KEY ACTIVITY #11:
Use a Systematic Approach to Address Inequities within the Population of Focus
This key activity involves the following elements of person-centered population-based care: operationalize clinical guidelines; implement condition-specific registries; proactive patient outreach and engagement; pre-visit planning and care gap reduction; care coordination; behavioral health integration; address social needs.
Overview
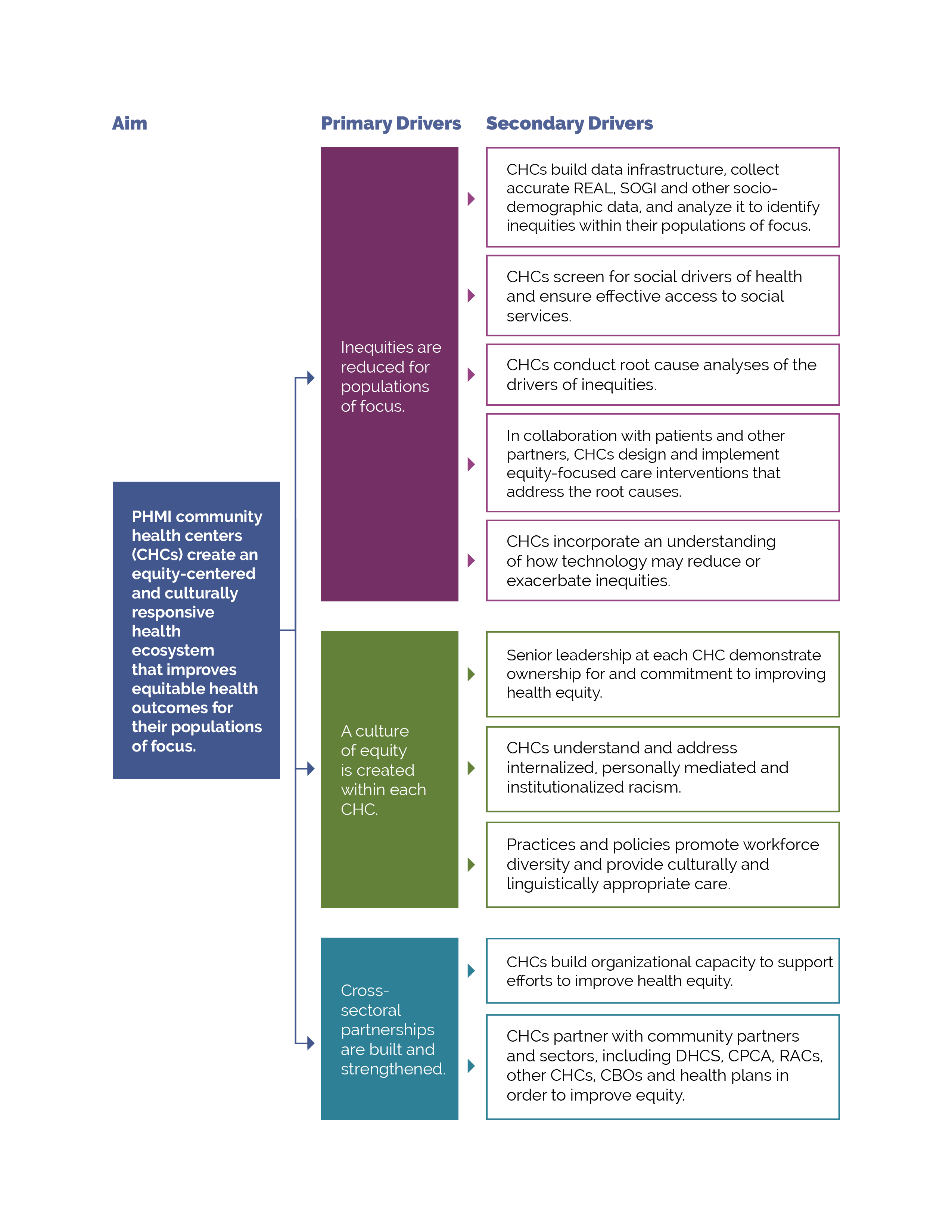
This activity provides guidance for a systematic evidence-based approach for identifying and then reducing inequities for people with behavioral health conditions. It focuses on the first primary driver in PHMI’s Equity Framework and Approach: Reduce inequities for populations of focus.
