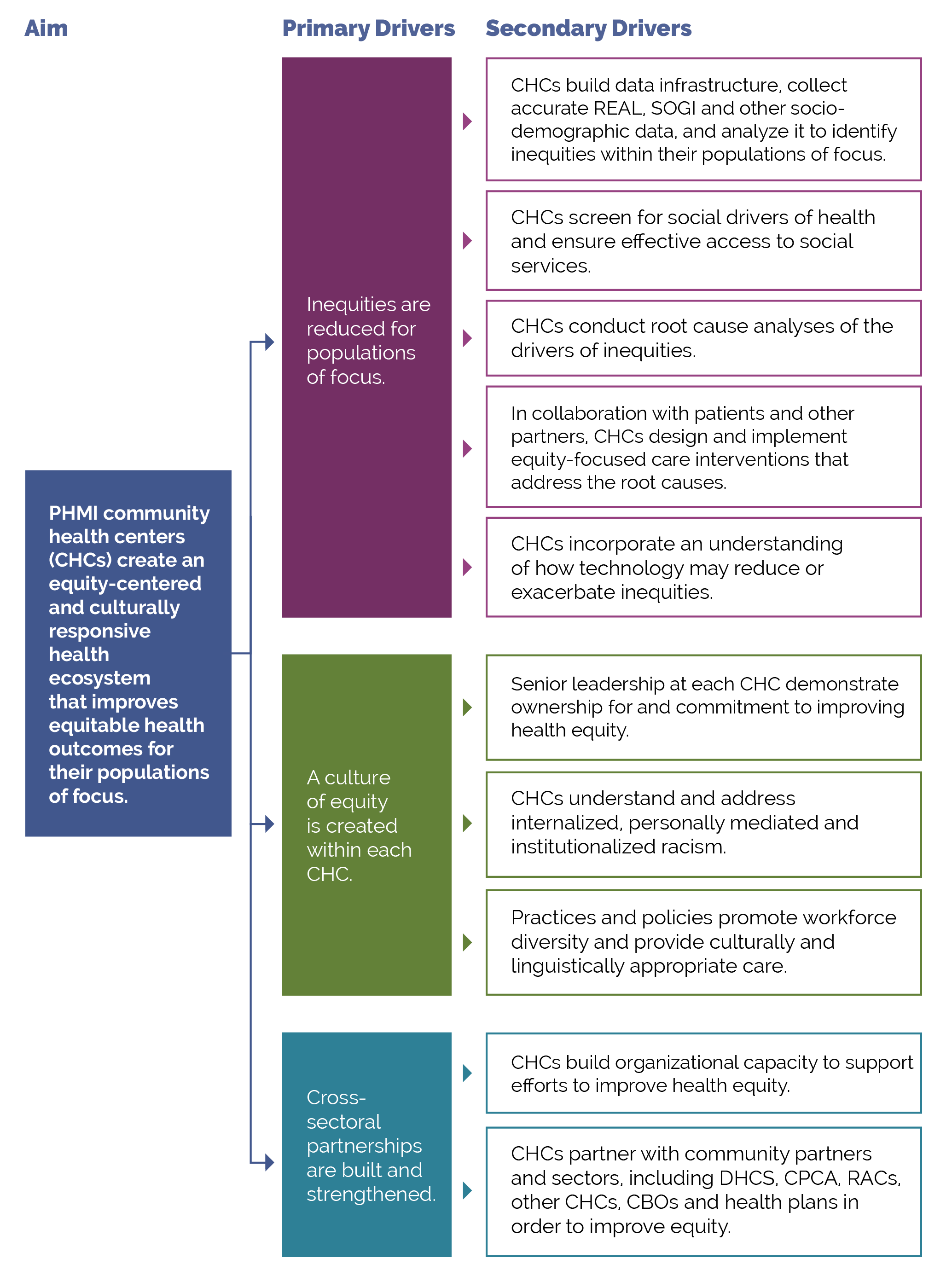
*The overarching goal is to eliminate inequities for populations of focus, but given the time frame of PHMI, the term “reduce” is being utilized instead of “eliminate.”
