KEY ACTIVITY #8:
Proactively Reach Out to Patients Due for Care
This key activity involves all seven elements of person-centered population-based care: proactive patient outreach and engagement; pre-visit planning and care gap reduction.
Overview
Conducting proactive outreach can ensure patients follow through on recommended care.
As part of PVP and other clinical workflows, your practice should be conducting some level of outreach to provide patients with information they may need to prepare for upcoming visits or engage in follow-up care. In addition, most EHRs can be integrated with an automated reminder system for upcoming appointments and apparent gaps in care, such as a patient being due for an A1c lab or a diabetic foot exam. Patient outreach also occurs as a part of care coordination, especially around supporting patients to engage in external referrals and in follow-up to a hospital admission or discharge (see Key Activity 18: Coordinate Care).
Proactive outreach to patients due for care focuses on identifying subpopulations among the patients assigned to a care team who may benefit from additional outreach and implementing more personalized reminders and “touches” to encourage them to engage in care.
Outreach to people who are not yet actively engaged in care goes beyond this foundational activity. See Key Activity 20: Strengthen Community Partnerships for more about identifying trusted messengers in your community.
Proactive outreach ensures that patients remain engaged in care. It also provides an opportunity for their health needs to be identified and addressed in a timely manner. Untreated health needs can lead to worse outcomes; proactive outreach may improve health outcomes and help ensure that the patient feels that their overall well-being is valued by the practice.
Timely engagement and development of an environment that is conducive to effective chronic condition management can lead to better health outcomes and reduce long-term healthcare costs by preventing the exacerbation of an untreated condition. Patients who have a chronic disease and feel asymptomatic may become disengaged with care if not regularly engaged by their care team.
Focus on equity by using data to identify which populations, subpopulations or groups the current outreach and education efforts do not reach. See the PHMI Data Quality and Reporting Guide for more information.
Unmet health-related social needs (e.g., income security, transportation and health literacy) can result in no-shows and deterioration of patient health status. Proactive outreach, combined with awareness of health-related social needs, ensures that practices can connect patients to community resources while establishing trust in the care team. See Key Activity 17: Use Social Needs Screening to Inform Patient Treatment Plans and Key Activity 20: Strengthen Community Partnerships for more information.
Co-designing outreach strategies with community partners and current patients promotes cultural humility and sensitivity. Tailored outreach with personalized reminders addresses diverse needs, reducing inequities in access to care.
This activity relies on similar capabilities as care gap management, utilizing population views and registries to track gaps in adult preventive healthcare against screening guidelines. These registries can be utilized to generate outreach lists for appointment schedulers and/or care managers and other care team members who might be tasked with contacting patients due for services. Many EHRs are capable of storing next appointment data that can also be used to generate lists and may link to automated appointment outreach workflows. Patient-facing outreach and engagement technologies can be utilized for delivering appointment reminders and for patient self-scheduling. Care managers might use care management applications to track and prompt adult preventive health needs, as well as wellness visits.
Other relevant HIT capabilities to support this activity include care guidelines; clinical decision support, including patient-facing clinical decision support; care dashboards; and reports. Some health centers may focus extra resources on adult patients identified as high risk through risk-stratification algorithms.
Action steps and roles
1. Identify subpopulations among your patients who may benefit from outreach.
Suggested team member(s) responsible: panel manager or data analyst with care teams.
Some methods for identifying subpopulations to reach out to may include:
- Start with frequent no-show patients. Seek to understand their reasoning behind the no-shows, which may be related to social health-related needs or health literacy issues.
- Ask your care teams to identify patients they consider high-risk patients who have been lost to care.
- This may also include reaching out to patients who have not been seen in the last 12 months.
- Conduct outreach to patients whose last blood pressure was not controlled but who did not have a follow-up.
- Use care gap reports to identify patients who are behind on screening or who have missed a follow-up visit.
