©️ 2024 Kaiser Foundation Health Plan, Inc.
This guide provides step-by-step guidance for improving population-based care for children with the goal of supporting substantive cultural, technological, and process changes, focusing on child immunization status, well child visits in first 30 months of life, child and adolescent well care visits, and immunization for adolescents.
This guide was designed as part of the Population Health Management Initiative (PHMI), a California collaboration of the Department of Health Care Services (DHCS), Kaiser Permanente and Community Health Centers. Much of the content is relevant and adaptable to primary care practices of all kinds working to improve the health of the populations they serve.
Preventive screenings and care for children and adolescents reduce the risk of disease that can lead to disabilities and premature mortality. However, many in the United States do not utilize suggested preventive healthcare services.[1]
In the case of children, regular well-child check-ups are essential to monitor growth and identify potential health issues at early stages when intervention is often more effective. Screenings and vaccinations play a pivotal role in upholding the well-being of individuals spanning various age brackets.[2][3]
This guide provides practices with detailed guidance, examples, resources and tools to develop, test, refine, bring to scale, and continually improve protocols around children’s immunization and well-child visits (WCVs). This guide is designed to be helpful as part of an organized quality improvement strategy, with the goal of supporting substantive cultural, technological and process changes that improve population-based care for pediatrics.
The guide lists several key activities by section:
- Foundational activities: The core activities that all practices must implement as part of their children’s immunization and WCV protocol.
- Going deeper activities: More advanced activities that build off the foundational activities and further your efforts to achieve equitable improvement in your children’s immunization and WCV rates.
Sequencing activities: We recommend that practices consider planning and attempting to implement the activities in the sequence provided in this guide. At the same time, we recognize that different practices may follow a different path toward prioritizing and implementing these activities. Furthermore, there is a lot of overlap between activities; many activities build off of or from the building blocks of other activities.
Testing and implementing: For each activity we provide guidance on how to plan, test and implement the activity along with links to other resources, technology considerations and examples. Consider testing different versions of the action steps and roles on a small scale before fully implementing at your practice.
Maintaining the progress: For many activities we have also provided tips for periodically reviewing and making improvements to key workflows even after initially implementing the change. Ongoing review and continual improvement are important for your practice to maintain your progress in population health management and help you stay nimble in adapting to changing patient demographics, new clinical best practices, new payment policies, workforce changes, and other changes at your practice.
If you implement the foundational activities in this guide, you should be able to achieve the following foundational competencies:
For pediatrics, your practice will be able to consistently:
- Engage patients served by your practice to validate any proposed process improvements and to learn alternative methods to improve quality in your focus area.
- Analyze core quality measures to identify disparities and improvement opportunities for adherence to American Academy of Pediatrics (AAP) preventive care guidelines year over year among attributed patients.
- Incorporate AAP preventive care guidelines into well-child visit protocols for infancy and early childhood (up to 30 months).
- Create an outreach protocol to reach and engage all attributed patients due for care.
- Prepare for integrating behavioral health follow-up services as needed.
- Create a health-related social needs screening process that informs patients’ treatment plans.
- Assess current capabilities and develop a plan for ongoing improvement in data utilization, care team workflows and efficiency that includes sustainable health information technology (HIT) strategies and continuous staff training on technology.
This guide also includes sections on measurement, equity, social health, behavioral health integration and an appendix including helpful tools and resources. We have included information about California Medi-Cal covered benefits and services that were up-to-date at the time of publishing, but benefits and billing guidance change over time. Nothing in this guide should be considered formal guidance, and anyone using this guide should check with the appropriate authorities on benefits and billing guidance.
This is a living document and will change based on continued learning on this topic and may include additional activities, examples, resources and sections in the future.
Improving the health of a population impacts everyone in a practice. Critical roles needed to engage in the work outlined in this guide and support practice change include:
- Quality improvement leadership, like a director of quality improvement (QI) or additional team leads (e.g., clinical, front office, etc.), to support cultural changes.
- Coaches or practice facilitators who are partnered with teams to help identify areas for improvement and support change through change management strategies.
Putting the Key Activities in Context
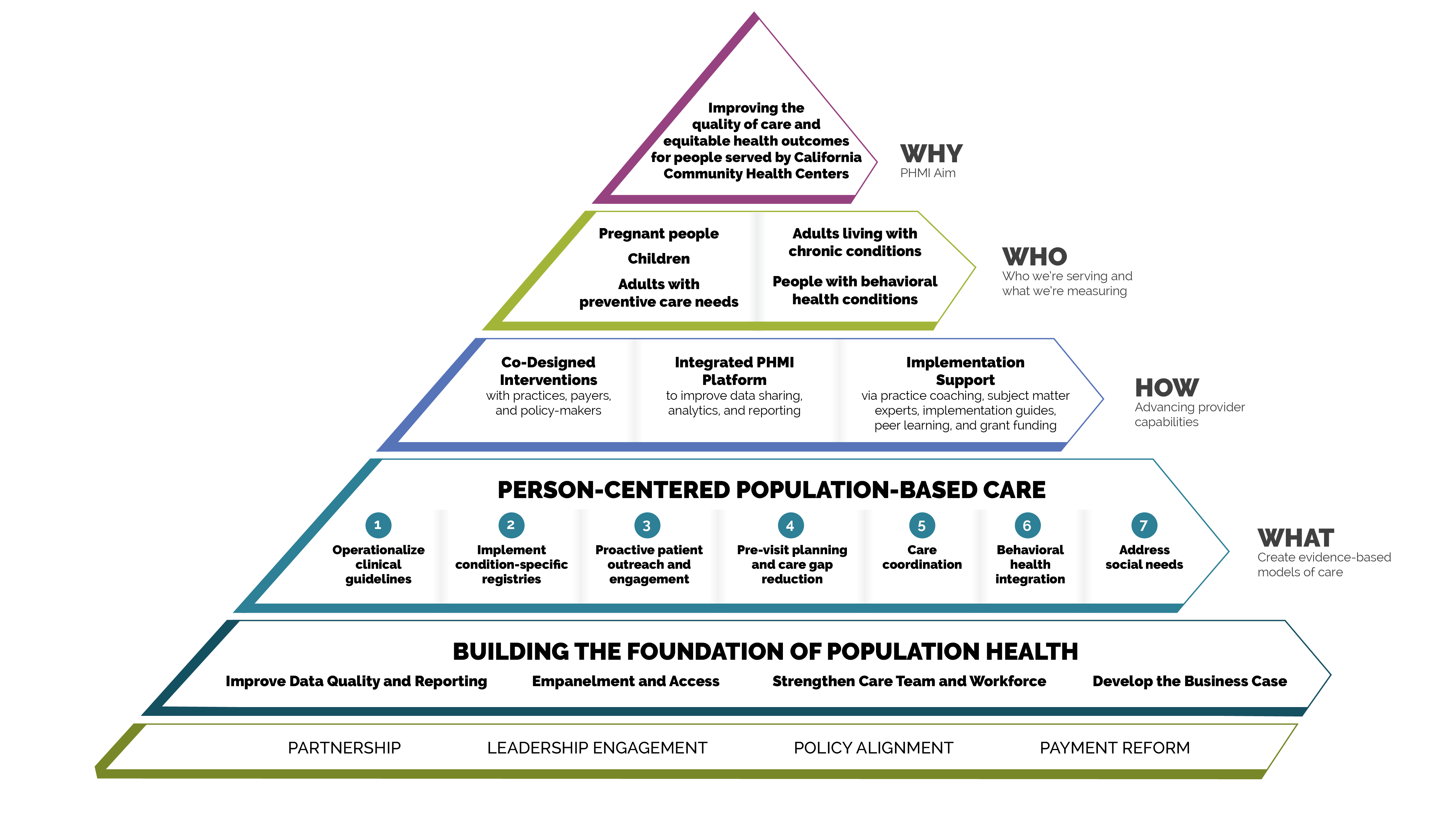
Person-centered population-based care
Each of the key activities advance one or more of the seven person-centered population-based care change concepts:
- Operationalize clinical guidelines.
- Implement condition-specific registries.
- Proactive patient outreach and engagement.
- Pre-visit planning and care gap reduction.
- Care coordination.
- Behavioral health integration.
- Address social needs.
FIGURE 1: PHMI IMPLEMENTATION MODEL
The measures covered in this guide consist of Healthcare Effective Data and Information Set (HEDIS) measures designated as core and supplemental measures by the Population Health Management Initiative (PHMI). All measures use standard HEDIS definitions and are aligned with California Advancing and Innovating Medi-Cal (CalAIM) and Alternative Payment Methodology (APM 2.0). For information about these measures, reference the Data Quality and Reporting Guide.
PHMI selected a few core and supplemental measures of focus for this population, though practices can track others that feel important and relevant. This guide provides detailed guidance to improve your practice’s results on the following two core measures and three supplemental measures for adolescents and families:
- Childhood Immunization Status (core measure).
- Well-child Visits in First 30 Months of Life (core measure).
- Child and Adolescent Well-Care Visits (supplemental measure).
- Immunization for Adolescents (Combo 2) (supplemental measure).
- Well-child Visits in First 30 Months of Life (15 to 30 months) (supplemental measure).
CORE HEDIS MEASURES FOR PHMI
PHMI Population of Focus |
Measure |
|---|---|
Children |
Childhood Immunization Status Percentage of two-year-old children who have received the 10 reported vaccines* *As of October 2023, there are 11 recommended vaccines. However, the RSV vaccine has not yet been incorporated into HEDIS measures. |
|
Well-Child Visits in First 30 Months of Life Percentage of children who have had six or more well-child visits in their first 15 months of life. |
SUPPLEMENTAL MEASURES FOR PHMI
PHMI Population of Focus |
Measure |
|---|---|
Children |
Child and Adolescent Well-Care Visits Percentage of children three to 21 years of age who received one or more well-care visits with a primary care practitioner or an OB/GYN practitioner during the measurement year. |
|
Immunization for Adolescents (Combo 2) Percentage of adolescents 13 years of age who had one dose of meningococcal vaccine, one Tdap vaccine and the complete human papillomavirus (HPV) series (i.e., two doses separated by 6-12 months) by their thirteenth birthday. |
|
|
Well-Child Visits in First 30 Months of Life (15 to 30 months) Percentage of children who turned 30 months old during the measurement year, and had at least two well-child visits with a primary care physician in the last 15 months. |
The core and supplemental measures are part of a larger measurement strategy and learning system, as outlined in Appendix A: Sample, Idealized System Diagram: Weaving Your Measurement Strategy and Learning System into Practice Operations. Key Activity 1: Convene a Multidisciplinary Implementation Team Focused on Pediatrics outlines how your practice can develop a robust measurement system to support this work. In addition to quality assurance and monitoring, these measures are also used during practice operations alongside other data for learning to:
- Guide the actions of the multidisciplinary implementation team as they use a systematic approach to decreasing inequities and support implementing key activities across the practice.
- Support the individual care team’s efforts to advance population health and reduce care gaps through daily, weekly and monthly workflows, as well as continuous identification of opportunities for improvement.
The PHMI Clinical Guidelines Advisory Group (CGAG) was established to create a standardized approach to review, adopt and promote established clinical guidelines in the PHMI cohort. For pregnant people, guidance includes prenatal care initiation and prenatal and postpartum depression. For more information, please see the Clinical Practice Guidelines for Key Medi-Cal Populations of Focus.
FIGURE 2: CLINICAL GUIDELINES: WELL-CHILD VISITS IN FIRST 30 MONTHS OF LIFE (FIRST 15 MONTHS)
Guideline source |
|
PHMI measure |
Well-Child Visits in First 30 Months of Life (First 15 Months) |
Definitions |
Well-child visit (WCV): The WCV must occur with a primary care provider (PCP), but that PCP does not have to be the practitioner assigned to the child. Documentation includes all five of the following components:
|
Guideline language |
Conduct WCVs as a newborn; at three to five days old; by one month; and then at two, four, six, nine, 12 and 15 months. If a child comes under care for the first time at any point on the schedule, or if any items are not accomplished at the suggested age, the schedule should be brought up to date at the earliest possible time. |
FIGURE 3: CLINICAL GUIDELINES: CHILD AND ADOLESCENT WELL-CARE VISITS
Guideline source |
|
PHMI measure |
Child and Adolescent Well-Care Visits |
Definitions |
Well-child visit (WCV): The well-care visit must occur with a PCP or an OB/GYN practitioner, but the practitioner does not have to be the practitioner assigned to the individual. Documentation includes all five of the following components:
|
Guideline language |
Conduct annual well-care visits for persons three to 21 years of age. |
FIGURE 4: IMMUNIZATIONS FOR ADOLESCENTS
Guideline Source |
Centers for Disease Control and Prevention/Advisory Committee on Immunization Practices (2024) |
PHMI Measure |
Immunizations for Adolescents (IMA) |
Guideline Language |
|
Many key activities in this guide include considerations for utilizing the intervention to improve equitable health outcomes and reduce the effects of racism, bias and discrimination. Key Activity 4: Use a Systematic Approach to Decrease Inequities describes key action steps for how to make an intentional and explicit effort to identify inequities, understand root causes, and reduce those inequities. Refer to existing data sources and reports that illuminate existing inequities, such as the 2021 Health Disparities Report.
This guide also offers resources for going deeper into organizational and ecosystem-level work to advance equitable outcomes such as what is outlined in Key Activity 20: Strengthen a Culture of Equity. More information about this approach can be found in the PHMI Equity Framework and Approach.
Integrated behavioral health supports are important for children and their caregivers, as behavioral health support is likely to boost health outcomes and enhance patients' quality of life. One foundational change is to ensure that the care team includes behavioral health staff as core members of the team. This is covered in detail in the Care Teams and Workforce Guide.
For children, foundational key activities for integrating behavioral health include Key Activity 7: Attending to Social and Emotional Development During WCVs and Key Activity 8: Providing Dyadic Care: Screen for Postpartum Depression. Throughout these and other key activities in this guide, we have incorporated considerations for providing trauma-informed care, detailed in Key Activity 10: Implement Trauma-Informed Care Approach Across the Patient Journey. For going deeper in behavioral health integration, practices can refer to Key Activity 17: Expand Dyadic Care to Provide More Comprehensive Social and Behavioral Health Services, and Key Activity 18: Continue to Develop Referral Relationships and Pathways for specialized behavioral health services.
Of note for California Medi-Cal, there are multiple considerations and complexities in integrating behavioral health. As one example, the behavioral health benefit is divided into mild to moderate versus severe mental health conditions; the clinicians qualified and contracted to provide this care are often different. As such, early on in the behavioral health evaluation process, a clinician must decide whether a client is at the mild to moderate or severe end of the spectrum. For mild to moderate, the Medi-Cal Managed Care Plan (MCP) provides the benefit, whereas for severe, the county mental health system is responsible.
The AAP/Bright Futures recommends integrating social drivers of health into primary care to assess family access to resources necessary for optimal child development.[4] For many key activities in this guide, we have highlighted considerations related to social needs at the individual or population level, such as expanding clinic hours. A foundational activity is Key Activity 7A: Develop a Screening Process for Social Needs and Adverse Childhood Experiences (ACES) that Informs Patient Treatment Plans which can help practices better understand and support patient- and population-level needs. Practices can help patients and families and make connections to resources in the community to address issues such as childcare, parenting, legal and health education needs. For Medi-Cal patients and families with high levels of social need, such as those experiencing homelessness, referrals to Enhanced Care Management (ECM) and Medi-Cal Community Supports services are available; see Key Activity 19: Provide Care Management for more.