For each of the secondary drivers, Figure 5 includes examples of change ideas that CHCs could implement. Together with CHCs and other PHMI stakeholders, we will determine specific change ideas to focus on within PHMI.
FIGURE 5: EXAMPLES OF CHANGE IDEAS
Secondary Drivers |
Change Ideas |
|---|---|
Build data infrastructure; collect accurate REAL, SOGI and other sociodemographic data; and analyze data collected to identify inequities with populations of focus. |
|
Design and implement equity-focused care interventions that address the root causes of inequity in collaboration with patients and other partners. |
|
Demonstrate senior leadership’s ownership for and commitment to improving health equity. |
|
Understand and address internalized, personally- mediated and institutionalized racism. |
|
Establish practices and policies to promote workforce diversity and provide culturally and linguistically appropriate care. |
|
Partner with a full range of community partners and sectors, including DHCS, CPCA, Regional Associations of California (RAC), other CHCs, community-based organizations and managed care plans to improve equity. |
|
E. Existing Equity Efforts by California Consortia
CPCA and the four RAC involved in PHMI — Aliados Health, Central Valley Health Network, Community Clinic Association of Los Angeles County and North Coast Clinics Network — have all been supporting CHCs with centering equity in their work. PT Partners interviewed team members of each organization in September and October 2023 to better understand what opportunities were and are currently available to the PHMI CHCs. This information will help connect CHCs and build on existing efforts. Figure 6 below summarizes the equity work and offerings of CPCA and the RAC.