- Review all patients who are due for a follow-up review of their care plan or who have not had an updated blood pressure or glucose laboratory test; prioritize those patients for outreach.
See Key Activity 3: Use Care Gap Reports or Registries to Identify All Patients Eligible and Due for Care for more information.
2. Establish the outreach model for your practice.
Suggested team member(s) responsible: practice leadership.
One commonly used outreach model is to hire dedicated staff as population health specialists who are responsible for using care gap reports to conduct proactive outreach and to schedule follow-ups. See more about this in the PHMI Care Teams and Workforce Guide Resource 2: Care Team Duties and Recommended Education and Licensure resource.
Different teams may adjust this role to fit their needs. This model ensures that each care team includes staff with knowledge of the local environment.
Train all outreach staff in cultural humility, motivational interviewing skills and the use of trauma-informed care. See more in the resource: Trauma-Informed Population Health Management.
3. Supplement your reminder system for contacting various subpopulations.
Suggested team member(s) responsible: population health specialist, with guidance from implementation team and IT staff.
Reminders should be sent to all persons with an upcoming scheduled appointment. The clinic scheduling system will likely have a function for generating automated reminders with an option for patients to cancel or reschedule if they cannot keep the appointment. Reminders should also be sent to all patients who appear to have gaps in care and missed appointments. See more about updating your care gaps reports to enable setting up automated reminders in Key Activity 3: Use Care Gap Reports or Registries to Identify All Patients Eligible and Due for Care. The reminders could include a request to bring medications and any home-monitoring readings, such as home glucose and blood pressure readings. These are valuable resources for clinicians as they allow the clinicians to complete an accurate medication reconciliation and review the readings during the patient’s appointment.
Automated reminder systems support efficiency and reliability. However, more intensive reminders where the patient receives a personalized telephone call from their care team may help patients who are at higher risks of nonattendance or being lost to care.[1]
FIGURE 13: PROACTIVE OUTREACH AND ENGAGEMENT
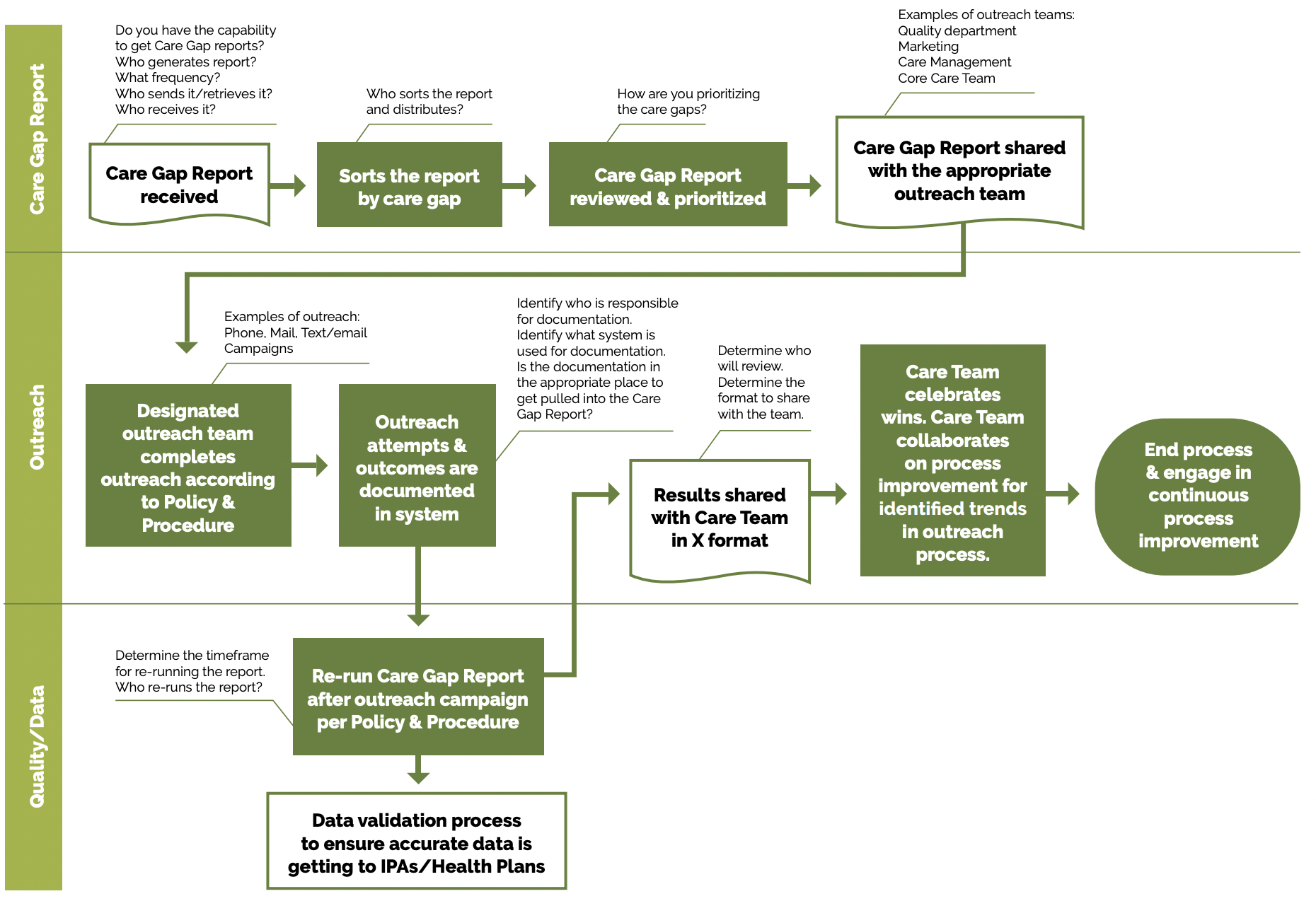
See the PHMI Care Teams and Workforce Guide Resource 6: Workflow Examples for more information.