For going deeper in this area, practices can refer to Key Activity 18: Develop Referral Relationships and Pathways for common social needs Key Activity 15: Strengthen Community Partnerships to build upon the strengths, infrastructure and resources available in the community. More information about this dual patient- and population-level approach is available in the PHMI Social Health Framework and Approach.
Foundational Key Activities
These are the core activities that all practices must implement as part of their children’s immunization and WCV protocols.
KEY ACTIVITY #1:
Convene a Multidisciplinary Implementation Team Focused on Pediatrics
This key activity involves all seven elements of person-centered population-based care: operationalize clinical guidelines; implement condition-specific registries; proactive patient outreach and engagement; pre-visit planning and care gap reduction; care coordination; behavioral health integration; address social needs.
Overview
This activity provides guidance for developing, launching and sustaining the team or task for within your practice that will be responsible for the planning and implementation of all of the foundational key activities in this guide and overseeing related quality improvement and equity efforts, as outlined in Appendix A: Sample Idealized System Diagram.
The implementation team is so important that it appears first in our sequenced list of foundational activities. Improving your practice’s key outcomes for each population of focus and reducing equity gaps requires the aligned efforts of all care teams and nearly all functional areas of the practice, not just those working directly with patients.
This team is responsible for ensuring that the foundational key activities in this guide, including those related to screening for social needs, are implemented. As a minimum standard for screening for social needs, consider addressing social needs included in the areas recommended by the AAP/Bright Futures periodicity schedule.
In identifying potential members of this multidisciplinary implementation team, the practice should identify a diverse group of staff who are reflective of the community served and who represent the lived experience of patients. Practices may also consider mechanisms for ensuring that patients and families are informing the decisions and actions of the multidisciplinary implementation team, including but not limited to embedding patients and/or family members on the team and creating an active patient and family advisory group, all of whom are paid for their expertise and time in compliance with any relevant local, state, or federal laws and regulations.
In addition to implementing the key activity focused on applying a systematic approach to decrease health inequities, the team should apply a trauma-informed care approach and equity lens to every step outlined in this guide to help ensure that any improvements are equitably spread among the patient population. See Key Activity 10: Implement Trauma-Informed Care Approach Across the Patient Journey for further guidance. To achieve optimal functioning and impact, all members of this diverse multidisciplinary team should have their perspectives proactively included.
Relevant health information technology (HIT) capabilities to support this activity include care guidelines, registries, clinical decision support, care dashboards and reports, quality reports, outreach and engagement, and care management and care coordination (see Appendix D: Guidance on Technological Interventions). To enable team coordination, thought must be given to how to access relevant technology and how data is consistently captured, can be distributed, integrated into workflows, and how data is accessible across team members. Where possible, it is desirable to avoid duplication of data entry, siloing of information in standalone applications and databases, and the need to work in multiple applications requiring separate login.
Action steps and roles
1. Develop a time-limited group of leaders within the practice to start this process.
Suggested team member(s) responsible: Chief medical officer or equivalent and office manager or quality improvement (QI) coordinator.
Start with a small group of leaders from your practice, some of whom will be on the implementation team. These people will help refine the charge or scope of work of the implementation team and identify and engage the people and roles that will be required to implement the scope of work of the team.
2. Develop a preliminary scope of work or charge outlining the responsibilities of the implementation team.
Suggested team member(s) responsible: Time-limited group of practice leaders.
This scope or charge includes (but may not be limited to) enabling, aligning, leveraging and supporting the planning and implementation of all foundational key activities in this implementation guide so that the practice meets the foundational competencies.
However, there may be further foundation building work needed at your practice in order for you to succeed at the above key activities. The Population Health Management Capabilities Assessment Tool (PhmCAT) is a multidomain assessment that is used to understand current population health management capabilities of primary care practices. This self-administered tool can help your practice identify opportunities and priorities for improvement.
If your practice has not scored high in the domains of leadership and culture, the business case for population health management, technology and data infrastructure, or empanelment and access, consider implementing the activities listed in the four guides on Building the Foundation before or in parallel to working on key activities related to pediatrics.
3. Identify leadership and key actors for the implementation team.
Suggested staff responsibilities: Time-limited group of practice leaders.
The multidisciplinary implementation team should include those empowered to make changes in workflows, policies and staff assignments. They should be respected influencers in the organization (early adopters) who can also guide the change management process.
- Appoint a champion or lead person (e.g., pediatric prevention coordinator) to oversee the implementation and coordination of the team.
- Identify key actors who will be the core members of the implementation team. This could include a core team and an expanded team. Potential members include.
- Pediatricians.
- Medical assistants.
- Panel managers.
- Quality improvement lead.
- Community health workers and other community outreach staff.
- A member of the information technology (IT) or electronic health record (EHR) team (as part of the expanded team).
- Billing manager or similar (as part of the expanded team).
- A data lead.
- A frontline staff member who interfaces with patients by phone and at check in.
- Invite identified people to become part of the implementation team and ensure that they have designated time for their participation.
4. Launch the implementation team and set it up for success.
Suggested team member(s) responsible: Clinical coordinator or chief operating officer (COO) or chief medical officer (CMO).
This work includes:
- Ensuring that the team understands their charge or scope of work and developing a outlining this work: see the Multidisciplinary Implementation Team Charter Template.
- Defining roles and responsibilities, including the anticipated commitment (in hours) on a monthly basis.
- Establishing a meeting structure, file structure and communications structure to support effective, efficient work.
- Dedicating time and effort to forming, storming, norming and performing as a team. The Team Communication and Working Style Template is one tool that team members can complete and share with other teammates to accelerate this process.
- Understanding baseline data related to outcomes of interest (e.g., baseline immunization rates, baseline well-child visit completion rates), along with data related to known and perceived barriers to these outcomes.
- Prioritizing elements within the scope of work, informed by baseline data and identified population needs.
- We recommend that practices consider planning and attempting to implement the activities in the sequence provided in this guide, focusing first on the foundational activities before focusing on the activities noted as Going Deeper activities. However, different practices may follow different paths toward implementation.
5. Develop a simple yet robust measurement strategy and learning system to guide your improvement efforts.
Suggested team member(s) responsible: Implementation team.
A learning system enables a group of people to come together to share and learn about a particular topic, to build knowledge, and to speed up improved outcomes. A simple yet robust measurement strategy and learning system:
- Contains a balanced set of measures looking at outcomes, processes and possibly unintended secondary effects (e.g., increased cycle time and impact on team well-being).
- Incorporates the patient perspective and the perspective of staff (front desk and others), care team members, and management.
- Allows the team to determine if the process or system has improved, stayed the same, or gotten worse.
- Helps guide improvement efforts and informs practice operations. See Appendix A: Sample Idealized System Diagram: Weaving Your Measurement Strategy and Learning System into Practice Operations for a sample system diagram for how your measurement strategy can be used to support practice operations.
Your practice should track the core and supplemental measures for childhood immunization status, well-child visits in the first 15 and 30 months of life, well-care visits, and immunizations for adolescents. These highly endorsed well-child and immunization guidelines can be considered proxy measures for outcome measures for improved child health.
In addition to the core and supplemental measures, practices should track process measures and balancing measures. Appendix C: Developing a Robust Measurement Strategy describes and defines the key milestones in the development of a robust measurement strategy, including definitions for each of these terms
Suggested process measures:
- Percentage of children zero to 30 months of age who were sent a reminder for recommended immunizations during the measurement year.
- Percentage of children five years of age who were sent a reminder for recommended immunizations during the measurement year.
- Percentage of children zero to 21 years of age who are identified as missing one or more recommended immunizations during the measurement year. For greater clarity and more actionable insights, also track completion rates by vaccination, such as:
- Percentage of children 21 months of age who are identified as missing one or more tetanus, diphtheria, acellular pertussis (Tdap) vaccines.
- Percentage of children 21 months of age who are identified as missing one or more inactivated poliovirus vaccine (IPV) vaccines.
- Percentage of children 18 months of age who are identified as missing one or more measles-mumps-rubella (MMR) vaccines.
- Percentage of children 18 months of age who are identified as missing one or more Haemophilus influenzae type b (Hib) vaccines.
- Percentage of children nine months of age who are identified as missing one or more hepatitis B (Hep B) vaccines.
- Percentage of children six months of age and older who are identified as missing the annual influenza (flu) vaccine.
Suggested balancing measures:
- One or more measures related to patient satisfaction.
- One or more measures related to staff satisfaction.
Practices can also look at other metrics to understand the progress of specific improvement initiatives over time. This may include:
- Progress on the Population Health Management Capabilities Assessment Tool (PhmCAT).
- Progress towards foundational competencies listed in this implementation guide. For example: “Yes or No: Did your practice achieve the following foundational competency: ‘Create a health-related social needs screening process that informs patients’ treatment plans.’”
- Any other care gaps, clinical guidelines or measures your practice feels are important to prioritize.
Applying an equity lens
Your practice may be achieving better outcomes with some patients than others. To understand these disparities, practices should stratify their data based on race, ethnicity and language (REAL), sexual orientation and gender identity (SOGI), and other patient characteristics (e.g., social needs, etc.). The advancing equity through data quality and reporting section of the PHMI Data Quality and Reporting Guide provides more guidance on this.
Putting it all together
We recommend that your practice record your measurement strategy in one place. This Measurement Strategy Tracker contains all the fields we believe are most useful, and it can be customized to meet your practice’s needs.
6. Plan and hold regularly scheduled meetings of the implementation team.
Suggested team member(s) responsible: Team lead or clinical coordinator or other individual tasked with coordinating the work of the team.
Hold time on team members' calendars for standing meetings. Consider biweekly (twice monthly) meetings to start with. The frequency, duration and focus of these meetings may change as you consider additional populations or subpopulations and additional sites or locations and as the nature of the work changes.
Develop a system to efficiently report on all workstreams and track follow-up items. The Action Plan Template is a tool that can be used to focus your team around the foundational competencies and define responsibility for actions and steps to be taken for each project your team has prioritized to work on.
7. Make adjustments based on data from the team’s measurement strategy and feedback loops.
Suggested team member(s) responsible: Implementation team.
Review data and feedback at least monthly, and adapt efforts as needed. Adaptation could include any or all of the following:
- Amending the charge or scope of work.
- Modifying meetings or meeting structures.
- Changing the team composition (adding or removing members).
- Refining key activities to better meet the needs of patients and practice staff, improve outcomes or reduce inequities.
- Modifying the measurement strategy and/or feedback loops to better understand what is and isn’t happening.
Create opportunities for celebrating small wins, progress and measured improvement.
On an annual basis, the team’s charter and core membership should be reviewed. As the goals of the implementation team are met, the team could disband, meet less frequently (e.g., twice per year), or fold this meeting into a similar standing meeting that occurs separately.
Resources
Health Center Quality Measurement Systems Toolkit
Health Alliance of Northern California created a summary crosswalk of measurement sets that provides an overview of alignment between measurement systems. It includes in-depth information on each Uniform Data System (UDS) or Quality Incentive Pool (QIP) clinical measure for childhood immunizations, immunizations for adolescents, well-child visits (zero to 15 months), well-child visits (three to six years), child and adolescent well care visits (three to 17 years), which are contained in a spreadsheet. The document also shares suggested clinical interventions and community interventions for childhood and adolescent immunizations status in rural northern California.
KEY ACTIVITY #2:
Assess and Improve Reliability in Meeting Well-Child Visit (WCV) Recommendations
This key activity involves all seven elements of person-centered population-based care: operationalize clinical guidelines; proactive patient outreach and engagement; pre-visit planning and care gap reduction; care coordination; behavioral health integration; address social needs.
Overview
The American Academy of Pediatrics (AAP)/Bright Futures developed a set of comprehensive health guidelines for well-child care, known as the periodicity schedule. It is a schedule of screenings and assessments recommended at each well-child visit from infancy through adolescence. Each pediatric clinic should implement protocols to ensure all recommended activities and interventions for all children and families are addressed during WCVs.
Click here for the periodicity schedule detailing recommended activities at each well-child visit.
This foundational activity deals with assessing and then improving your practice’s reliability in implementing the guidelines in periodicity schedule. Of note, a recent thoughtful article published in Pediatrics proposes a population health framework to facilitate a redesign – with emphasis on care teams – for delivering the most evidence-based dimensions of pediatric preventive care. It doesn't solely rely on the traditional WCV as the sole venue in which key preventive services are delivered. The innovation proposed in this framework may prove impactful for patients and practices; currently, however, this approach does not align with the quality measurement framework of reporting the compliance rate with annual well-child visits.
Well-care visit activities are recommended to assess and support children’s healthy development and their ability to access needed supports to achieve their best possible health and well-being. Bright Futures compiled tables of evidence and rationale describing the high degree of certainty for guidelines included in the periodicity schedule.
It is likely that the quality and reliability of the recommended WCV activities will vary across clinics. Ensuring that every child benefits from every recommended activity across their childhood is an essential goal for pediatric clinics.
Due to racism, bias and discrimination, children of color and children from families with lower socioeconomic status are less likely to complete all WCVs and therefore benefit from all WCV activities.[5][6][7][8] Ensuring that every WCV is optimized can contribute to mitigating inequities in health and well-being experienced by children based on race, ethnicity and class.
Additionally, WCVs provide an opportunity to forge healthy, positive, strengths-based relationships with children, youth and their families. A trusted, caring relationship can provide a foundation for mitigating the deleterious and harmful effects of racism, bias and discrimination.
WCVs provide an opportunity for screening for and responding to unmet social needs as well as building the trusted relationship necessary for families to disclose unmet needs. An initial minimum standard for social need screening may be guided by the Bright Futures implementation tip sheet on integrating health-related social needs.
Relevant HIT capabilities to support this activity include electronic access to care guidelines, registries, clinical decision support, care dashboards and reports, quality reports, outreach and engagement, and care management and care coordination. See Appendix D: Guidance on Technological Interventions.
Access to outside data may be a consideration or requirement (e.g., California Immunization Registry (CAIR) immunization registry data, school health data, and data from other practices) as services received outside the health center may be part of compliance. While claims data provided by payors may be helpful in this regard, lag time may impact its usefulness. Partner Medi-Cal managed care plans (MCPs) likely already do or can provide upon request reports of children who appear overdue, based on claims and encounter data, for pediatric preventive care, such as well-child visits and lead screening. Such reports may reduce the need for health centers to generate reports from raw claims data. Patient-facing applications should be strongly considered to assure that parents, caregivers and older adolescents are informed and appreciative of the nature and importance of recommended care. Confidentiality concerns and regulatory requirements protecting emancipated adolescents can be challenging, as EHRs and other technologies may not support segmentation of information. This may need to be overcome through manual workarounds and procedures
Action steps and roles
1. Review current practices to identify key opportunities for improvement.
Suggested team member(s) responsible: QI lead with frontline staff (e.g., PCP, nurse, medical assistant, front desk staff).
Using the periodicity schedule as a guide, catalog the clinic’s current practices, processes and protocols related to WCVs. Identify how current practices align with the recommendations of the periodicity table and identify top opportunities for improvement.