FIGURE 6: CPCA AND RAC EQUITY EFFORTS AND OPPORTUNITIES
CPCA |
Equity Efforts and Opportunities |
|---|---|
|
Leadership Equity Program Links to equity-focused system-level transformation |
|
|
Justice, Equity, Diversity & Inclusion (JEDI) Peer Network Links to equity-focused system- and ecosystem-level transformation |
|
|
Supporting Black Communities Workgroup Links to equity-focused practice transformation, and system- and ecosystem-level transformation |
|
RAC |
Equity Efforts and Opportunities |
|
Aliados Health Links to equity-focused practice transformation and system-level transformation |
|
|
Central Valley Health Network Links to equity-focused practice transformation |
|
|
Community Clinic Association of Los Angeles County Links to equity-focused practice transformation, and system- and ecosystem-level transformation |
|
|
North Coast Clinics Network Links to equity-focused practice transformation, and system- and ecosystem-level transformation |
|
In addition, in September 2023, the PT Partners interviewed all 32 CHCs that are a part of PHMI about their coaching preferences and current equity efforts and interests. The equity-related questions and responses are summarized in Figure 7 below.
FIGURE 7: CHC EQUITY EFFORTS AND INTERESTS
Question Asked During Interview |
Equity Efforts and Interest |
|---|---|
How is your organization defining equity? |
|
Could you share examples of health equity work? |
|
What are your wishes for equity moving forward? |
|
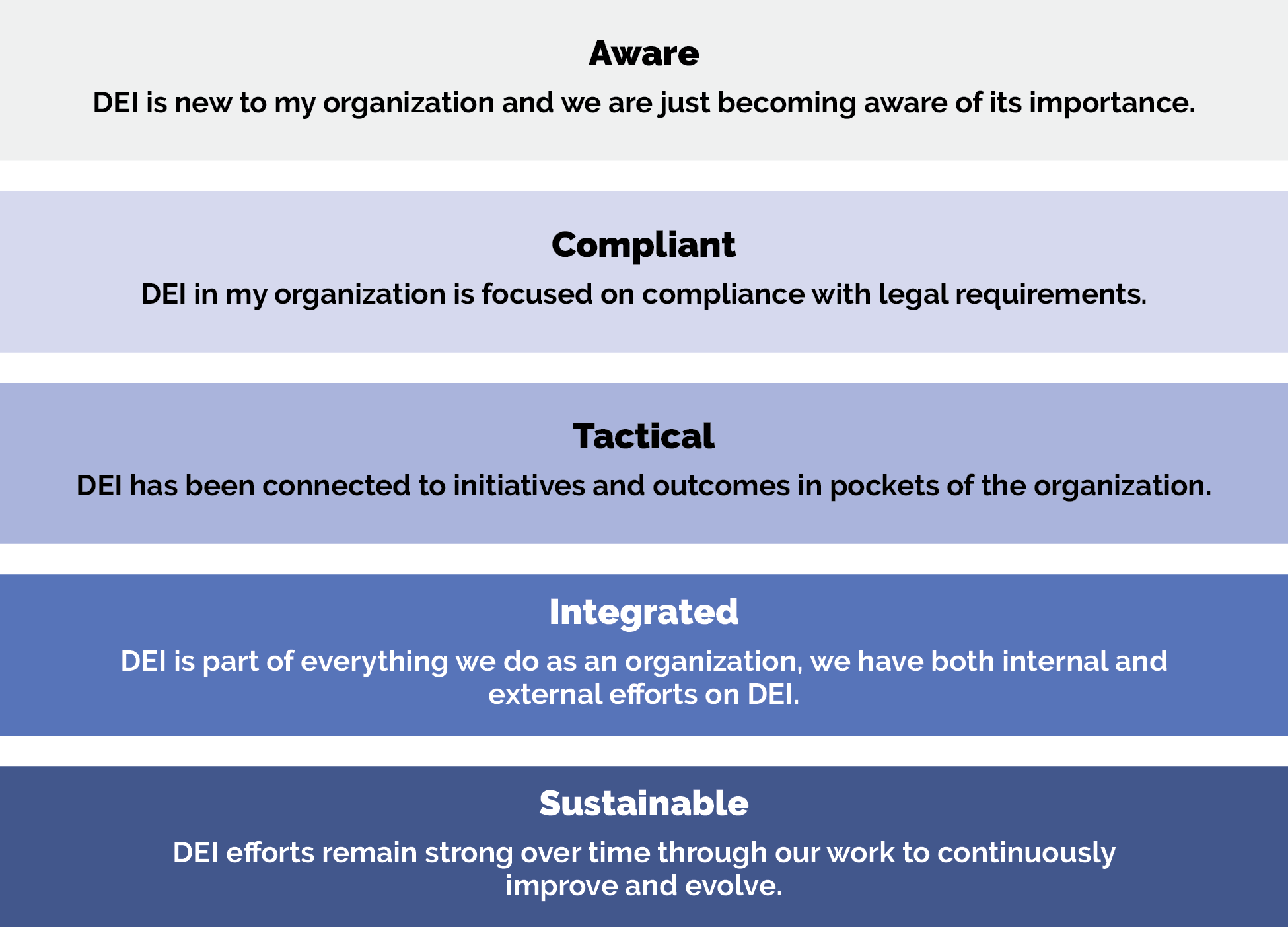
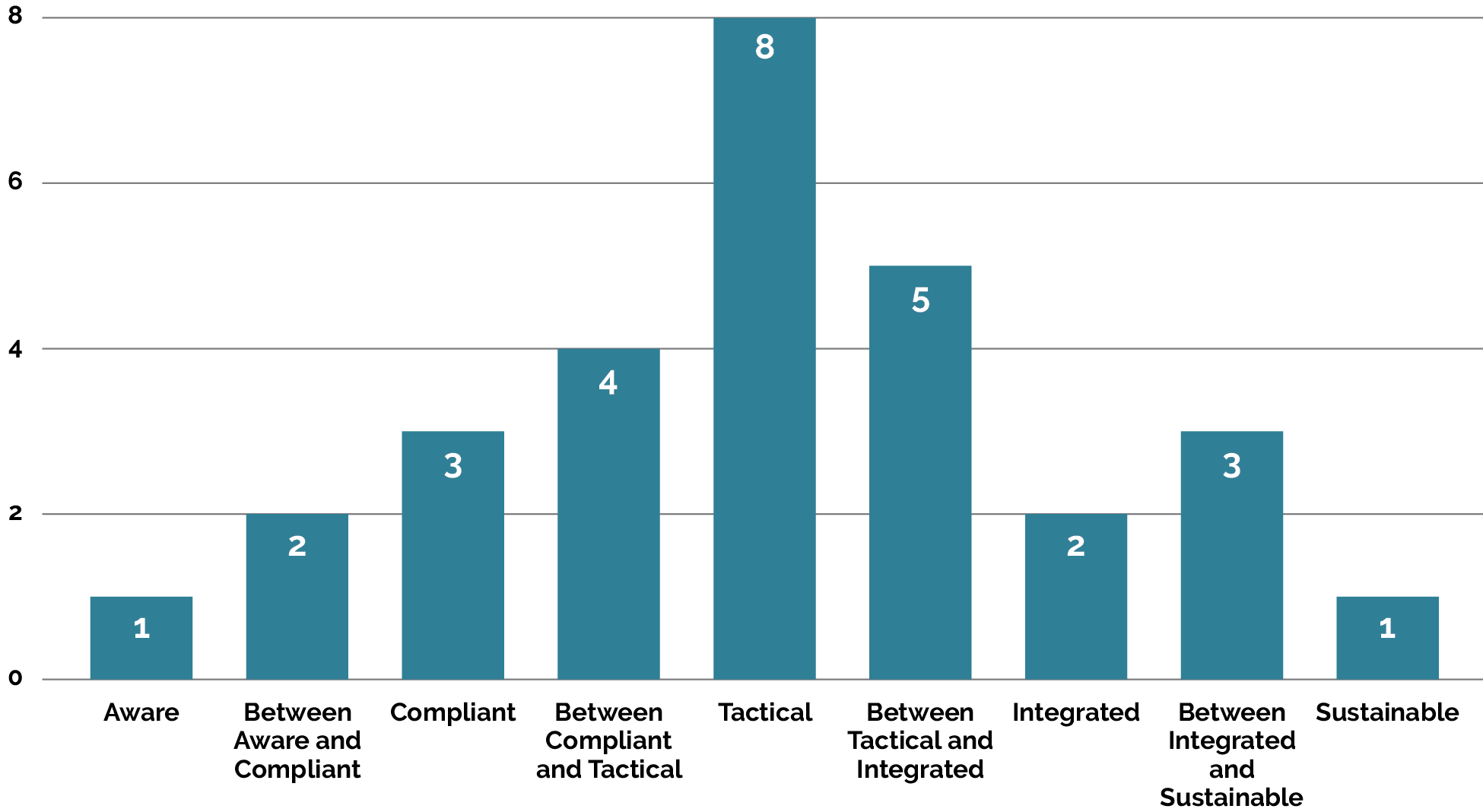