Utilize multiple pathways to reach and engage patients. For example, a Swiss clinic used sequential appointment reminders consisting first of a phone call and second a text if patients did not answer the phone after three attempts. If the patient had no phone number listed, they received a postal reminder two days prior to their appointment. The reminder system significantly reduced the rate of missed appointments and allowed the clinic to reallocate 28% of the canceled appointments.[2]
Reminders should accommodate language requirements, as well as stated patient communication preferences (text, email, mail or phone). Reminders that include standard information (appointment date, time, clinic location), as well as information about what to expect and additional clinical information, may be more effective.[3]
4. Use “touches” that provide alternatives to the traditional office visit.
Suggested team member(s) responsible: extended care team, including community health workers and population health specialist, with guidance from implementation team.
Assess what types of interactions/care can be provided outside of a typical office setting. Collaborate with patients as part of their care planning to understand their preferences for communication and care team interactions. Examples of alternative interactions include, but are not limited to:
- Nursing staff visits (virtual).
- Pharmacy visits.
- Digital communication through emails, texts and patient portals.
- Newsletters focused on a specific condition.
- Social media that includes discussion groups related to the management of conditions of focus.
- Home visits for high-risk, underserved, or mobility-challenged patients.
- Other technological solutions, such as apps focused on patient conditions that provide a vehicle for ongoing engagement.
For patients with diabetes, group visits often can result in peer support systems that contribute to health literacy and assist with addressing health-related social needs. See Key Activity 19: Provide Group Visits for Chronic Care Management for more information.
Foster patient’s ability to self-monitor their diabetes and/or hypertension at home: For patients with hypertension and/or diabetes, empowering patients to self-measure their blood pressure can influence their health literacy and lifestyle choices. See Key Activity 24: Develop System to Provide Remote Patient Monitoring for more information.
5. Establish a process for engaging patients assigned to your practice by their managed care team who have not yet been seen by the practice.