FIGURE 9: PHMI EQUITY DRIVER DIAGRAM
Your practice likely achieves better outcomes with certain populations or subpopulations and worse outcomes with others. Nationally, Black and Hispanic or Latino/awhite patients.[1][2] Reasons for such inequities are likely multifactorial and include factors such as socioeconomic status, experiences of structural and overt racism, family structure, neighborhood effects, and childhood adversity.[3] Some hypothesize that lower engagement with mental health services, combined with adverse childhood experiences, result in high levels of unmet need.[4][5] Social and cultural factors that serve as barriers to accessing care are generally most acute among persons of color, immigrants, persons speaking a primary language other than English, and people with historically stigmatized conditions, such as chronic pain and addictive disorders. As we work to reduce and, over time, eliminate inequitable health outcomes, we need to understand what contributes to these different outcomes as well as factors that do not contribute to them.
This includes recognizing that race is a social construct determined by society’s perception. While some conditions are more common among people of certain heritage, inequities in conditions, such as cancer, diabetes, and adverse maternal outcomes, have no genetic basis. While genetics do not play a role in these inequitable outcomes, the extent to which inequities in the quality of care received by people of color contribute to inequitable health outcomes has been extensively documented.[6] These inequities are often a direct result of racism, particularly institutionalized racism – that is, the differential access to the goods, services, and opportunities of a society by race.[7] Racial health inequities are evidence that the social categories of race and ethnicity have biological consequences due to the impact of racism and social inequality on people’s health.[8] It is also critical to recognize that we have policies, systems and procedures that unintentionally cause inequitable outcomes for racial, ethnic, language and other minorities, in spite of our genuine intentions to provide equitable care and produce equitable health outcomes.
Improving your practice’s key outcomes for behavioral health requires a systematic approach to identifying equity gaps (e.g., who your practice is not yet achieving equitable outcomes for) and then using quality improvement (QI), co-design, systems thinking, and related methods to reduce these equity gaps. This effort will be more effective if it is guided by a theory of change that addresses the ways in which structural and institutional racism lead to inequities in care provision. For more discussion, read resources such as this one on how structural and institutional racism has a negative impact on mental health.
Identifying and meeting patients’ social health needs is a key driver of reducing inequitable health outcomes. We provide additional guidance in this activity on how to both reduce inequities and meet patients’ social health needs.
Access to the data required to identify and monitor inequities, as outlined in the actions below, is fundamental to this activity.
Relevant HIT capabilities to support this activity include care guidelines, registries, clinical decision support (e.g., modifications required to consider disparate groups), care dashboards and reports, quality reports, inreach and engagement, and care management and care coordination. See Appendix D: Guidance on Technological Interventions.
EHRs can capture basic underlying socioeconomic, sexual orientation and gender identity (SOGI), and social needs-related data but may, in some cases, lack granularity or nuances that may be important for subpopulations. Mismatches between how UDS captures REAL data, versus how EHRs capture or MCPs report data, can also create challenges. This may require using workarounds to capture these details. It is also important to ensure that other applications in use that may have separate patient registration processes are aligned. Furthermore, tracking inequities in accessing services not provided by the health center may also require attention to data sources or applications outside the EHR.
Health centers should also be alert to the potential for technology as a contributor to inequities. For example, patient access to telehealth services from your practice may be limited by the inequitable distribution of broadband networks and patient financial resources (e.g., for phones, tablets, and cellular data plans).
Language, literacy levels, technology access, and technology literacy should also be considered and assessed against the populations served at the health center.
Action steps and roles
1. Build the data infrastructure needed to accurately collect REAL, SOGI, social needs and other demographic data.
Suggested team member(s) responsible: Data analyst.