Another question that CHCs answered is where they would rank their health center in regard to their focus and work on equity. They chose from five different options, which are explained in Figure 8, below.
FIGURE 8: EQUITY RANKING OPTIONS
Out of the 32 CHCs, we received responses from 30 on how they rank themselves. One CHC rated themselves as “a bit of all,” so it was not included in the graph. Figure 9 below includes 29 CHC responses. Several CHCs ranked themselves between two different options, such as “between aware and compliant” or “between compliant and tactical”; these options have also been included in the graph. The majority of the CHCs ranked themselves in the middle as tactical.
FIGURE 9: CHC EQUITY RANKINGS
F. Integrating Equity Into the Curriculum and LAN
The Equity Framework and Approach will be integrated into the PHMI curriculum and LAN activities in the following ways.
Curriculum
- Implementation guides. Equity strategies and actions are incorporated throughout the Building the Foundation (BtF) and Populations of Focus Implementation Guides, both in how CHCs consider approaching and integrating equity-related key activities, and in calling out how equity is included in each PHMI population of focus.
- LAN curriculum. The curriculum includes equity topics, methods and tools (e.g., methods for making equity a strategic priority, tools for data stratification, methods for partnering with those with lived experience). The curriculum charts the path of strategy development and implementation for CHCs based on their readiness to advance equity. This path can be laid out across the different modalities for learning.