Suggested team member(s) responsible: multidisciplinary implementation team.
Depending on your agreement with the health plans, it is important for practices to make a proactive plan to build capacity to accommodate assigned-but-not-yet-seen health plan patients in the clinic. Practices should develop strategies for outreach and engagement with these populations in order to shift them from not yet seen to fully engaged in primary care.
6. Continuously reassess outreach approaches with a goal of improvement.
Suggested team member(s) responsible: population health specialist.
Test your outreach approaches and measure their effectiveness. Outreach can be measured by reviewing data from missed appointments, numbers lost to follow-up, etc.
Survey patients to obtain retrospective and prospective feedback on outreach efforts.
Regularly update outreach strategies based on community feedback and changing demographics.
Implementation tips
Providing more intensive outreach: For high-risk patients or patients with complex health and social needs, consider care management as a more intensive approach for facilitating ongoing communication and coordination (See Key Activity 21: Provide Care Management and Key Activity 18: Coordinate Care).
Exploring one-time outreach efforts: If there is a backlog of patient care gaps, consider a campaign where you focus on closing gaps for specific screenings, labs or vaccines.
Going deeper with community partners: Consider strengthening community partnerships to provide greater infrastructure for closing gaps in care (see Key Activity 20: Strengthen Community Partnerships). Community partners can support outreach and health literacy efforts, participate in co-design by providing insight around a particular patient population, and provide resources and supports for patients. For example, education and programs on chronic conditions can be made broadly available through community partners (such as schools, community gathering places, churches, senior centers, etc.), which allows for community health improvement beyond the typical reach of the practice. Consider nontraditional community partners that allow practices to reach patients where they are.
- A more intensive approach to outreach involves the more real-time information flow between the clinician and the patient enabled by RPM programs. See Key Activity 24: Develop System to Provide Remote Monitoring for more information.
- The Sonoma County Indian Health Project used a script to talk to patients about joining its program that focuses on preventing heart attacks and strokes in patients with high blood pressure, high cholesterol and high glucose levels.
- This patient brochure from San Francisco Health Network educates patients on strategies to identify risk factors for heart disease and improve blood pressure.
Evidence base for This activity
Biola H, Deyo J, Hayes T, Small L, Chaplin J, Pak-Harvey E, et al. Reaching the Hard-to-Reach: Outcomes of the Severe Hypertension Outreach Intervention. American Journal of Preventive Medicine [Internet]. 2020 Nov 1;59(5):725–32. Available from: https://www.ajpmonline.org/article/S0749-3797(20)30291-9/fulltextDenberg TD, Myers BA, Eckel RH, McDermott MT, W. Perry Dickinson, Lin CT. A patient outreach program between visits improves diabetes care: a pilot study. International Journal for Quality in Health Care. 2009 Apr 1;21(2):130–6.
Endnotes
- McLean SM, Booth A, Gee M, Salway S, Cobb M, Bhanbhro S, Nancarrow SA. Appointment reminder systems are effective but not optimal: results of a systematic review and evidence synthesis employing realist principles. Patient Prefer Adherence. 2016 Apr 4;10:479-99. doi: 10.2147/PPA.S93046. PMID: 27110102; PMCID: PMC4831598.
- Perron NJ, Dao MD, Kossovsky MP, Miserez V, Chuard C, Calmy A, Gaspoz JM. Reduction of missed appointments at an urban primary care clinic: a randomised controlled study. BMC Fam Pract. 2010 Oct 25;11:79. doi: 10.1186/1471-2296-11-79. PMID: 20973950; PMCID: PMC2984453.
- McLean SM, Booth A, Gee M, Salway S, Cobb M, Bhanbhro S, Nancarrow SA. Appointment reminder systems are effective but not optimal: results of a systematic review and evidence synthesis employing realist principles. Patient Prefer Adherence. 2016 Apr 4;10:479-99. doi: 10.2147/PPA.S93046. PMID: 27110102; PMCID: PMC4831598.