- Race, ethnicity and language (REAL).
- Sexual orientation and gender identity (SOGI).
The PHMI Data Quality and Reporting Guide provides guidance and several resources for collecting this information. According to this guide, the initial step in addressing inequities is to collect high-quality data that fosters a comprehensive understanding of each patient. This entails incorporating REAL data, demographic data (e.g., age, gender), and social needs data. By leveraging this information, healthcare practices can gain valuable insights into differences in access, continuity and health outcomes." Steps two to four below provide more information on this process.
Collecting REAL information allows practices to identify and measure inequities in care while also ensuring that practices are able to interact successfully with patients. This is done by understanding their unique culture and language preferences.[9] KHA Quality has a toolbox that assists with REAL data collection.
The Uniform Data System (UDS) Health Center Data Reporting Requirements (2023 Manual) provides detailed guidance on REAL and SOGI. Note: While UDS does not currently require that practices report on the specific primary language of each patient, practices should make an effort to identify and record each patient’s primary language due to UDS reporting still requiring languages other than English to be reported.
Accurate collection of data requires appropriate fields and options in the EHR and other employed technologies, as well as appropriate human workflows in collecting the data. Staff responsible for data collection should be continuously trained and assessed for best practices in data collection, including the promotion of patient self-report.
In addition, practices should work to ensure that patients understand the importance and use of this information to help them feel comfortable supporting its collection. High rates of “undetermined” or "declined” in these fields may be indicative of the need to attend to these staff training needs.
Collecting this data is important, especially to obtain a complete picture of health for patients who identify as transgender. By understanding the needs of patients more fully, providers can make more informed decisions for the best treatment of their patients. The World Professional Association for Transgender health (WPATH) has provided further guidance regarding standards of care related to gender diversity.
2. Use the practice’s electronic health record (EHR) and/or population health management tool to understand inequitable health outcomes at your practice by stratifying your data.
Suggested team member(s) responsible: Data analyst.
This includes reviewing your care gap report or care registry and being able to stratify all of the following:
- Core measures for the population of focus.
- Supplemental measures for the population of focus.
- Process measures for the population of focus.
Stratify this data by:
- Race, ethnicity and language (REAL).
- Sexual orientation and gender identity (SOGI).
- Other factors that can help identify subpopulations in need of focused intervention to reduce an equity gap (e.g., immigrants, people experiencing homelessness, literacy levels, etc.).
This is not a one-time event but rather a continuous process (see step 13 below) and should be done in tandem with step three below.
Each practice should define the frequency of review and use of their registry to stratify data for adult preventive care. In early use, the stratified data will support the identification of areas of inequity and allow for prioritization of interventions.
3. Screen patients for social needs.
Suggested team member(s) responsible: Care team.
Key Activity 10: Develop a Social Needs Screening Process that Informs Patient Treatment Plans provides guidance on screening patients for health-related social needs and how the information can begin to be used to inform patient treatment plans, including referral to community-based services.
This is not a one-time event but rather a continuous process and should be done in tandem with step two above.
4. Analyze the stratified data from steps two and three to identify patterns in inequitable outcomes within the population of focus.
Suggested team member(s) responsible: Data analyst.
This includes:
- Utilizing tools to visualize and understand differences across different populations or subpopulations.
- Data over time (using run charts).
- Exploring trends, patterns and significant differences to understand which demographic groups will require a focused effort to close equity gaps.
This is not a one-time event but rather a continuous process (see step 13 below) and should be done in tandem with step two above and step four below.
Periodic review of the stratified data will provide insight into improvements in inequities and/or the emergence of new areas of disparity.
5. Conduct a root cause analysis for each population (e.g., demographic group) that the practice does not yet have equitable outcomes for.
Suggested team member(s) responsible: Multidisciplinary team.
Select root cause analysis approaches that work best for the equity gap you are closing:
- Engage and gather information from patients affected by the health outcome in your root cause analysis (see step six).