- Health information technology. Health information technology key considerations for embedding equity are below. These considerations align with the larger principles expressed in the “techquity” white paper.[16] The term “techquity” and the concepts in the white paper are being promulgated in the industry as a framework for ensuring that design, development and deployment of technology promote rather than exacerbate equity.
- Best practices for the collection and utilization of race/ethnicity, SOGI and SDOH
- Balance between data collection and respect and protection of patient
- Data-sharing practices reflect transparency around uses of data and measures to protect vulnerable communities and populations in how data is shared and
- Quality monitoring and training for staff who collect
- Identification of and attention to specific technology access issues, including broadband access, cost of technology, multiple languages, literacy, usability across different levels of ability and cultural
- Precautions around employed artificial intelligence models to ensure incorporated logic is appropriate to reduce and not exacerbate disparities.
Learning Action Network
- Peer-learning events. Examples of how equity could be included in peer-learning activities in the LAN include:
- Conduct equity-focused workshops in statewide and regional learning
- Foster “container building” to develop safe, shared spaces to talk about equity and to advance skills together. Include equity reflections and pauses for conversation throughout processes, even in non-equity-specific topic
- Build affinity groups during action periods around specific equity topics where select CHCs may need to go deeper (e.g., data stratification, partnering with those with lived experience, identifying a portfolio of equity improvement projects, racial/ethnic identity groups to support individual equity journeys).
- Coaching. Center equity in PHMI’s coaching efforts, including:
- Train coaches on this Equity Approach and hold spaces for ongoing equity discussions.
- Identify in real time when specific CHCs need individualized support in equity.
- Engage equity subject matter experts to work closely with the primary coaches and CHCs on implementing equity approaches.
- Work more intensely with CHCs that want deeper support to center equity.
- Communications. Feature “equity spotlights” of CHC and RAC challenges and successes on the PHMI website and newsletters.
- Measurement. Develop specific measures of how equity is being integrated by the PT Partners, including in quality assurance-related surveys.
G. Collaborative Design Process With Stakeholders
PT Partners conducted a collaborative design process to get a deeper understanding of the equity work that is already in progress and how it aligns with PHMI. This process was done, in part, to solicit feedback on the proposed Equity Approach and to learn from our stakeholders (CHCs, CPCA, DHCS and regional consortia) what actions they prefer to focus on and how they can best be supported in their equity journeys.
- In August, the PT Partners:
- Conducted a session at the all-stakeholder meeting (which included CHC, RAC and CPCA representatives). Some of the key themes from the meeting included the need for staff training around health-related social needs screening and more assistance with closing referral loops; the desire for timely, usable and granular data to identify and assess health inequity gaps; and understanding equity and adapting care teams and patient panels accordingly.
- In September, the PT Partners:
- Met with DHCS on September 8 to get feedback on the Equity Approach.
- Attended the all-RAC meeting on September 21 to get feedback on the Equity Approach.
- Met with CPCA and regional consortia in September to learn about current efforts in supporting CHCs in their equity journeys.
- Conducted interviews with CHCs and asked them equity-specific questions to capture where they are in their equity journey, as well as how they envision integrating equity work as a part of PHMI.
- In October, the PT Partners:
- Incorporated coaches’ ideas into the brief through feedback received in the coaches’ training.
- Conducted an environmental scan of existing equity initiatives and programs in which the CHCs are participating and which state and regional consortia offer to ensure we are building on and aligning with existing efforts.
- In November and December, the PT Partners:
- Continued to refine the PHMI Equity Approach and incorporated it into the populations of focus implementation guides.
- Worked with PHMI stakeholders to define recommended measures to include in the implementation guides.
H. Tracking Equity Work for PHMI
Our approach to tracking progress in equity in PHMI is multipronged, centered on both process and outcome measures, and focused on patient outcomes. This approach also will prioritize measuring the organizational and system transformation needed to spread and sustain those outcomes over time. We aim to center equity throughout PHMI to support participating CHCs to improve the health of their patients on the seven HEDIS core quality measures for PHMI, as shown in Figure 10 below.