Consider compiling additional data to determine the rate of completion of each of the recommended activities at each WCV, even if these data are from a small sample of WCVs (e.g., the next five to 10 WCVs for 15-month-olds). Review aggregated data to identify areas of strong performance to learn from and areas for improvement to prioritize. See more in Key Activity 3: Use Care Gap Reports or Registries to Identify all Patients Eligible and Due for Care.
Opportunities for improvement may include:
- Improving scheduling and completion rates for WCVs at the recommended ages.
- Introducing a practice, process or protocol that is currently not being done at all.
- Expanding the WCVs at which a practice, process or protocol is currently being done.
- Improving the quality or reliability of a current practice, process or protocol.
Of note, one of the more challenging Bright Futures and U.S. Preventive Services Task Force (USPSTF) recommendations is the initiation of fluoride varnish after the eruption of the first primary tooth. A new HEDIS measure in 2023 for fluoride varnish reads, “The percentage of members one to four years of age who received at least two fluoride varnish applications during the measurement year.” While federally qualified health centers (FQHCs) with colocated dental clinics may have additional resources and flexibility regarding integration of this key pediatric preventive service, practices without colocated dental clinics may need to employ new strategies.
2. Test new and adapted practices and processes to develop improved workflows and standard protocols for implementing recommended activities during WCVs, focusing first on prioritized areas for improvement.
Suggested team member(s) responsible: QI lead with frontline staff, as appropriate for the WCV activity of focus; patients and their families.
Consider how to use registries, the pre-visit planning process, and daily huddles to support this key activity. (Note: Other key activities are included in this guide to support these aspects.) Use the individual WCV resource pages at AAP Schedule of Well-Child Care Visits – HealthyChildren.org to design, organize and improve each WCV. Consider how to integrate a trauma-informed approach as your practice creates and tests new or adapted processes and enlist caregivers as partners in ensuring WCV activities are provided on time. HealthyChildren.org provides a caregiver-friendly version of the AAP Schedule of Well-Child Care Visits that clinics can share with parents so they know what to expect.
3. Continuously improve approach to WCVs, both overall and for key subpopulations.
Suggested team member(s) responsible: QI lead with frontline staff, as above.
Track data on completion of WCVs in real time and collect disaggregated data by race and ethnicity, as well as by language spoken and geographies, whenever possible. Advocate for strategies that address the challenges specific to subgroups, particularly those with low WCV completion rates, to drive optimal WCVs for all children and families. See more in Key Activity 10: Implement Trauma-Informed Care Approach Across the Patient Journey and Key Activity 4: Use a Systematic Approach to Decrease Inequities.
Implementation tips
Below are examples of quality improvement efforts to improve reliability of meeting WCV recommendations:
- Sonoma Valley Community Health Center created a training booklet to both train new staff and act as a reference guide for existing staff. Updated annually, it contains many of the health center’s key workflows, including childhood immunizations.
- Shasta Community Health Center conducted an improvement project centered around increasing the rate of pediatric patients who leave an acute care visit with a scheduled well child visit from the baseline of 30%.
- Marin Community Clinics undertook a multipronged improvement effort for completing required immunizations for all patients by their second birthday by creating a culture of vaccinations at the practice.
- Hill Country Health & Wellness Center conducted a quality improvement project where they tested a new workflow for Childhood Health and Disability Prevention (CHDP) visits with one provider to optimize the use of provider time by segmenting the 40-minute appointment slot into two sessions. The first 20 minutes is with the licensed vocational nurse (LVN) or registered nurse (RN) for education, and the remaining 20 minutes is with the provider. This change was designed to increase access to well-child visits and deliver education on immunizations, thereby increasing immunization rates according to accepted periodicity schedules.
KEY ACTIVITY #3:
Use Care Gap Reports or Registries to Identify All Patients Eligible and Due for Care
This key activity involves all seven elements of person-centered population-based care: operationalize clinical guidelines; implement condition-specific registries; address social needs.
Overview
This foundational activity provides detailed guidance on how to reliably and efficiently develop and use a regularly updated list of all patients eligible for recommended or standard screenings or interventions through a care gap report or registry.
Care gaps are gaps between the recommended care that a patient should receive according to clinical guidelines and protocols and the care a patient has actually received. Rather than put the responsibility on the individual care team member for searching through charts or remembering which patients need further preventive care or follow-up, this key activity provides guidance for how the practice can efficiently leverage electronic health records (EHRs) and other applications or technical approaches for all its patients.
Care gap reports are essential for practices to understand and continually improve consistency and reliability for meeting guidelines for preventive care. At the care team level, care gap reports focus on gaps for patients assigned to your care team and help your team understand which patients you are responsible for. These lists can be used to:
- Support improvements to the pre-visit planning process, develop standing orders, and improve other routine clinical workflows designed to systematically identify and address gaps in care.
- Prioritize patients for whom care teams should provide proactive outreach and reminders for engaging in care.
- Support quality improvement efforts with an equity lens.
Actively identifying and acting on care gaps ensures all eligible patients assigned to your practice receive timely screenings and other preventive services.
Many practice patients and families experience barriers in accessing care due to structural and historical racism, homophobia, xenophobia, and other biases that have historically disadvantaged individuals and groups from receiving equitable services. Defining clear criteria and gaps for patients due for specific screenings or preventive services helps to illuminate groups who have not had equitable access. It also combats biases by standardizing expectations for what constitutes quality standards of care for all clients.
Staff can identify potential barriers to patients accessing and engaging in care by using enhanced care gap reports to filter and display the data alongside demographic information, social needs, behavioral health needs, and communication preferences. This information can be incorporated into a person-centered approach when designing the care plan, promoting self-care and other patient engagement activities, such as conducting outreach in the patients’ preferred language. Adopt a trauma-informed approach when designing, testing and implementing interventions to address potential barriers and gaps in care.
Furthermore, care gap reports that segment the data into cohorts based on demographic and other personal information may help the team identify disparities in care, access and outcomes, which can inform improvement efforts.
Care gap reports can be used during pre-visit planning to identify people for whom social needs screening has not yet been completed. This creates an opportunity to identify unmet social health needs and connect patients with resources that address their social needs.
Many EHRs already have a module that identifies what services are due for each patient, while others do not. Where this functionality is available, it may not be configurable to align with the health center’s specific protocol or be able to incorporate outside data. Other options for developing registries include supplemental applications, population health platforms, and freestanding customized databases that draw data from the EHR and other sources. A comprehensive approach to the use of care gap reporting may require multiple modalities.
A registry can be thought of simply as a list of patients sharing specific characteristics that can be used for tracking and management.
Care gap reports may be embedded in electronic health records or made available through other technology channels (see Appendix D: Guidance on Technological Interventions) and are useful both at the individual patient level and aggregated to identify groups of patients to facilitate population-level management through registries.
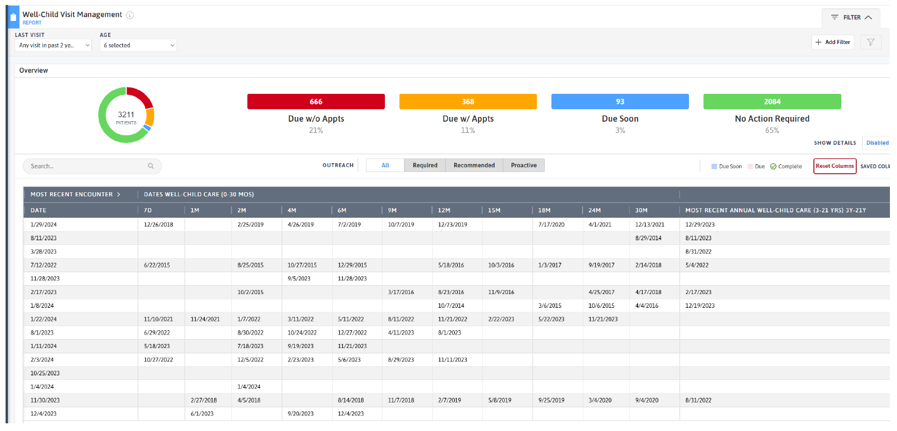
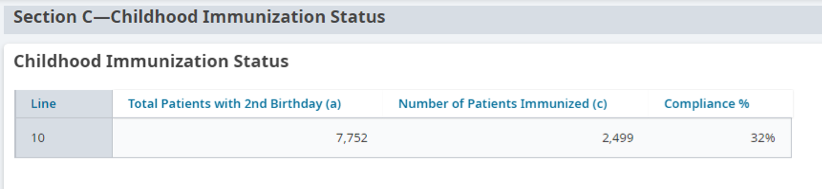
Figure 4, Figure 5 and Figure 6 provide an example of a care gap report for immunizations and well-child visits.
Other relevant HIT capabilities to support and relate to this activity include care guidelines, care dashboards and reports, quality reports, outreach and engagement, and care management and care coordination.
See Appendix D: Guidance on Technological Interventions.
Access to outside data may be a consideration or requirement (e.g., CAIR immunization data, school health data, and data from other practices) as services received outside the health center may be part of compliance. While claims data may be helpful in this regard, lag time may impact its usefulness. Patient-facing applications should be strongly considered to assure they are informed and appreciative of the nature and importance of recommended care. In California, many healthcare organizations are required or have chosen to participate the in California Data Exchange Framework (DxF), which can facilitate data sharing between clinics, MCPs and other partners.
FIGURE 4: EXAMPLE IMMUNIZATION CARE GAP REPORT FOR AN INDIVIDUAL PATIENT
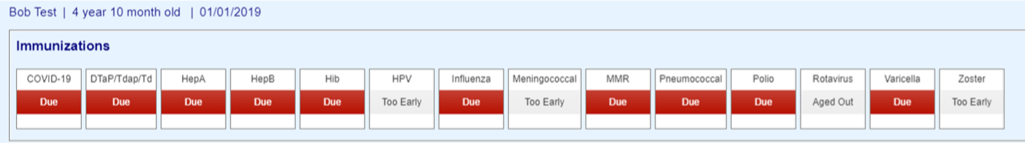
FIGURE 5: EXAMPLE IMMUNIZATION CARE GAP REPORT FOR A PANEL OF PATIENTS UNDER TWO YEARS OF AGE
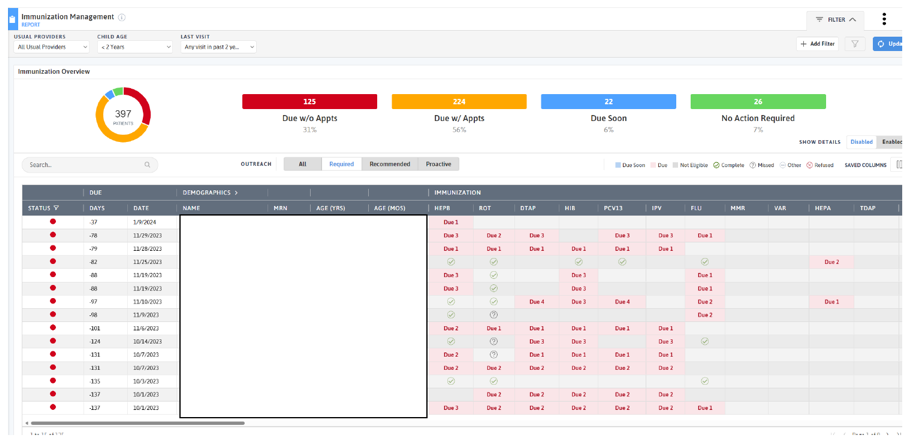
FIGURE 6: EXAMPLE WCV CARE GAP REPORT FOR A PANEL OF PATIENTS
Action steps and roles
1. Plan the care gap report.
Suggested team member(s) responsible: Panel manager or data analyst. If it is not clear how the report can be produced, this step may involve one or more people from the practice who work on the EHR and, possibly, the EHR vendor.
As a team, decide what screenings or treatment guidelines are appropriate for your patients and prioritize the most important care gaps to run reports on. Start with the core and supplemental measures and any process measures your practice is tracking. Create care gap reports for childhood immunizations and recommended or standard well-child visits based on the Bright Futures periodicity schedule. Consider if there are any other gaps, clinical guidelines or measures your practice feels important to prioritize. See the Pre-Visit Planning: Leveraging the Team to Identify and Address Gaps in Care for a more complete list of preventive and health maintenance guidelines to consider.
Identify the inclusion criteria for each report, such as age, any exclusion criteria, and factors that make someone high risk.
For more information about California immunization requirements for school entry across childhood and adolescence, refer to Shots for School by the California Department of Public Health (CDPH). Initial efforts to develop care gap reports could focus on ensuring that pediatric patients are receiving these required immunizations.
Childhood immunizations are also tracked in the California Immunization Registry (CAIR). CAIR can link into your EHR to provide more up-to-date information for immunizations your patients received at community pharmacies or other health facilities. See Key Activity 2: Assess and Improve Reliability in Meeting Well-Child Visit (WCV) Recommendations for other tips on implementing these protocols.
2. Build the report.
Suggested team member(s) responsible: Data analyst.
Determine whether the EHR has an existing report or one that can be modified to fit the inclusion criteria. You should talk to staff who are familiar with the electronic record; in some cases, it may be necessary to consult with the EHR vendor to confirm this information and how to run the report.
The care gap format should include:
- Criteria for inclusion in the report.
- The overall compliance rate for the care gap being measured.
- All patients eligible for the screening and their addresses and phone numbers.
- The last date the screening or service was provided (if known or if applicable), the previous results, and the type of assessment used.
- Preferred method of communication (e.g., phone, email, text).
Reports should be able to display and/or disaggregate the data based on:
- Race, ethnicity and language (REAL) as well as sexual orientation and gender identity (SOGI).
- Any known social or behavioral needs.
- Communication preferences or other preferences that would inform the screening modalities offered, such as documented declination of prior screenings.
- Data on any other characteristic, including insufficient insurance coverage, that could pose a barrier to completing screening.
3. Standardize the data format.
Suggested team member(s) responsible: Panel manager and care team.
Standardizing the data format and where it is entered is critical to ensuring accuracy in the resultant report. Once you know that a report can be produced, understand the specific data elements that are needed to produce the reports.
Document how each data element must be entered into the EHR in order to populate the fields needed for reporting. In some cases, data on completion of screening must be entered by hand (e.g., when the test is performed by a lab that does not communicate with the legacy EHR). Doing this will require a decision on the part of the practice as a whole and may require staff training and reinforcement on an ongoing basis. Where issues or apparent confusion are identified, regular discussion at team huddles or staff meetings will help in maintaining a standard approach.
Tip: Assign responsibility for the initial review of the reports to confirm data integrity.
4. Use the care gap reports in service to other workflows and improvement activities (e.g., assess and improve reliability in meeting well-child visit recommendations).
Suggested team member(s) responsible: Panel manager or data analyst.
A few examples include:
- At the patient level, the care gap report can be used for or linked with reminders or alerts for clinicians, as well as for sending reminders to patients who need to come into the clinic for screening or follow-up.
- Depending on communication preferences that have been expressed by patients, the patient care gap report may be exported to an automated reminder system that can trigger reminders by phone, text, email or mail.
- As part of the practice’s preplanning process, patient care gaps could be reviewed as part of the daily huddle. See Key Activity 5: Develop or Refine and Implement a Pre-visit Planning Process for more details.