- Brainstorming.
- Systems thinking (e.g., understanding how interconnected social, economic, cultural, and healthcare access factors may be impacting the health outcome).
- Tools that rank root causes by their impact and the feasibility of addressing them (e.g., prioritization matrix and/or an impact effort matrix).
- Visual mapping of root causes and effects (e.g., fishbone diagram).
- Perform focused investigations into selected root causes, gathering qualitative data through interviews, surveys or focus groups with the subpopulation of focus.
Present the findings to a broader group of stakeholders to validate the identified root causes and gain additional insights. Incorporate their feedback and refine the analysis, as needed.
6. Partner with patients to develop additional insights that will help you develop successful strategies.
Suggested team member(s) responsible: Care team and people with lived experience (e.g., patients representative of the population(s) of focus).
Using one or more human-centered design methods, such as focus groups, 7- Stories, Journeymapping, etc. (see links to these methods below), work with patients of each population of focus to better understand:
- Their assets, needs and preferences, as they relate to adult prevention recommendations.
- Cultural beliefs, including traditional healing practices that may impact their understanding of or willingness to engage in certain adult prevention practices.
- Beliefs and level of trust in healthcare generally and in the topic of focus specifically (e.g., cancer screening, immunizations, behavioral health, etc.).
- Barriers to accessing care, including health insurance, transportation, childcare, housing access and other social factors.
- Barriers to remaining engaged in care, including the above-noted barriers and including cultural beliefs, trust, and concerns about follow-up requirements.
- Trusted sources of information and communication mechanisms and preferences for this population.
- Their ideas for improving health outcomes as they relate to the uptake of preventive care.
The patients you partner with for this and other steps in this activity may be part of a formal or informal patient group and/or identified and engaged specifically for this equity work.
7. Identify key activities that address or partially address the identified equity gaps.
Suggested team member(s) responsible: Care team.
Based upon the insights your practice has developed for a population of focus and your root cause analysis, determine which of the key activities in this implementation guide could address or partially address the equity gap.
Most of the key activities in this guide either explicitly address an equity challenge or can be adapted to better address an equity challenge. Examples of activities that can be adapted to reduce identified equity gaps include but are not limited to:
- Key Activity 5: Enhance Inreach and Outreach to Engage People in Behavioral Healthcare.
- Key Activity 6: Expand Access to Integrated Care, particularly around providing cultural humility training.
- Key Activity 9: Adopt Universal Screening of All Adults for a Range of Behavioral Health Needs.
- Key Activity 10: Develop a Social Needs Screening Process that Informs Patient Treatment Plans, such as providing a referral for one of the CalAIM Community Supports.
- Key Activity 14: Coordinate Care.
- Key Activity 17: Continue to Develop Referral Relationships and Pathways.
- Key Activity 18: Strengthen Community Partnerships.
8. Develop new strategies/ideas to address the identified equity gaps.
Suggested team member(s) responsible: Care team and people with lived experience.
If one or more of your root causes cannot be addressed fully through any of the key activities in this guide, use one or more human-centered design methods (see resources below) to develop ideas to improve health outcomes and reduce inequities among this population.
Developing these ideas is best done with representatives of the population of focus, as they have expertise and experience that may be missing from the practice’s care team. In an effort to generate dozens of potentially viable ideas during this brainstorm, develop potential strategies without immediate judgment of the ideas.
Selected resources on human-centered design and co-design:
- Center for Care Innovations (CCI) Human-Centered Design Curriculum.
- IDEO’s Field Guide to Human-Centered Design.
- IDEO’s Design Kit: Methods.
9. Determine which strategies to test first.
Suggested team member(s) responsible: Care team and people with lived experience.
Steps seven and eight above help your practice identify existing key activities and generate new ideas. Your practice likely doesn’t have the bandwidth to test all of them, at least not at the same time, so now is the time to prioritize a few to begin testing.
There are many ways to prioritize ideas. The Institute for Healthcare Improvement often recommends a prioritization matrix and/or an impact effort matrix.