FIGURE 10: HEDIS CORE QUALITY MEASURES
|
PHMI Populations of Focus |
Measures |
|---|---|
Children |
Child Immunization Status |
|
Well Child Visits in First 30 Months of Life |
|
Pregnant people |
Prenatal and Postpartum Care |
Adults with preventive care needs |
Colorectal Cancer Screening |
Adults living with chronic conditions |
Controlling High Blood Pressure |
|
Comprehensive Diabetes Care |
|
People with behavioral health conditions |
Depression Screening & Follow-Up for Adolescents and Adults |
To determine the short-term and intermediate impact of the equity work, the PT Partners will work together with the University of Chicago and Kaiser Permanente to determine which measures to track.
As a starting point to determining equity-related impact measures, the PT Partners reviewed the following two sets of measures:
- Select measures from the Population Health Management Capabilities Assessment (PhmCAT) listed in Figure 11 below to track the progress on key processes within CHCs that are vital for the infrastructure to advance equity.
- IHI’s 100 Million Healthier Lives Community Transformation Map tool, which helps to assess where a CHC is on the journey to becoming a healthy, equitable organization.8 It measures the organizational and system improvement and transformation that often accompany movement on population health measures but are less often focused on or tracked. The tool is designed to guide organizational teams through each stage of the process. Measures included in this tool are listed in Figure 12 below. The tool has been created for coalitions, but it can be adapted for CHCs and is an optional tool for CHCs to use.
FIGURE 11: PHMCAT MEASURES
PhmCAT Category |
PhmCAT Measure |
|---|---|
Business care for population health management |
Organization considers equity implications of budget decisions. |
Care team and workforce |
Recruitment, hiring and development of a workforce that reflects the population served. Self-management support provided by a trained core team and designed to be culturally and linguistically concordant with patient needs. |
Empanelment and access |
Telehealth and alternative visits are used by the practice to improve patient access. |
Technology and data infrastructure |
Organization uses disaggregated data on care processes or outcomes to identify issues and target resources/interventions. |
Leadership and culture |
Dedicated staffing, funding and structures to support equity, diversity and inclusion goals. Active support by clinical leaders and executive leaders for continuous learning and quality improvement. |
Patient-centered population-based care |
Measuring patient and community priorities by incorporating patient feedback into quality improvement activities and having a community engagement process. |
FIGURE 12: COMMUNITY TRANSFORMATION MAP MEASURES
Community Transformation Map Sections |
Community Transformation Measures |
|---|---|
How the CHC approaches the change process |
|
How the members of the CHC relate to one another and create abundance |
|
How the CHC leads for social change and equity |
|
With guidance from PHMI stakeholders, the PT Partners will identify additional key measures that might be assessed and measured beyond those in the PhmCAT.