FIGURE 7: EXAMPLE POPULATION CARE GAP REPORT ON IMMUNIZATION STATUS
5. Monitor the care gap report for accuracy and completeness.
Suggested team member(s) responsible: Panel manager or data analyst.
It is critical to have bidirectional feedback with the practice’s care team about any real or potential errors in the care gap report, such as:
- Errors in how the data is entered compared to what is required under the new standardized data format.
- Patients who are eligible for and due for screening who are missing from the report.
- Patients who have recently been screened who are still listed as due for a screening.
Errors should be investigated through a chart review. If errors in the report specifications are discovered, the care gap report or process for producing the report should be modified. If the issue is incorrect documentation, staff training and reinforcement of documentation standards will be required.
Additional consideration for sustainability: Ensure there is an internal process for updating the criteria included in the EHR for care gap reports as clinical guidelines change.
Resources
KEY ACTIVITY #4:
Use a Systematic Approach to Decrease Inequities
This key activity involves all seven elements of person-centered population-based care: operationalize clinical guidelines; implement condition-specific registries; proactive patient outreach and engagement; pre-visit planning and care gap reduction; care coordination; behavioral health integration; address social needs.
Overview
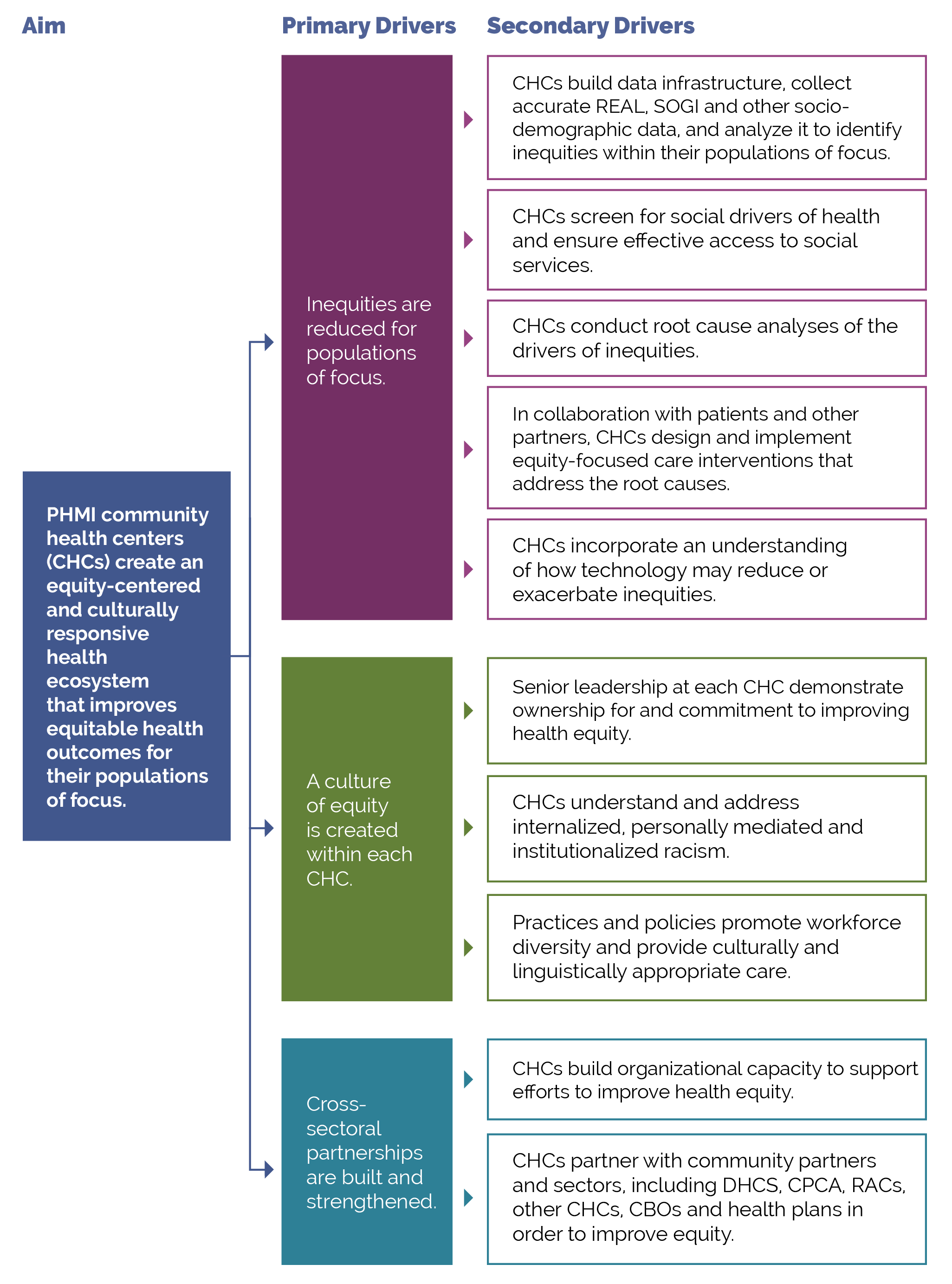
This activity provides guidance for a systematic evidence-based approach for identifying and then reducing inequities for children. It focuses on the first primary driver in PHMI’s equity approach: Reduce inequities for populations of focus.
FIGURE 8: PHMI EQUITY DRIVER DIAGRAM
As with virtually any clinical outcomes, your practice is likely achieving better outcomes with certain populations or subpopulations and worse outcomes with others. Inequitable outcomes are generally most acute among persons of color, immigrants, persons speaking a primary language other than English, and other populations who have been marginalized. As we work over time to reduce and eliminate inequitable health outcomes, we need to understand both what contributes to these different outcomes as well as factors that do not contribute to them.
This includes recognizing that race is a social construct determined by society’s perception. While some conditions are more common among people of certain heritage, disparities in conditions such as cancer, diabetes and adverse maternal outcomes have no genetic basis. While genetics do not play a role in these inequitable outcomes, the extent to which inequities in the quality of care received by people of color contribute to inequitable health outcomes has been extensively documented.[9] These inequities are often a direct result of racism, particularly institutionalized racism – that is, the differential access to the goods, services and opportunities of a society by race.[10] Racial health inequities are evidence that the social categories of race and ethnicity have biological consequences due to the impact of racism and social inequality on people’s health.[11] It is also critical to recognize that we have policies, systems and procedures that unintentionally cause inequitable outcomes for racial, ethnic, language and other minorities, in spite of our genuine intentions to provide equitable care and produce equitable health outcomes.
Improving your practice’s key outcomes for children requires a systematic approach to identifying equity gaps (e.g., who your practice is not yet achieving equitable outcomes for) and then using quality improvement (QI), collaboratively design, systems thinking and related methods to reduce these equity gaps. This effort will be more effective if it is guided by a theory of change that addresses the ways in which structural and institutional racism lead to inequities in care provision. For more discussion, read resources such as this one from the Center for American Progress on how structural and institutional racism contributes to declining childhood immunizations rates.
Identifying and meeting patients’ social health needs is a key driver of reducing inequitable health outcomes. We provide additional guidance in this key activity on how to both reduce inequities and meet patients’ social health needs.
Access to data required to identify and monitor inequities as outlined in the key actions outlined below is fundamental to this activity.
Relevant HIT capabilities to support this activity include care guidelines, registries, clinical decision support (modifications required to consider disparate groups), care dashboards and reports, quality reports, outreach and engagement, and care management and care coordination (See Appendix D: Guidance on Technological Interventions).
EHRs have the ability to capture basic underlying socioeconomic, SOGI and social needs-related data but may in some cases lack granularity or nuances that may be important for subpopulations. Mismatches between how UDS captures REAL data versus how EHRs capture or MCPs report data can also create challenges. This may require using workarounds to capture these details. It is also important to assure that other applications in use, which may have separate patient registration processes, are aligned. Furthermore, tracking inequities in accessing services not provided by the health center may also require attention to data sources or applications outside the EHR.
In the pediatric population, some of the contributing data may pertain to the parent or caregiver. For example, children’s risk of experiencing chronic disease is associated with maternal health conditions including asthma, obesity and mental distress.[12] Where possible and relevant, comprehensive strategies might include ability to draw such data into analyses and reports.
Health centers should also be alert to the potential for technology as a contributor to inequities. For example, patient access to telehealth services from your practice may be limited by the inequitable distribution of broadband networks and patient financial resources (e.g., for phones, tablets, and cellular data plans). EHR-embedded algorithms used to stratify populations by risk may also contain inherent racial biases. The Techquity framework can be a useful way to structure an approach to assure that technology promotes rather than exacerbates disparity.
Language, literacy levels, technology access and technology literacy should also be considered and assessed against the populations served at the health center.
Finally, attention needs to be paid to the use of best practices in collecting the data, accurate categories in the technologies in which it is collected and stored, and adequate training and monitoring of staff responsible in order to assure reports and analysis have a valid basis.
Action steps and roles
1. Build the data infrastructure needed to accurately collect REAL, SOGI and other demographic data.
Suggested team member(s) responsible: Data analyst.
The PHMI Data Quality and Reporting Guide provides guidance and several resources for collecting this information. According to this guide, the initial step in addressing disparities is to collect high-quality data that fosters a comprehensive understanding of each patient. This entails incorporating race, ethnicity and language (REAL) data, demographic data (age, gender) and social needs data. By leveraging this information, healthcare practices can gain valuable insights into disparities in access, continuity and health outcomes." Steps two to four below provide more information on this process.
Collecting REAL information allows for practices to identify and measure disparities in care, while also ensuring that practices are able to interact successfully with patients. This is done by understanding their unique culture and language preferences.[13] KHA Quality has a toolbox that assists with REAL data collection.
The Uniform Data System (UDS) Health Center Data Reporting Guidance (2023 Manual) provides detailed guidance on REAL and sexual orientation and gender identity (SOGI). Note: While UDS does not currently require that practices report on the specific primary language of each patient, practices should make an effort to identify and record each patient’s primary language, as UDS reporting still requires for languages other than English to be reported.
Accurate collection of data requires appropriate fields and options in the EHR and other employed technologies, as well as appropriate human workflows in collecting the data. Staff responsible for data collection should be continuously trained and assessed for best practices in data collection, including promotion of patient self-report.
In addition, practices should work to ensure that patients understand the importance and use of this information to help them feel comfortable supporting its collection. Example language can be found at The MGH Disparities Solution Center. High rates of “undetermined” or “declined” in these fields may be indicative of the need to attend to these staff training needs.
Collecting this data is important, especially to obtain a complete picture of health for patients who identify as transgender. There are certain risks and condition indicators that are gender-specific, which impact how care teams provide care to a patient. By understanding the needs of patients more fully, care teams can make more informed decisions for the best treatment of their patients. The World Professional Association for Transgender Health (WPATH) has provided further guidance regarding standards of care related to gender diversity.
2. Use the practice’s EHR and/or population health management tool to understand inequitable health outcomes at your practice by stratifying your data.
Suggested team member(s) responsible: Data analyst.
This includes reviewing your care gap report or care registry and being able to stratify all of the following:
- Core measures for the population of focus.
- Supplemental measures for the population of focus.
- Process measures for the population of focus.
Stratify this data by:
- Race, ethnicity and language (REAL).
- Sexual orientation and gender identity (SOGI), when possible.
- Other factors that can help identify subpopulations in need of focused intervention to reduce an equity gap (e.g., immigrants, people experiencing homelessness, etc.).
This is not a one-time event, but rather a continuous process (see step 13 below) and should be done in tandem with step three below.
Consider reviewing data on disparities at the state and health plan level for greater context.
You might not have enough sample size in some REAL categories to identify whether a trend is significant or not. If you’re seeing something in your patient population, you can examine other known data sources, such as a recent state health disparities report, for context.
3. Screen patients for social needs.
Suggested team member(s) responsible: Care team.
Key Activity 7A: Develop a Screening Process for Social Needs and Adverse Childhood Experiences (ACESs) that Informs Patient Treatment Plans provides guidance on screening patients for health-related social needs and how the information can begin to be used to inform patient treatment plans, including referral to community-based services. This is not a one-time event, but rather a continuous process and should be done in tandem with step two above.
4. Analyze the stratified data from steps two and three to identify patterns of inequitable outcomes.
Suggested team member(s) responsible: Data analyst, QI leads, care team.
Analyze the stratified data from steps two and three to identify patterns in inequitable outcomes.
This includes:
- Utilizing tools to examine, visualize and understand disparities across different populations or subpopulations.
- Data over time (using run charts).
- Exploring trends, patterns and significant differences to understand which demographic groups will require a focused effort to close equity gaps.
Update your practice’s measurement strategy so your practice’s improvement efforts remain centered around advancing equitable outcomes. Some examples include creating specific, measurable, achievable, relevant, time-bound, inclusive and equitable (SMARTIE) goals and updating your process and outcome measures so you can understand differences by REAL or SOGI indicators. See Appendix C: Developing a Robust Measurement Strategy for more.
This is not a one-time event but rather a continuous process (see step 13 below). Periodic review of stratified data allows for recognition of gap closures and emergence of new disparities.
5. Use a root cause analysis to identify improvement approaches for subpopulations with lagging health outcomes.
Suggested team member(s) responsible: Implementation team.
Select root cause analysis approaches that work best for the equity gap you are closing:
- Engage and gather information from patients affected by the health outcome in your root cause analysis (see step six).
- Brainstorming.
- Systems thinking (understanding how interconnected social, economic, cultural and healthcare access factors may be impacting the health outcome).
- Tools that rank root causes by their impact and the feasibility of addressing them (e.g., prioritization matrix and/or an impact effort matrix).
- Visual mapping of root causes and effects (e.g., fishbone diagram).
- Perform focused investigations into selected root causes, gathering qualitative data through interviews, surveys or focus groups with the subpopulation of focus.
Present the findings to a broader group of stakeholders to validate the identified root causes and gain additional insights. Incorporate their feedback and refine the analysis, as needed.
6. Partner with patients to build successful strategies addressing inequitable outcomes.
Suggested team member(s) responsible: Care team and people with lived experience (patients representative of the population(s) of focus).
Using one or more human-centered design methods, such as focus groups, Journey Mapping, etc. (see links to these methods below), and engage patients to better understand perspectives that may influence the health outcome of interest. This may include collecting information on:
- Their assets, needs and preferences.
- Cultural beliefs, including traditional healing practices.
- Level of trust in healthcare generally and in the topic of focus specifically (e.g., immunizations, behavioral health, etc.).
- Barriers to accessing care.
- Barriers to remaining engaged in care.
- Trusted sources of information or communication mechanisms for this population.
- Their ideas for improving health outcomes.
The patients you partner with for this and other steps in this key activity may be part of a formal or informal patient group and/or identified and engaged specifically for this equity work. Fairly compensating patients for participating in improvement activities is a best practice.
Selected resources on human-centered design and collaboratively design:
- Center for Care Innovations (CCI) Human Centered Design Curriculum via CCI Academy.
- IDEO’s Field Guide to Human-Centered Design.
- IDEO’s Design Kit: Methods.
7. Develop strategies that address or partially address the identified equity gaps.
Suggested team member(s) responsible: Care team and people with lived experience.
Based upon the insights your practice has developed for a population of focus and your root cause analysis, determine which of the key activities this guide could address or partially address the equity gap.