If you have organized your key activities and new ideas into themes or categories, you may choose to work on one category or select one to two ideas per category to work on.
The number of key activities and/or new ideas that you prioritize for testing first should be based on the team’s bandwidth to engage in testing. It is critical to determine the bandwidth for the team(s) that will be doing the testing so that you can determine how many ideas to test first.
10. Use quality improvement (QI) methods to begin testing your prioritized key activities and new ideas.
Suggested team member(s) responsible: Care team and people with lived experience.
Nearly all the key activities and all of your new ideas will require some degree of adaptation for use within your practice and to be culturally relevant and appropriate to your population(s) of focus.
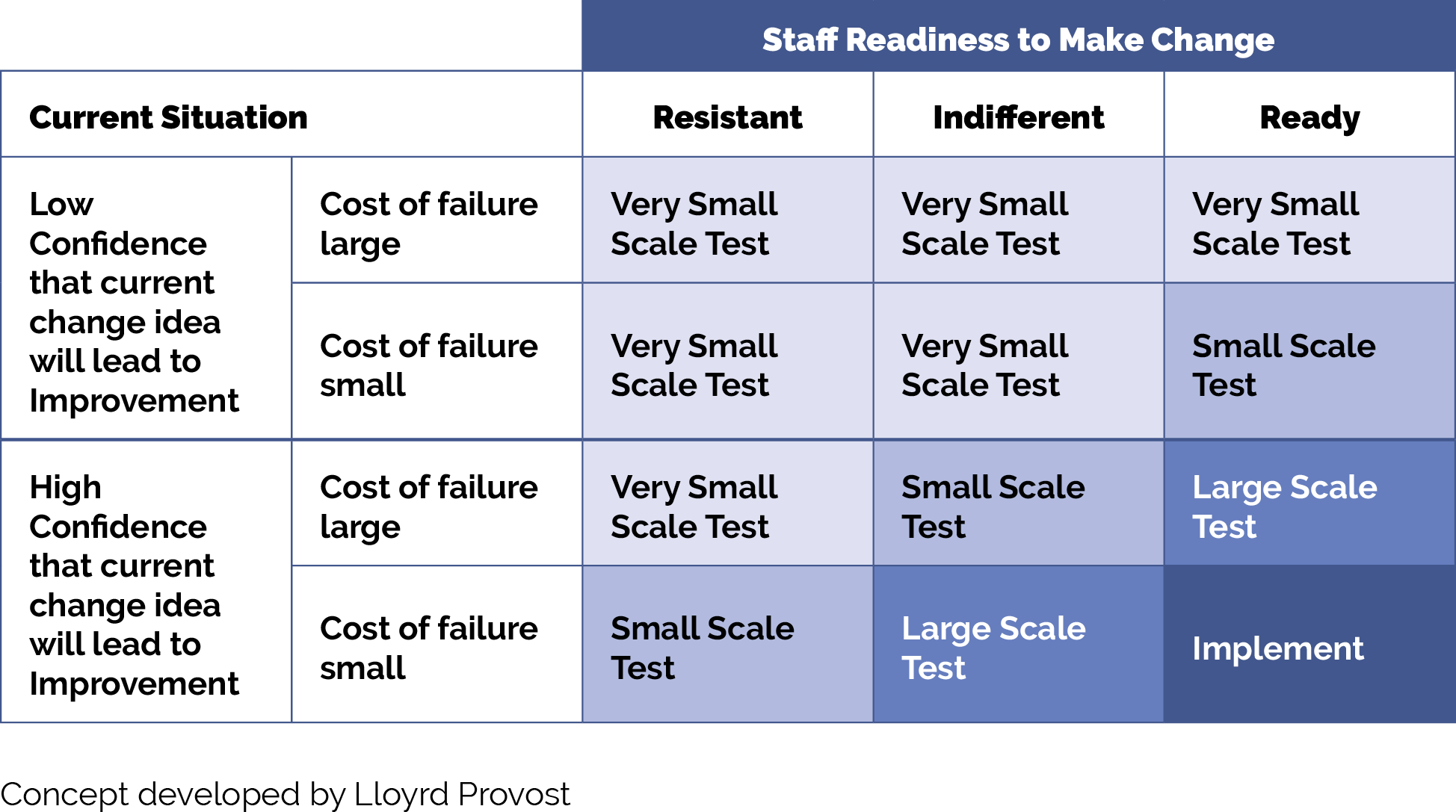
Use plan-do-study-act (PDSA) cycles, as feasible, generally starting as small as feasible. Think “ones” (e.g., one clinician, one hour, one patient, etc.) and become larger as your degree of belief in the intervention grows.