Endnotes
- Health Equity Guide.org: a Human Impact Partners project [Internet]. Oakland (CA): Human Impact Partners. Defining health equity; [updated 2023 Jun 13; cited 2024 Mar 16]; [about 3 screens]. Available from: https://healthequityguide.org/about/ defining-health-equity
- Race Forward [Internet]. Washington: Race Forward; c2023. What is racial equity?; [cited 2023 Dec 12]; [about 5 screens]. Available from: https:// www.raceforward.org/what-racial-equity
- Centers for Disease Control and Prevention [Internet]. Atlanta: The Centers. NCHHSTP Social Determinants of Health; [updated 2022 May 9; cited 2023 Dec 12]; [about 3 screens]. Available from: https://www.cdc.gov/nchhstp/ socialdeterminants/index.html
- Kirwan Institute for the Study of Race and Ethnicity [Internet]. Columbus (OH): The Ohio State University. Lesson 1: What is implicit bias?; [cited 2023 Dec 12]; [about 1 screen]. Available from: https://kirwaninstitute.osu.edu/ implicit-bias-module-series/module-1- understanding-implicit-bias/lesson-1-what- implicit-bias
- Chin MH. Advancing health equity in patient safety: a reckoning, challenge and opportunity. BMJ Qual Saf [Internet]. 2021 Apr 19 [cited 2023 Dec 12];30:356-61. Epub 2020 Dec 29. Available from: https:// pubmed.ncbi.nlm.nih.gov/33376125
- Wyatt R (Office of Quality and Patient Safety, The Joint Commission, Oakbrook Terrace, IL); Laderman M, Botwinick L, Mate K, Whittington J. Achieving health equity: a guide for health care organizations [Internet]. Cambridge (MA): Institute for Healthcare Improvement; 2016 [cited 2023 Dec 12]. 46 p. Available from https://www.ihi.org/sites/default/files/ IHIAchievingHealthEquityWhitePaper.pdf
- Hostetter M (Pear Tree Communications, Cleveland, OH); Klein S. 100 million healthier lives: case studies from around the globe [Internet]. Cambridge (MA): Institute for Healthcare Improvement; 2020 [cited 2023 Dec 12]. 23 p. Available from: http://www.ihi. org/100MLives
- Department of Health Care Services. Comprehensive quality strategy 2022 [Internet]. Sacramento (CA): The Department; 2022 [cited 2023 Nov]. 194 p. Available from https:// www.dhcs.ca.gov/services/Documents/ Formatted-Combined-CQS-2-4-22.pdf
- Manchanda R (HealthBegins, Burbank, CA); Do R, Miles N. A toolkit to advance racial health equity in primary care improvement [Internet]. Oakland (CA): California Improvement Network, California Health Care Foundation, Healthforce Center at UCSF; 2022 [cited 2023 Dec 12].52 p. Available from: https://www.chcf.org/ publication/toolkit-racial-equity-primary- care-improvement
- Manchanda R (HealthBegins, Burbank, CA). The Compass for Health Equity Transformation: a tool to move from compliance to impact [Internet]. Burbank (CA): HealthBegins; 2023 Nov 1 [cited 2023 Dec 12]. [about 4 screens]. Available from: https://healthbegins.org/the-compass-for- health-equity-transformation-a-tool-to-move-from-compliance-to-impact
- Jones CP. Levels of racism: a theoretic framework and a gardener’s tale. Am J Public Health [Internet]. 2000 Aug; [cited 2023 Dec 12];90(8):1212-5. Available from: https://pubmed.ncbi. nlm.nih.gov/10936998
- California Primary Care Association [Internet]. Sacramento (CA): The Association; c2023. Leadership Equity Program; [cited 2023 Dec 12]; [about 5 screens]. Available from: https:// leadershipequityprogram.com
- California Primary Care Association [Internet]. Sacramento (CA): The Association; c2023. Workgroups; [cited 2023 Dec 12]. [about 2 screens]. Available from: https://www.cpca.org/CPCA/GET_ INVOLVED/WORKGROUPS.aspx
- North Coast Clinics Network [Internet]. Eureka (CA): The Network. QI project story boards; [cited 2023 Dec 12]. [about 5 screens]. Available from: https://www.northcoastclinics.org/ programs/quality-improvement/qi-project- story-boards
- Washington EF (Ellavate Solutions, Washington, DC). The necessary journey: making real progress on equity and inclusion. Boston: Harvard Business Review Press; 2022. 320 p.
- Anderson A. The Path to Techquity [Internet]. Ipsos; 2022 Mar [cited 2023 Dec 12]. Available from: https://www.ipsos.com/sites/default/ files/ct/publication/documents/2022-03/ Ipsos-HLTH-Path-to-techquity_0.pdf
- Domlyn, A, Scaccia, J, Lewis, N, Coleman, S, Saha, S. Community Transformation MapVersion 2.0. Boston: 100 Million Healthier Lives, convened by the Institute for Healthcare Improvement [internet]. Institute for Healthcare Improvement; 2020 [cited 2023 Nov]. Available from http://www.ihi. org/100MLives.