Most of the activities in this guide either explicitly address an equity challenge or can be adapted to better address an equity challenge. Examples of activities that can be adapted to reduce identified equity gaps include but are not limited to:
- Key Activity 9: Proactively Reach Out to Patients Due for Care.
- Key Activity 7A: Develop a Screening Process for Social Needs and Adverse Childhood Experiences (ACEs) that Informs Patient Treatment Plans, such as providing a referral for one of the Medi-Cal Community Supports.
- Key Activity 11: Coordinate Care.
- Key Activity 15: Strengthen Community Partnerships.
If one or more of your root causes cannot be addressed fully through key activities in the relevant implementation guide, use one or more human-centered design methods to develop ideas to improve health outcomes and reduce inequities among this population.
Developing these ideas is best done with representatives of the population of focus, as they have expertise and experience that may be missing from the practice's care team. During this brainstorm, you are developing ideas without immediate judgment of the ideas in an effort to generate dozens of potentially viable strategies.
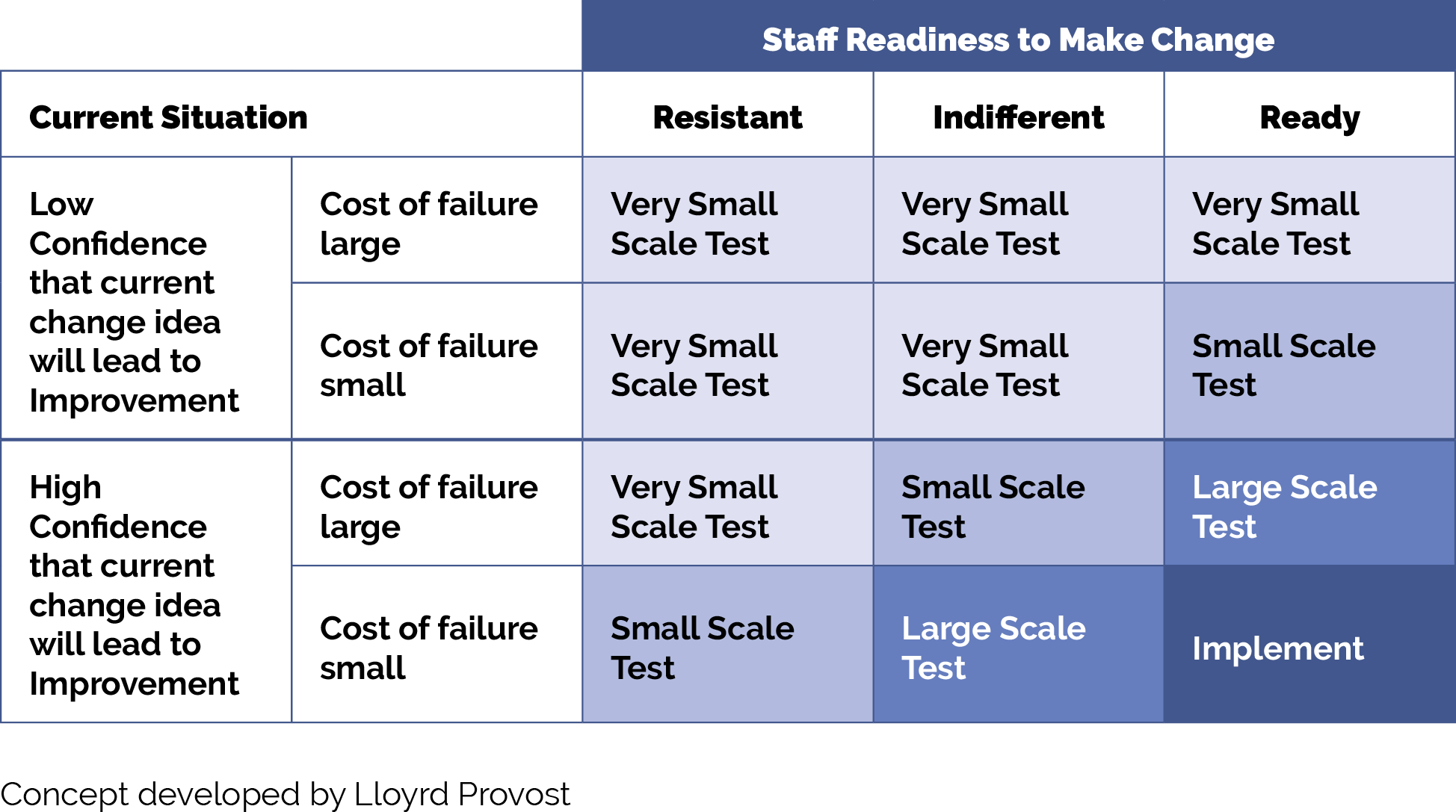
8. Determine which strategies to test first.
Suggested team member(s) responsible: Care team and people with lived experience.
There are many ways to prioritize ideas. The Institute for Healthcare Improvement (IHI) often recommends a prioritization matrix and/or an impact effort matrix and offers a video on making them.
If you have organized your key activities and new ideas into themes or categories, you may choose to work on one category or select one or two ideas per category to work on.
The number of key activities and/or new ideas that you prioritize for testing first should be based on the team’s bandwidth to engage in testing. It is critical to determine the bandwidth for the team(s) who will be doing the testing so that you can determine how many ideas to test first.
9. Use quality improvement (QI) methods to begin testing your prioritized key activities and new ideas.
Suggested team member(s) responsible: Care team and people with lived experience.
Nearly all the key activities and all of your new ideas will require some degree of adaptation for use within your practice and to be culturally relevant and appropriate to your patient population.
Use plan-do-study-act (PDSA) cycles, generally starting as small as feasible. Think “ones” (e.g., one clinician, one hour, one patient, etc.) and become larger as your degree of confidence in the intervention grows.
Whenever testing a key activity or new idea, we recommend that the practice:
- Use plan-do-study-act (PDSA) cycles to test your ideas and bring them to scale. See more information on PDSAs below in the tips and resources section.
- Generally, start with smaller scale tests (e.g., test with one patient, for one afternoon, in a mailing to 10 patients, etc.). Use the chart titled “How Big Should My Test Be?” below in the tips and resources section to help you decide what size test is most appropriate.
Develop or refine your learning and measurement system for the ideas you are testing. A simple yet robust learning and measurement system will help you understand improvements, unintended secondary effects, and how implementation is going.
By working out the inevitable challenges in the idea you are testing using a smaller scale PDSA cycle, the improvement activity will ultimately work better for patients and be less frustrating to the care team. Testing and refining also can eliminate inefficient workarounds that occur when a new process or approach is imposed onto an existing system or workflow.
Select resources on quality improvement (QI):
- Institute for Healthcare Improvement’s (IHI) QI Essentials Toolkit, including details on:
- Cause and effect diagrams.
- Driver diagrams.
- Failure modes and effects analysis.
- Flowcharts.
- Histograms.
- Pareto charts.
- PDSA worksheet.
- Project planning forms.
- Run charts.
- Scatter diagrams.
- IHI’s Videos on the Model for Improvement (Part one and Part two).
- Rapid Experiments to Improve Healthcare Delivery.
- CCI’s ABC's of QI via CCI Academy.
10. Implement – bring to full scale and sustain – those practices that have proven effective.
Suggested team member(s) responsible: Care team.
Once an idea has been well tested and shown to be effective, it is time for your practice to hardwire the idea, approach or practice into your daily work. Consider using the MOCHA Implementation Planning Worksheet to think through:
- Measurement.
- Ownership.
- Communication (including training).
- Hardwiring the practice.
- Assessment of workload.
Sometimes implementation may require that you update your protocol and/or policies and procedures for the populations of focus.
11. Once you have tested, refined and scaled up the initially prioritized ideas, begin testing other ideas.
Suggested team member(s) responsible: Care team and people with lived experience.
This might include going back to the ideas developed previously but not prioritized and/or going back through the testing steps above to develop and prioritize new ideas and potentially for additional populations of focus.
12. Put in place formal and informal feedback loops with patients and the care team.
Suggested team member(s) responsible: Care team.
Establishing formal and informal feedback loops regarding new processes will ensure that your practice’s ideas are meeting the needs of patients and are reducing identified equity gaps. These feedback loops also ensure the changes are feasible and sustainable for your practice.
For patients, feedback loops could be created using many of the human-centered design tools used to design your improvement activity (e.g., surveys, interviews, focus groups). Feedback loops should also involve the patient satisfaction survey and grievance processes. Consider establishing a standing funded patient advisory board that is available to design, implement and evaluate all of your practice’s improvement activities.
For the care team, feedback loops might include:
- Existing or new staff satisfaction and feedback mechanisms.
- Regularly scheduled meetings and calls to obtain staff feedback on processes, methods and tools. Leverage existing meetings to mitigate staff burnout.
13. Continually analyze your data to determine if your efforts are closing equity gaps.
Suggested team member(s) responsible: Care team.
This includes regular (at least monthly) review of the key stratified measures from your measurement strategy. Share the data with patients to both show your work to decrease known equity gaps and to solicit ideas for closing them.
Implementation tips
- When testing a change idea (either a key activity or new idea) for your practice to address a known equity gap, the size of your test scope or group is critical.
- We recommend starting with a very small test (e.g., with one patient or with one clinician) or a small test (e.g., with all patients seen during a three-hour period by this clinician) unless you are certain the change idea, key activity or test will lead to improvement with little or no adaptation for your practice, the cost of a failed test is extremely low, and staff are excited to test the change idea.
- As you learn from each test what is and isn’t working, you can conduct larger scale tests and tests under a variety of conditions. While at first glance this would appear to slow down the implementation effort, starting small and working out the kinks as you progressively work to full scale actually saves time and resources and is much less frustrating for your patients and care team. The visualization below provides guidance on how big your test should be.
FIGURE 9: HOW BIG SHOULD MY TEST BE?
Resources
KEY ACTIVITY #5:
Develop or Refine and Implement a Pre-Visit Planning Process
This key activity involves all seven elements of person-centered population-based care: operationalize clinical guidelines; pre-visit planning and care gap reduction; care coordination; address social needs.
Overview
This key activity provides guidance for how the care team can effectively and efficiently embed preventive care measures into the practice’s pre-visit planning process (PVP). Pre-visit planning is typically driven by the medical assistant with help from other care team members and includes steps taken:
- At the end of the current visit to ensure the patient understands any actions they need to take and to schedule for any follow-up.
- Prior to a scheduled appointment, to scrub the chart and identify any pre-visit tasks per the pre-visit checklist.
- The day of an appointment, during the daily huddle and before the patient sees the PCP.
Approximately 80% of pediatric visits last 20 minutes or less,[14] and many patients come to these visits with multiple needs. Pre-visit planning works towards optimizing a team-based approach outside of these short primary care visits so patients receive comprehensive care in alignment with the latest clinical guidelines and their own preferences.
Pre-visit planning allows for better coordination of care. This can be particularly beneficial for patients with complex health needs, ensuring they receive comprehensive and equitable care. As your practice works to reduce any identified equity gaps, pre-visit planning is often a powerful activity for ensuring culturally relevant care as the care team partners with the patient to discuss follow-up actions.
The PVP should incorporate your practice’s process for screening and responding to social needs, including checking whether social needs screening is due. When social needs are identified the team should be clear on the pathways, both during and after visits, to address and follow up on those needs.
Pre-visit planning draws upon similar technical enablers as care gap reporting, and likewise can be facilitated at the individual patient level and at the level of groups of patients coming for care by a specific team in an appointment schedule block. The format in which planning is done needs to consider the workflow and staffing model.
Relevant HIT capabilities to support this activity include electronic access to care guidelines, registries, clinical decision support, care dashboards and reports, outreach and engagement, and care management and care coordination. See Appendix D: Guidance on Technological Interventions.
Individual patient-level pre-visit planning would optimally be enabled within the EHR, provided the EHR is able to store relevant information, such as assessments, plans, orders and notes outside of a visit note. Pre-visit planning might also include use of patient-facing applications, such as portal reminders, questionnaires and self-completed screenings and assessments, which ideally would be available to the clinician and care team in the EHR.
Engagement of the expanded care team in pre-visit planning requires access by all relevant members of the care team to contribute to and view relevant information. This may require coordination with technology additional to the EHR, such as care coordination and population management applications where relevant information might be stored.
Huddle reports, in which individual patient information can be visualized in summary views across all patients within a session, can require use of technology outside the EHR, but might also be supported by developing reports populated by data from the EHR. Ideally, internal practice and EHR data should be supplemented with external data where such information completes the patient’s current status. If such electronic access is not possible, workflow should include manual reconciliation by history from the patient.
Action steps and roles
1. Assess the current state of the pre-visit planning (PVP) process across your practice.
Suggested team member(s) responsible: Implementation team or QI team.
Understand how the process currently works, for all visit types (e.g., scheduled, same-day, virtual), in light of your practice’s performance on core and supplemental measures.
Compile existing paperwork and process documentation about each visit type into one place and talk to medical assistants and other members of the care team to understand their questions and challenges around the pre-visit planning process.
Consider making current-state process maps for each visit type that communicate the major steps in the PVP process and acknowledge pain points or kinks in the process. Pain points are places where the process isn’t working well for patients, staff, or specific subpopulations or demographic groups for which your data analysis has revealed equity gaps. These pain points also likely differ by visit type. In addition, pay attention to places where staff are creating workarounds to the process. The presence of workarounds indicate that the process might need further clarification or refinement to support the care team to reliably implement it.
Your team may find it helpful to compile process maps for both the high-level pre-visit planning, as detailed in figure 6.1 of the PHMI Care Teams and Workforce Guide Resource 6: Workflow Examples, in addition to more detailed documentation for specific clinical workflows.
2. Identify where to update the PVP process to more consistently and reliably address care gaps.
Suggested team member(s) responsible: Implementation team or QI team; may include the data manager to assist with identifying patients through EHRs.
Examine where you can further incorporate or streamline your practice’s clinical protocols and standing orders into PVP, including via the PVP checklist, daily huddles, and other key clinical workflows.
This may include the following discussion points:
- Who will initiate the discussion with the patient based on the needs (e.g., primary language) and preferences of the patient.
- How and when they will plan to have the discussion during the visit.
- How they will be prepared to address any barriers.
- Educational materials available for use that are relevant to the patient.
Examples and considerations for updating the PVP process are included below.
Clinical guidelines and care gaps: Consider which preventive and maintenance services could be addressed more reliably using PVP, including those in your EHR’s care gap module. The Pre-Visit Planning: Leveraging the Team to Identify and Address Gaps in Care resource provides a more complete list of preventive services for adults and children. Figure 10 provides an example of how your EHR might be able to support flagging patients overdue for specific preventive services
FIGURE 10: PRE-VISIT PLANNING REPORT DETAILING OVERDUE SERVICES FOR AN ADOLESCENT
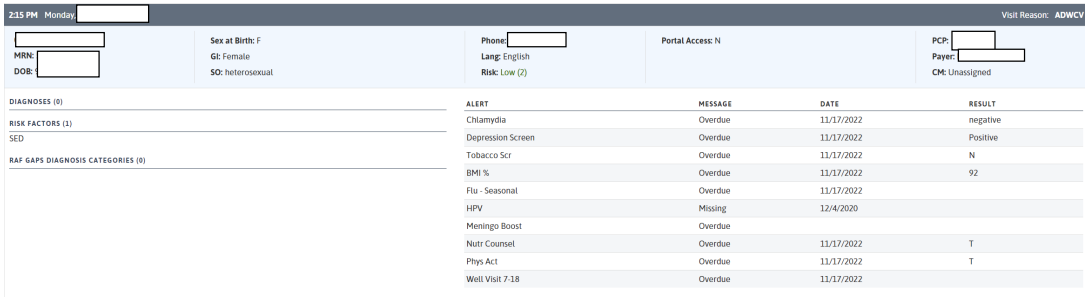
PVP checklist: A generic PVP checklist to be completed by the medical assistant (MA) or LVN at least one to three days before the appointment is provided in Figure 11. Most EHRs will have a health maintenance module that identifies what preventive care is due, but a printed or digital checklist provides a starting point for ensuring key steps aren’t missed.