Whenever testing an activity or new idea, we recommend that the practice:
- Use PDSA cycles to test your ideas and bring them to scale. See more information on PDSAs below in the tips and resources section.
- Generally, start with smaller scale tests (e.g., test with one patient, for one afternoon, in a mailing to 10 patients, etc.). Use Figure 10 below in the tips and resources section to help you decide what size test is most appropriate.
Develop or refine your learning and measurement system for the ideas you are testing. A simple, yet robust learning and measurement system will help you know if your ideas are having their intended effect, if they are having unintended secondary effects (e.g., staff burnout), and how the overall implementation process is going. Consider the following:
- What core measures, supplemental measures and/or process measures is this intervention designed to improve equity for?
- What are or will be the first or early indications that the intervention or idea is working?
- How will you know how the implementation itself is going from a patient perspective, a staff perspective, and a management perspective?
- What are some balancing measures to monitor, including those for the implementation itself and those related to spending time and resources on implementation?
- Study the successes and challenges of the test. When feasible, this should include getting feedback from patients directly after testing a new idea with them and incorporating their feedback into your next test.
- Refining the idea, as needed, based on the test.
- Testing again and increasing the scale of the test as these tests result in fewer challenges and better results.
By working out the inevitable kinks in the idea you are testing before taking it to full scale, the practice will make the idea work better for patients and less frustrating to the care team. Testing and refining also can eliminate the workarounds that occur when a process or approach doesn’t fit well into the system or workflow it is being placed into.
Select resources on quality improvement (QI):
- The Institute for Healthcare Improvement (IHI) QI Essentials Tooklit includes details on:
- Cause and effect diagrams.
- Driver diagrams.
- Failure modes and effects analysis.
- Flowcharts.
- Histograms.
- Pareto charts.
- PDSA worksheets.
- Project planning forms.
- Run charts.
- Scatter diagrams.
- IHI’s videos on the Model for Improvement (parts 1 and 2).
- Rapid Experiments to Improve Healthcare Delivery.
- Center for Care Innovation’s ABCs of QI.
11. Implement – bring to full scale and sustain – those practices that have proven effective.
Suggested team member(s) responsible: Care team.
Once an idea has been well tested and shown to be effective, it is time for your practice to hardwire the idea, approach or practice into your daily work. Consider using the MOCHA implementation planning worksheet to think through:
- Measurement.
- Ownership.
- Communication, including training.
- Hardwiring the practice.
- Assessment of workload.
Sometimes, implementation may require that you update your protocol and/or policies and procedures for the populations of focus.
12. Once you have tested, refined and scaled up the initially prioritized ideas, begin testing other ideas.
Suggested team member(s) responsible: Care team and people with lived experience.
This might include going back to the ideas developed previously but not prioritized and/or going back through the testing steps above to develop and prioritize new ideas, potentially for additional populations of focus.
13. Put in place formal and informal feedback loops with patients and the care team.
Suggested team member(s) responsible: Care team.
Establishing formal and informal feedback loops regarding new processes will ensure that your practice’s ideas are meeting the needs of patients and are reducing identified equity gaps. These feedback loops also ensure the changes are feasible and sustainable for your practice.
For patients, feedback loops could be created using many of the human-centered design tools used to design your improvement activity (e.g., surveys, interviews, focus groups).