FIGURE 11. PVP PLANNING CHECKLIST ITEMS TO ADD FOR PEDIATRICS
Checklist Domain |
Checklist Item |
|---|---|
General |
|
Room readiness |
|
Medical record review |
|
Assessments Needed |
|
Care Gaps |
|
Chart scrub: An example chart scrub process led by the MA or LVN as part of PVP for completing open orders is detailed in Figure 12.
FIGURE 12: EXAMPLE CHART SCRUB PROCESS FOR OPEN ORDERS
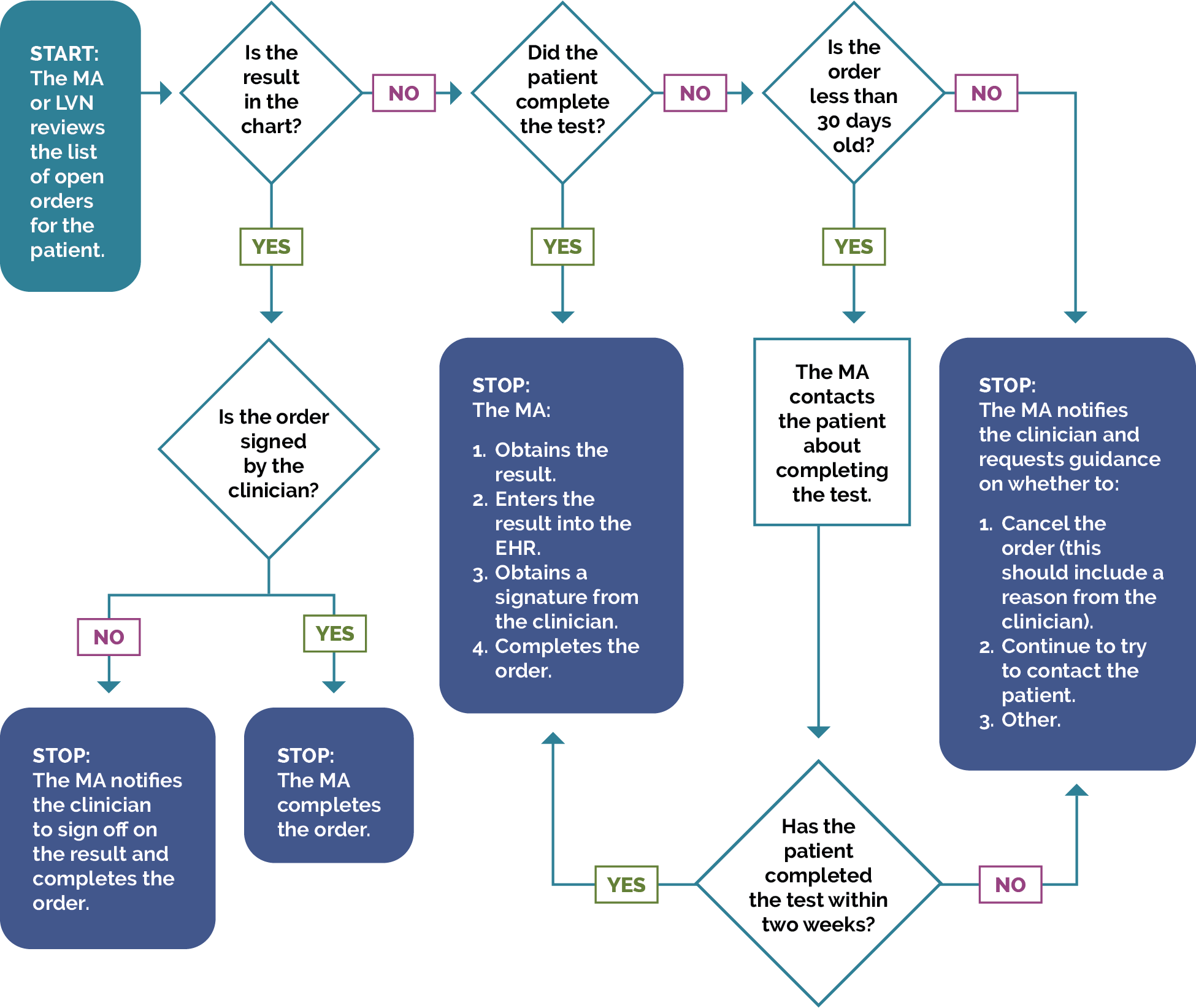
Daily huddles: Design or redesign the team’s daily huddle so the care team can review prioritized action items for the list of patients scheduled to come and any further follow-up for patients seen in the previous days. For more information, see Care Team Daily Huddle Process.
The Centers for Excellence in Primary Care resource on Healthy Huddles includes tools, a video, and examples around how pre-visit planning flows into the daily huddle process, including a “Healthy Huddles Warm-Up,” which can help MAs prepare for huddles.
Patients requiring special considerations: Ensure that the PVP includes a process to flag for the care team:
- Patients requiring special attention, such as those with chronic conditions, complex needs, and recent ED visits or hospitalizations, or who are in foster care.
- Patients who need extended time or additional services during their visit (e.g., multiple vaccinations needed, translation services, mobility assistance, and screenings).
Detailed clinical workflows: Clinical workflows should be updated to describe at which step in the PVP or the patient visit a care team member will address a specific gap in care with the patient.
FIGURE 13: EXAMPLE WORKFLOW FOR SCREENING FOR ADVERSE CHILDHOOD EXPERIENCES
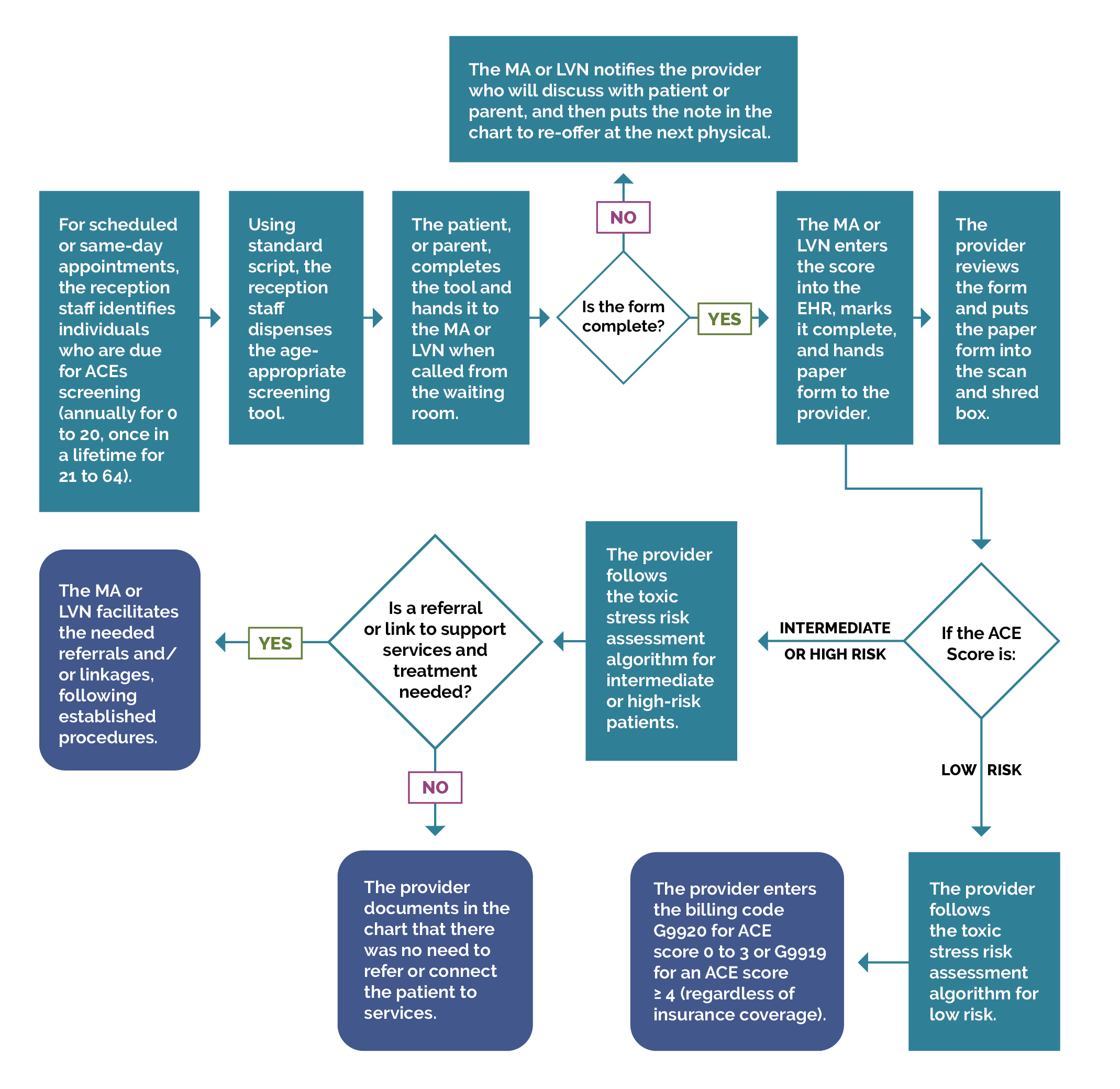
This example workflow for ACEs screening depends on reception staff and MAs and LVNs as core team members for ensuring the patient gets screened when they are in-office and facilitating referrals afterwards.
Planning for care after the visit: Effective PVP includes scheduling pre-visit labs and other diagnostics at the end of the current visit and care coordination for referrals for services not available at the practice. See Key Activity 11: Coordinate Care for more information. Confirm that the patient understands the purpose of any follow-up care. Ensure that the appropriate after-visit summary has been provided at the conclusion of the visit.
Example: Marin Community Clinics has their hospital-based Comprehensive Perinatal Services Program (CPSP) workers schedule both the newborn visit and three-week appointment with the PCP before the birthing person and baby are discharged from the hospital. Medical assistants have been trained to recognize this workflow to avoid confusion that could lead to mistakenly canceling the three-week appointment. If the newborn visit is kept, subsequent appointments are scheduled before the patient checks out. If the appointment is missed, medical assistants follow a missed appointment workflow. The encounter is labeled as “Well-Check No-Show” and categorized as high-risk.
Tip: The American Medical Association (AMA) has an online guide for implementing pre-visit planning, which includes forms, templates and other resources. Limited published literature on the effectiveness of pre-visit planning in the pediatric setting exists, however Samaan, et al. published this study in Pediatrics in 2016: Implementation of a preventive services bundle in academic pediatric primary care centers.
3. Test planned changes to the PVP workflows and support care teams in implementing the workflow.
Suggested team member(s) responsible: Implementation team or QI team.
Test and refine important changes to the PVP process with one or two care teams before considering rolling out the change more broadly at the practice.
Implementing the change includes updating documentation and creating a staff training schedule or “training refresher” for staff to sustain workflow changes. For example, train MA's every 6 months on the PVP. If they have difficulty, have them retake training with a different highly effective MA and monitor closely until competency in the task is reached.
Tip: Develop staff training and talking points on how to communicate about the importance of vaccinations. See more in Key Activity 9A: Providing Caregiver Support to Overcome Vaccine Hesitancy.
4. Establish a process to review and update PVP workflow.
Suggested team member(s) responsible: Care team with quality improvement manager.
Identify staff responsible for reviewing and updating the PVP process at least annually to incorporate the latest clinical guidelines and check for any workarounds that have developed.
KEY ACTIVITY #6:
Develop and Implement Standing Orders
This key activity involves all seven elements of person-centered population-based care: operationalize clinical guidelines; pre-visit planning and care gap reduction.
Overview
A standing order is a pre-approved clinician order to perform a specific intervention for any patient who meets the criteria for the order and is used when the step in the workflow specifically requires the order of a qualified clinician. Standing orders describe the action to be taken and identify who on the care team is authorized to complete the order. Standing orders are designed to enable care team members other than the primary care provider (PCP) to initiate specific clinical actions to provide timely screening and care, provided that specific criteria are met. Common standing orders include preventive measures, such as immunization, to be prepared for, or potentially conducted ahead of the clinician’s time with the patient.
To limit the potential for errors and ensure patient safety, standing orders should be carefully designed, regularly reviewed and revised as necessary. They should be based on evidence-based recommendations and best practices, and they should have broad support from the medical director, practice manager, physicians and other staff. Assessment of current attitudes and strategies to respond to them should inform the testing and adoption process. For more discussion of these matters, see the AAP publication Use of Standing Orders for Vaccination Among Pediatrics. In addition, standing orders should outline the criteria for initiating, modifying or discontinuing a particular course of action or treatment for a patient.[15]
Standing orders, in concert with other key activities, allow care team members to work to the full scope of their license and provide scaffolding to support care team members as they work to greater autonomy. They promote practice workflow efficiency and effectiveness by standardizing who gets what care while freeing up time for the prescribing clinician.
Standing orders help promote equity by ensuring that every patient who meets the criteria for an intervention under the standing order is provided with appropriate services, limiting variation that could occur in interpersonal encounters.
Most EHRs have the ability to enable creation of order sets that can be utilized to create standing orders. Depending upon the health center’s workflows, these can be placed on the chart by providers or can be drawn down by responsible designated staff according to protocols.
Relevant HIT capabilities to support this activity include electronic access to care guidelines, registries, care gap reports and clinical decision support.
Effectiveness of standing orders can be tracked through registries and care quality reports.
Action steps and roles
Outlined below are the actions and steps required to create standing orders and are adapted from the University of California, San Francisco (UCSF) Center for Excellence in Primary Care.[16]
1. Review and understand the latest clinical guidelines for the required standing order and your practice’s already established protocols.
Suggested team member(s) responsible: Quality improvement lead and panel manager, data analyst, or medical director (or equivalent).
Standing orders for recommended immunizations are based on the CDC Child and Adolescent Immunization Schedule by Age.
For some vaccines, clinics need to pay careful attention to how the standing orders are generated. For example, vaccines for diseases such as rotavirus follow a specific timeline; if kids don't receive their first vaccine by a certain age, they are no longer eligible for the vaccine. For other diseases, such as hepatitis A, the vaccine doses must be given six months apart. Additionally, patients who are following a modified or catch-up schedule will receive immunizations on a different timeline than those who are receiving them on the standard recommended timeline.
Consider creating standing orders for additional well-care visit activities (e.g., the periodicity schedule). Some screenings, such as postpartum depression screening, do not require a physician order and are often integrated into clinic workflows and pre-visit planning without utilizing standing orders. However, the distinction between a standing order and a protocol can have different meanings and implications for different teams, so there are instances where practices find it useful to create standing orders for these screenings as a way to support the care team to provide evidence-based care.
2. Translate the appropriate clinical guidelines into a standing order.
Suggested team member(s) responsible: Panel manager or data analyst.
The standing order will follow the relevant clinical guidelines and be updated whenever clinical guidelines are updated. It will generally allow the following:
- Registered nurses (RNs) and/or medical assistants (MAs) with proper training may initiate the agreed upon standing order process when patients meet the agreed upon criteria for initiating screening, and do not have any clinical history that may require a PCP to address the concern.
- Tip: Verify if carrying out standing orders falls within the legal scope of practice for the supportive clinical staff intended to carry them out.
- This may include initiating an order, initiating a referral or notifying the PCP of the need for screening and testing.
Immunize.org has an array of resources for developing and implementing standing orders for use in pediatrics. Many materials on the site can be adapted for other types of standing orders.
In addition to the written standing order, the practice should develop a process map or update other documentation outlining how and when the standing order is to be implemented in the practice’s current workflows.
3. Obtain approval for standing orders from clinical leadership.
Suggested team member(s) responsible: Panel manager or data analyst and medical director (or equivalent).
For the standing order to be valid and in effect, it must be approved by clinical leadership at the practice, signed by a designated valid signatory (e.g., medical director or other physician) and dated, and it must include the effective date for the standing order. Practices should consider including an expiration date and flagging this date in their system to help ensure that the standing order is reviewed and updated regularly. As the clinical guidelines change or other components are updated, the standing order should be signed and dated again by the appropriate party with an effective date for the revision.
4. Train practice staff on how to use standing orders and include this training in clinical onboarding of new staff.
Suggested team member(s) responsible: Medical director or equivalent.
It is critical that practice staff, both those directly named in the standing order and other members of the care team, receive training on the use of this standing order. Such training should include a thorough review of the written standing order and ensure that practice staff understand all of its aspects, including the associated workflow and any additional materials related to the workflow, such as patient education or instructional materials, that include nuances that the care team will need to understand.
Training should be provided on each standing order at least annually, retraining should be provided before the effective date on any revisions, and the training should be part of the orientation for all new members of the practice care team.
Based on feedback from the staff, the standing order can be refined to make the instructions clearer (e.g., during training several staff members were confused by a specific instruction, indicating that the instruction needed to be revised).
5. Institute mechanisms to ensure the proper use of the standing order and its effectiveness.
Suggested team member(s) responsible: Clinical director or equivalent or their designee.
It is likely that one or more aspects of the standing order will not work as planned. For example, the practice’s workflow may not fully support the standing order, the wording may be confusing to one or more staff members, or the standing order’s protocol may not be regularly followed exactly (e.g., staff are using workarounds). The practice should routinely check for these and other common challenges and revise and update the standing order as needed to ensure that it works for the practice and meets all applicable regulations and guidelines.
Complete an annual review of the immunization schedule, WCV activity, and key screenings recommendations to ensure standing orders align with the most up-to-date recommendations from the American Academy of Pediatrics and the Centers for Disease Control and Prevention.
Implementation tips
Avoid common pitfalls of standing orders:
- Standing orders are not updated when screening guidelines are revised and reflect an outdated practice. The remedy is to assign the task of updating the protocols to a member of the team who is responsible for at least annual review and modification.
- New staff are not instructed on the clinical protocols. The remedy is to include review of standing orders as a core element of orientation for all roles named in the standing order.
- Standing orders include the signature of a clinician who is no longer with the practice. The remedy is to review standing orders at least annually and any time a clinician responsible for setting the order has changed roles.
Resources
KEY ACTIVITY #7:
Attend to Social and Emotional Development in WCVs
This key activity involves all seven elements of person-centered population-based care: operationalize clinical guidelines; behavioral health integration; address social needs.
Overview
This activity outlines how practices can support social and emotional development of their patient population, as well as screen for and respond to children with social and emotional development needs.
Social and emotional development creates the foundation for building self-esteem and self-confidence, self-efficacy, self-regulation, and executive functioning, as well as social and communication skills.[17]
Educating and supporting parents and families on how to nurture social and emotional development is an important activity for a pediatric clinic, as is screening for and responding to children and youth with social and emotional development needs. Per the American Academy of Pediatrics (AAP), an understanding of how a child grows and develops can establish realistic expectations for child behavior at all ages. Parents who experienced harsh discipline or other negative childhood experiences may need extra help to change the parenting patterns they learned as children. All caregivers can benefit from increasing their knowledge and understanding of child development including: physical, cognitive, language, and social-emotional development; signs of developmental delays and where to turn for help; and healthy discipline and strategies to impact child behavior.[18]
Universal early childhood developmental screening offers a strong opportunity to discuss childhood development with parents. This discussion can help to promote healthy childhood development and prevent risks that may impact the social and emotional growth of children. Importantly, screening tools for social and emotional development are better than broader developmental screening tools at identifying young children at risk for behavioral and social and emotional issues. The Department of Health Care Services (DHCS) Comprehensive Quality Strategy and Medi-Cal Accountability Set (MCAS) For Health Care Delivery Systems include developmental screening in the first three years of life among their measures.
As trusted authority figures, clinicians play a role in helping parents cope with variability and delays in social and emotional development. This means helping patients and families understand what is normal, when there is a need for watchful waiting, and when there is need for additional follow-up.
Even before the pandemic, one in six children ages two to eight had an unidentified mental health concern.[19] Children of color and children with a social and emotional developmental need or concern from families with lower socioeconomic status are less likely to be identified and supported than white children.[20] Including universal education and screening with response can mitigate this unjust inequity.
For multiple reasons, unmet social needs increase risk for suboptimal social and emotional development. Tending to the social needs of patients and families in service to optimal social and emotional development is an essential strategy. Additionally, bringing a strengths-based, trauma-informed frame to these discussions and interventions can support families and the relationships between the clinic and families. See Key Activity 10: Implement Trauma-Informed Care Approach Across the Patient Journey.
Alongside efforts to support social and emotional development, Bright Futures recommends integrating social drivers of health into primary care to assess family connections and access to resources necessary for optimal child development. Bright Futures has developed age-specific pre-visit questionnaires for ready adoption; they are freely, readily accessible online. These efforts should include:
- Tending to families’ support structure, including extended family, friends and community support. These resources can be valuable for fostering resilience.
- Supporting parents’ resilience, as resilient families are more likely to achieve healthy outcomes and maintain healthy relationships.
EHRs can be utilized to prompt and structure history taking and assessments in well-child visits. Appendix D: Guidance on Technological Interventions lists screening tools that are available in digital format assessments or results-only and can be captured in the EHR as well. These screeners can also be delivered directly to patients on tablets in the office or remotely through patient-facing outreach and engagement applications. Expanded care teams can also utilize care management applications to conduct assessments and to manage referrals required for follow-up. It is important to consider how results and the need for follow-up of any assessments carried out in these other applications are also available in the primary record, as well as used for quality reporting.
Other relevant HIT capabilities to support this activity include care guidelines, registries, clinical decision support, and care dashboards and reports.
Action steps and roles
1. Review current practices to identify key opportunities for improvement.
Suggested team member(s) responsible: QI lead and staff.
Catalog and map the clinic and healthcare team’s current practices and processes related to social and emotional development support, screening and referrals.
Also examine staff’s current comfort with knowledge, tools and communication about social and emotional development.
2. Identify materials and resources for educating about and supporting healthy social-emotional development in childhood.
Suggested team member(s) responsible: Staff.
Review existing materials and explore new sources for educating families about social and emotional development. Select and test materials and resources with a small number of families.
3. Identify social and emotional development screening tools and processes.
Suggested team member(s) responsible: QI lead with staff and families.
Review currently used tools and consider exploring new or other tools for screening social and emotional development during well-child visits (WCVs). Select and test tools with a small number of families. Bright Futures provides a list of links to tools for use at specific Bright Futures visits, as well as screening and assessment tools for use at the discretion of the health care professional: Bright Futures Developmental, Behavioral, Psychosocial, Screening and Assessment Forms.
Please note that some of the tools provided in the link above are free to use. Others, such as the Ages and Stage Questionnaire: Social-Emotional (ASQ:SE-2), require a nominal fee. Again, as mentioned above, Bright Futures has also developed age-specific pre-visit questionnaires for ready adoption, freely, readily accessible online.
4. Develop standard processes for incorporating social and emotional development education, screening and referrals during WCVs.
Suggested team member(s) responsible: Care team.
Test adaptations to current practices and processes to work towards high-quality social and emotional development education, screening and referrals during every WCV. Depending on the need, referral sources range from behavioral health clinicians, development pediatricians, speech and language therapists, early intervention, and the local school system. Having an accessible list of contact information for these resources is an important first step for developing a closed loop referral process. Consider testing different versions of who does what, where, when and how. Create and adapt a process map to standardize and optimize workflow.
5. Focus on the medical care team.
Suggested team member(s) responsible: Director.
Ensure that the medical care team is comfortable addressing socioemotional development education, screening and referrals. Support the care team with education, training and practice delivering sensitive information and supporting parents. Engage behavioral health colleagues who are trained in pediatric care to aid in this work.
Resources
Parental Resilience: Protective and Promotive Action Sheet
The action sheet provides specific advice for clinicians on how to work with parents around each of the five protective factors: parental resilience, social connections, knowledge of parenting and child development, concrete support in times of need, and social and emotional competence of children. Infographics that can be shared with parents for each of these protective factors are available on the Alliance National Parent Partnership Council website.
KEY ACTIVITY #7A:
Develop a Screening Process for Social Needs and Adverse Childhood Experiences (ACEs) that Informs Patient Treatment Plans
This key activity involves all seven elements of person-centered population-based care: behavioral health integration; address social needs.
Overview
This activity provides guidance on screening for health-related social needs and adverse childhood experiences (ACEs) and for beginning to use the data to inform patient treatment plans, including referral to community-based services.
Social needs are defined as individual material resources and psychosocial circumstances required for long-term physical and mental health and well-being, such as housing, food, clean water and air, sanitation and social support. ACEs are the potentially traumatic events that occur before the age of 18 years and are associated with toxic stress that can contribute to adverse health and social outcomes.[21] More specifically, the term ACEs refers to ten categories of adversities across three domains identified in the landmark 1998 study by the Centers for Disease Control and Prevention (CDC) and Kaiser Permanente.[22][23]
There is not yet consensus or uniform endorsement regarding screening for social needs, due at least in part to a lack of high-quality evidence on the risks, benefits and best practices of screening and response.[24] The AAP/Bright Futures currently includes select social needs in its recommendations. Findings from the recent Centers for Medicare and Medicaid Services (CMS) Accountable Health Communities (AHC) Model indicate that the social needs screening and navigation services reduced ED utilization and may have reduced expenditures but did not appear to increase patient’s connection to community services or resolve the patient’s social needs.[25] Other possible ways social needs screening can support attending to social needs include strengthening the patient-provider relationship,[26] destigmatizing social services, tailoring care, and – at a population level – increasing social investment.[27]
Screening for ACEs is neither a recommendation of Bright Futures nor USPSTF. However, California Medi-Cal providers can be reimbursed for ACEs screening when they first complete a mandatory two-hour training. Additionally, DHCS encourages providers to conduct ACEs screening.
Increasing amounts of evidence demonstrates how social needs and ACEs impact physical and mental health outcomes[28][29] and, in turn, how physical and mental health conditions impact social stability.[30] Screening for and responding to unmet social needs and ACEs provides an opportunity to ensure medical care is provided in the context of patient and family life circumstances and as part of a more holistic, person-centered approach to care.
Health equity is advanced by addressing the underlying issues that prevent people from being healthy. At the population level this means addressing communitywide social drivers of health and structural determinants, and at the individual level this means acknowledging and beginning to address health-related social needs.[31]
Social needs screening asks questions about personal and potentially stigmatized aspects of patients’ lives (e.g., poverty, interpartner domestic violence).[32] See below about screening for and responding to unmet social needs and reported ACEs in a trauma-informed way. Also, be aware that staff may also experience trauma when screening for social needs and ensure essential, empathic support for their needs.
Technology-enabled screening can be utilized to screen patients for social needs through various channels: Directly in the EHR, in applications used by care coordinators, and directly to patients via patient-facing outreach and engagement technologies. Practices will need to determine a process to assure that externally generated screening information be incorporated into the patient record and used for care delivery, risk assessment and management and for managing relevant referrals. Social health information exchanges exist in some communities to identify where patients are getting social services and to help identify higher risk patients; these will develop over time.
Ability to link information in parents’ records to the child’s record is often not possible electronically in the EHR, requiring manual data collection.
Action steps and roles
1. Select one or more validated, standardized screening instruments to use and establish how screening results are documented.
Suggested team member(s) responsible: Clinical leadership.
Pick standardized screening tools that fit your organizational environment and the context of your patient population.
- For health-related social needs, the Social Interventions Research and Evaluation Network (SIREN) conducted a review of social needs screening tools and provides a comparison and search tool for different tools for children including Income, Housing, Education, Legal Status, Literacy, Personal Safety (IHELLP) Questionnaire, Safe Environment for Every Kid (SEEK), Survey of Well-being of Young Children (SWYC) and WeCare, as well as tools that are nonspecific to an age including Protocol for Responding to and Assessing Patients’ Assets, Risks and Experiences (PRAPARE), the screening toolkit by Health Leads and several others. The Center for Child Health Policy and Advocacy at Texas Children’s Hospital also has a helpful guide comparing and selecting a screening tool for a pediatric setting.
- For ACEs, consider using a Medi-Cal qualified screener like Pediatric ACEs and Related Life-events Screener (PEARLS) provided for the caregiver for ages zero to 19 years and/or the patient for ages 12 to 19.
Work with your clinical informatics team to determine how staff will document screening results in your EHR. Consider documenting the results of screening for ACEs in a structured EHR field to facilitate reporting and trending at the practice level. Additionally, since screening for ACEs is reimbursable by both Medi-Cal and California commercial health plans since the passage of S.B. 428, ACEs Equity Act (CA 2021), providers should submit the appropriate billing code for reimbursement and to fulfill Medi-Cal managed care reporting requirements to DHCS. Specifically, HCPCS Code G9919 is used when screening yields an ACE score of four or higher; G9920 is used when the ACE score is between zero and three. Some EHR systems have screening tools already embedded and many are moving quickly to incorporate screening; some EHRs may be able to auto-populate Z codes based on screening results. Your managed care plans may offer additional guidance or support and can be a resource to connect your practice to other organizations who have experience with screening instruments and technology tools. By using the same screening tools and/or information technology platforms, the consistency and quality of care delivery can be enhanced.
For the patient’s problem list for health-related social needs, DHCS provides a list of 25 Priority Social Determinants of Health (SDOH) Codes to focus on. This shorter list of codes is intended to capture areas where the health system may have the greatest impact on identifying and addressing social needs.
2. Understand resources and community referrals for positive social needs screens.
Suggested team member(s) responsible: Referral manager, community health workers.