Consider establishing a standing funded patient advisory board that is available to design, implement and evaluate all of your practice’s improvement activities.
For the care team, feedback loops might include:
- Existing or new staff satisfaction/feedback mechanisms.
- Regularly scheduled meetings/calls to get staff feedback on processes, methods and tools.
14. Continually analyze your data to determine if your efforts are closing equity gaps.
Suggested team member(s) responsible: Care team.
This includes regular (at least monthly) review of the stratified measures for all of the following:
- Core measures for the population of focus.
- Supplemental measures for the population of focus.
- Process measures for the population of focus.
- Social needs data.
- Any additional measures collected as part of your testing and refinement effort.
Share the data with patients to both show your work to decrease known equity gaps and to solicit ideas for closing them.
Implementation tips
In integrated behavioral health settings, it is especially important that quality improvement is an effort of the integrated team with the express involvement of behavioral health clinicians and community health workers.
When testing an idea for change (either a key activity or new idea) for your practice to address a known equity gap, the size of your test scope or group is critical. We recommend starting with a very small test (e.g., with one patient or with one clinician) or a small test (e.g., with all patients seen during a three--hour period by this clinician) unless you are certain the change idea, activity or test will lead to improvement with little or no adaptation for your practice, the cost of a failed test is extremely low, and staff are excited to test the change idea. As you learn from each test what is and isn’t working, you can conduct larger scale tests and tests under a variety of conditions. While at first glance this would appear to slow down the implementation effort, starting small and working out the kinks as you progressively work to full scale actually saves time and resources and is much less frustrating for your patients and care team. Figure 10 provides guidance on how big your test should be.
FIGURE 10: HOW BIG SHOULD MY TEST BE?
Resources
Endnotes
- Simpson, S. M., Krishnan, L. L., Kunik, M. E., & Ruiz, P. (2007). Racial disparities in diagnosis and treatment of depression: a literature review. The Psychiatric quarterly, 78(1), 3–14. https://doi.org/10.1007/s11126-006-9022-y
- Enslow, M. R., Galfalvy, H. C., Sajid, S., Pember, R. S., Mann, J. J., & Grunebaum, M. F. (2023). Racial and ethnic disparities in time to first antidepressant medication or psychotherapy. Psychiatry research, 326, 115324. https://doi.org/10.1016/j.psychres.2023.115324
- Garcia JL. Historical trauma and American Indian/Alaska Native youth mental health development and delinquency. New Dir Child Adolesc Dev. 2020;2020(169):41-58.
- Viswanathan M, Wallace I, Middleton JC, et al. Screening for Depression, Anxiety, and Suicide Risk in Children and Adolescents: An Evidence Review for the U.S. Preventive Services Task Force. Evidence Synthesis No. 221. Agency for Healthcare Research and Quality; 2022. AHRQ publication No. 22-05293-EF-1.
- Koball, A. M., Rasmussen, C., Olson-Dorff, D., Klevan, J., Ramirez, L., & Domoff, S. E. (2019). The relationship between adverse childhood experiences, healthcare utilization, cost of care and medical comorbidities. Child abuse & neglect, 90, 120–126. https://doi-org.aurarialibrary.idm.oclc.org/10.1016/j.chiabu.2019.01.021
- Institute of Medicine. 2003. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: The National Academies Press. https://doi.org/10.17226/10260
- Improving Health Equity: Build Infrastructure to Support Health Equity. Guidance for Health Care Organizations. Boston, Massachusetts: Institute for Healthcare Improvement; 2019. (Available at www.ihi.org)
- Chadha N, Lim B, Kane M, Rowland B. Institute for Healing and Justice in Medicine; 2020. https://belonging.berkeley.edu/race-medicine
- REaL Data Collection Toolbox [Internet]. KHA; 2022 [cited 2023 Dec 18]. Available from: http://www.khaquality.com/Portals/[4]/Resources/HQIC_REaL%20Data_Collection_Toolbox.pdf