Through CalAIM, the California Department of Health Care Services (DHCS) has taken steps to ensure that Medi-Cal members have access to social support that can impact health outcomes. Connect with your managed care plan (s) (MCPs) and regional area consortia to understand what services and resources they have in place to support patient access to community-based social services. Many MCPs are developing relationships with social services agencies to meet the needs of their members. For Medi-Cal members with the highest level of social needs, MCPs offer Enhanced Care Management (see Key Activity 19: Provide Care Management) and some or all of 14 Community Supports: these provide resources to address social needs such as housing navigation, recuperative post-hospitalization care, and medically tailored meals. Some MCPs use the new CalAssist tool for Medi-Cal members to self-identify whether they are eligible for any of the 14 CalAIM Community Supports and generate a referral to the applicable provider.
Many patients will screen positive for social needs and will benefit from connection to resources that are not part of Community Supports. Contact your MCP to see if they have established relationships with providers who connect individuals to social services. Health plans may contract with an online provider or with a social services network lead entity that can connect you with existing community-based organizations and public agencies in the area. These contracted services will often include a process for making closed loop referrals, where the referring provider is notified if the patient has successfully accessed the referral. Closed loop referrals are a best practice in care coordination that leads to higher levels of patient and provider satisfaction.[33]
Key services to catalog include nutrition assistance, employment readiness, childcare support, postpartum paid family leave, rent and utility assistance, and resources for transportation. Other places to look to build sources for local community referrals include:
- Your current social work staff and/or community health workers, who may have many go-to resources already identified.
- Free online aggregators for local community services in California such as findhelp.org.
- 2-1-1, a free telephone number providing access to local community services for housing, utility, food and employment assistance.
- Resource networks maintained by a local hospital or larger health system in your area.
For going deeper in this area, practices can consider prioritizing quality improvement activities that establish new or previously underutilized community resources to address specific social needs as part of your systematic approach to decrease inequities. See Key Activity 4: Use a Systematic Approach to Decrease Inequities for more information. Case studies provided in the resources linked below provide examples these improvement initiatives.
3. Establish a workflow for screening and referrals.
Consider screening before the patient meets with the PCP and have a workflow in place for follow-up of positive screen (e.g., meet with the care coordinator or care management staff who will facilitate referral). Take steps to flag the positive screen so the PCP is aware and can address any positive screen during the visits.
Train staff in the new workflows and how to provide trauma-informed screening. Several resources are provided below. Staff often initially resist screening if there is a sense they feel they don’t have the tools to help address positive screens.
Following screening, ask patients for their prioritized need and whether they would like assistance before making a referral. Providing a written script for staff and accompanying signage can build confidence in dealing with the challenging circumstances many patients experience.
4. Provide person-centered care that acknowledges social needs.
Suggested team member(s) responsible: PCPs, expanded care team.
Information about a patient’s social needs and ACEs can be used to provide tailored, person-centered care and treatment plans that patients are more likely to follow and benefit from. For example, if a patient and their family screen positive for food insecurity, that could influence details around advice given for healthy weight management.
ACEs Aware offers two asynchronous online courses as well as periodic live recorded webinars for safety net organizations to screen for ACEs and treat toxic stress.
In developing shared plans of care, use trauma-informed ways of engaging patients in their own care, including developing shared goals, providing self-management support, and using communication techniques such as motivational interviewing. See Key Activity 10: Implement Trauma-Informed Care Approach Across the Patient Journey.
The desires and goals of the patient will inform how and when to move ahead in addressing social needs. It is important to support patients through motivational interviewing and trauma-informed practices to create a person-centered care plan. Having processes in place to support ongoing person-centered care planning, such as a warm handoff to a care coordinator or a documented plan to follow up on issues discussed at the next visit, will help to build trust and support connection to community referrals when the patient is ready.
Implementation tips
- Start by identifying the most common social needs (e.g., food, housing, income security) and map out an end-to-end process from identification to resolution for each need.
- Practice coaches can be resources in this process of mapping, which can include:
- Selection of screening tool.
- Capture of data within the tool (e.g. Z codes for health-related social needs for future tracking and reporting.
- Development of a referral pathway, including individuals and agencies responsible.
- Defining success and resolution.
- Ongoing periodic follow-up.
- Seek input from patients, families, clinic staff and referral entities as you develop your process
Resources
KEY ACTIVITY #8:
Provide Dyadic Care: Screen for Postpartum Depression
This key activity involves all seven elements of person-centered population-based care: operationalize clinical guidelines; pre-visit planning and care gap reduction; behavioral health integration.
Overview
California created a dyadic services Medi-Cal benefit effective January 2023. The dyadic services benefit allows Medi-Cal to cover behavioral health and wellness visits that focus on the individual child and their surrounding environment, including caregiver wellness, all within the context of the child’s medical appointment. Dyadic services provide reimbursement for evidence-based health promotion and primary prevention supports that can be brief in duration. Covered behavioral health services include screening for behavioral health problems, interpersonal safety, tobacco and substance misuse, and health-related social needs and referrals for appropriate follow-up care.
This foundational activity provides guidance on screening for postpartum depression (PPD) in a pediatric setting. At minimum, the Clinical Practice Guidelines for Key Medi-Cal Populations of Focus for postpartum depression screening should be adhered to. Currently, the American Academy of Pediatrics (AAP) recommends that pediatric care providers screen mothers for postpartum depression at the infant's one-, two-, four-, and six-month well-child visits (WCVs). Repeated screening at these visits allows for a birthing person who may not be comfortable disclosing initially to do so at a later visit, and it maximizes the opportunity to engage a dyad that may miss one or more of the recommended well-infant visits. AAP also recommends use of community resources for the treatment and referral of the birthing person with depression and providing support for the maternal/child dyad relationship, including breastfeeding support. Of note, some advocates are encouraging screening the partner for postpartum depression as well.
Pediatric care providers have a crucial role in recognizing birthing people who may be experiencing PPD and referring them to appropriate treatment. When left unaddressed, depression can undermine a parent's capacity to form a strong bond with and provide proper care for their infant. This can result in the cessation of breastfeeding, disruptions within the family dynamic, and an elevated likelihood of child abuse and neglect. Moreover, untreated depression can adversely impact an infant's brain development, heightening the risk of toxic stress, which in turn hampers the timely development of language, cognitive skills, and socio-emotional abilities.
Nonetheless, a survey conducted in 2019 among members of the American Academy of Pediatrics (AAP) revealed that merely around half of pediatricians (53.9%) incorporate formal screening for maternal depression into their practices.
According to the AHA’s Institute for Diversity and Health Equity, PPD affects one in eight people and the risk is 1.6 times higher for Black people than white people. Yet Black people are less likely to receive help due to factors such as financial barriers, stigma associated with mental health struggles, structural racism, and a historical mistrust of the healthcare system. Reliable, culturally appropriate PPD screening and follow-up care is essential.
PPD causes intense long-lasting feelings of anxiety, sadness and fatigue, making it difficult for birthing people to care for themselves and/or their babies, as well as handle daily responsibilities.[34] Providing PPD screening and follow-up care, as well as other dyadic services, can identify potential barriers and challenges the perinatal population may face, with long-range impacts on birthing person and newborn outcomes.
Linkage of the birthing person’s prenatal and postpartum records to the infant’s record is often challenging in the EHR, and even more complicated for other children in the family. Care coordination applications are one opportunity to assure that the child’s care plan includes and addresses the birthing person’s concerns. Another approach is assuring that there is a place in the child’s record to store and update this information by more manual means.
Action steps and roles
1. Understand current recommendations for perinatal depression screening compared to the baseline screening rate.
The Clinical Practice Guidelines for Key Medi-Cal Populations of Focus for postpartum depression screening includes the current recommendation. If practices wish to go beyond the PHMI CGAG endorsed recommendations, this 2019 article in the American Academy of Pediatrics also includes current recommendations.
Establish a baseline by assessing the current PPD screening rate compared to the guideline (e.g., PPD screening was documented at 63% of the visits at one to six months). If these data are not available in a format amenable to a care gap report, consider gathering data prospectively by tracking how often PPD screening occurs during recommended visits over the next two to four weeks).
2. Flag all eligible patients for postpartum depression screening and administer screening.
To screen for depression, consider:
- During pregnancy: Patient Health Questionnaire-2 (PHQ-2) or Patient Health Questionnaire-9 (PHQ-9). (PHQ-2 In Spanish; PHQ-9 in Spanish.)
- During postpartum: Edinburgh Postnatal Depression Screen (EDPS). (EPDS in Spanish). Note this is included in some pediatric screening tools, including SWYC.
Care teams may administer depression screening in various ways: verbally by rooming staff, by paper screener at check-in, virtually through tablets at check-in, or as part of a pre-visit screening packet sent via text or email. Regardless of the method, clinic teams must have a process for reviewing the results in a timely fashion on the day of the visit and initiating the next step in the workflow, namely: if the score is positive, the rooming staff would hand off information to the medical or behavioral health staff.
Resources for empathic, trauma-informed screening and responding to positive screens are provided below:
- Postpartum depression and anxiety: How to start the conversation from the AAP.
- Empathic Connections: Follow-Up Conversations on Sensitive Screens.
3. Support access to postpartum mental health services.
If screening results are positive, the pediatric care provider can conduct an assessment or bring in a member of the behavioral health team to do an evaluation and discuss appropriate timing of the best next steps, including combination of the following:
- Watchful waiting.
- Behavioral health referral.
- Medication management.
Ensure staff can activate an immediate suicide risk assessment and response protocol, as needed, for patients with identified suicidal ideation, significant risk of harm to self and/or others, or psychosis. The PHMI People with Behavioral Health Conditions Guide provides more information about implementing a suicide response protocol.
Under the Medi-Cal dyadic care benefit, the caregiver does not need to be enrolled in Medi-Cal or have other coverage, so long as the care is for the direct benefit of the child. This benefit includes services provided to the caregiver during a child’s visit including brief emotional and behavioral assessment, depression screening, and psychiatric diagnostic evaluation. Other relevant dyadic benefits for postpartum depression include dyadic comprehensive community supports services to help the caregiver gain access to needed services and family therapy to improve parent/child relationships and encourage bonding, resolve conflicts, and create a positive home environment.
Case example: In response to a review of their practice’s data showing Hispanic patients were less likely to be screened for maternal PPD, a pediatric practice developed a campaign to better support these patients. Educational materials were created in Spanish to address frequently asked questions and concerns about depression and the need for depression screening, especially during the prenatal and postpartum periods. The screening workflow was altered, so the educational materials were provided alongside the paper screening tool when patients and their families checked in for their appointments. To improve reliability, the practice decided to administer the tool for all visits for children aged one to six months, including both WCVs and sick visits. Care teams were retrained on the process for PPD screening and referrals, including how to respond empathically to achieve positive results.
Resources
KEY ACTIVITY #9:
Proactively Reach Out to Patients Due for Care
This key activity involves all seven elements of person-centered population-based care: proactive patient outreach and engagement, pre-visit planning and care gap reduction.
Overview
Conducting proactive outreach can ensure patients follow through on recommended care. Outreach activities for the pediatric population will almost always be directed towards the parent, legal guardian, or foster parent or caregiver. There may be incidences where a practice outreaches to an older teen, but that would depend on individual or unique circumstances.
As part of pre-visit planning (PVP) and other clinical workflows, your practice should be conducting some level of outreach to provide patients with information they may need to prepare for upcoming visits or engage in follow-up care plans determined during the visit. In addition, most electronic health records (EHRs) can be integrated with an automated reminder system for upcoming appointments and for patients who appear to have gaps in care. Patient outreach also occurs as a part of care coordination, especially around supporting patients to engage in external referrals and in follow-up to a hospital admission or discharge. See Key Activity 11: Coordinate Care for further information.
Proactive outreach to patients due for care focuses on identifying subpopulations among the patients assigned to a care team that may benefit from additional outreach and implementing more personalized reminders and touches for them to engage in care. Of note, multiple outreach modalities exist, including but not limited to phone, text, mail, email, and patient portal, and different modalities may be preferred or more effective with different subpopulations. Consider learning from others (e.g., research, campaigns, AAP recommendations), from your practice’s own experience and from testing various approaches in your QI work.
Outreach to people who are not yet actively engaged in care goes beyond this foundational activity. See going deeper Key Activity 15: Strengthen Community Partnerships for more about identifying trusted messengers in your community.
Proactive outreach ensures that patients remain engaged in care and provides an opportunity for their health needs to be identified and connected to appropriate care in a timely manner. As untreated health needs can lead to worse outcomes, proactive outreach may improve health outcomes. In addition, frequent outreach using multiple approaches can keep the practice front of mind and reinforce the practice’s concern for each patient’s well-being. Outreach and education to caregivers can boost caregivers’ sense of agency, and thereby lead to improved engagement in preventive care and better health outcomes for their children.
Additionally, in California, MCPs are expected to perform at a minimum performance level on multiple pediatric measures related to this activity. Therefore, they may incentivize and/or support practices working on pediatric care.
Focus on equity by using data to identify which populations, subpopulations or groups are experiencing disparities in gaps in care or that the current outreach and education efforts don't reach. When possible, collaboratively designing outreach strategies with community partners and current patients promotes cultural humility and sensitivity.
Health-related social needs (e.g., income insecurity, transportation issues, and health literacy) can result in no-shows and deterioration of patient health status. Proactive outreach, coupled with awareness of clues to health-related social needs, can connect patients to community resources and establish trust in the care team.
Recognize that trauma and its sources can lead to lower engagement. Consider identifying a staff member or peer leader who is very skilled in empathic listening to reach out to caregivers and families to learn what gets in the way of children participating in well-child visits and being immunized, as well as the supports that they would most appreciate and would be most effective. This could be through email or text, phone or in-person conversation, or in focus groups.
This activity relies on similar capabilities as care gap management, utilizing population views and registries to track the pediatric population against the schedule of well-child care. These registries can be utilized to generate outreach lists for appointment schedulers and/or care managers and other care team members who might be tasked with contacting patients due for services. Many EHRs are capable of storing next appointment data that can also be used to generate lists and may link to automated appointment outreach workflows. Patient-facing outreach and engagement technologies can be utilized to deliver appointment reminders and for patient self-scheduling. These applications can include a variety of channels, such as text messaging and chatbots, to provide proactive anticipatory guidance to promote patient engagement and efficient use of visit time. Care managers might use care management applications to track and prompt well-child visits.
Other relevant HIT capabilities to support this activity include electronic access to care guidelines, clinical decision support, including patient-facing clinical decision support and care dashboards and reports. Some health centers may focus extra resources on children and families identified as high risk through risk stratification algorithms. See Appendix D: Guidance on Technological Interventions.
Action steps and roles
1. Identify subpopulations who may benefit from outreach.
Suggested team member(s) responsible: Population health staff, care managers, data analysts, community health workers.
- Start with frequent no-show patients and seek to understand their root causes, which may be related to social health-related needs or health literacy issues.
- Ask your care teams to identify patients they consider high-risk patients who have been lost to care.
- Use care gap reports to identify patients who are behind on screening or who have missed a follow-up visit. See Key Activity 3: Use Care Gap Reports or Registries to Identify All Patients Eligible and Due for Care.
2. Establish the outreach model for your practice.
Suggested team member(s) responsible: Practice leadership.
One outreach model commonly used is to hire dedicated staff as population health specialists. This person would be responsible for using care gap reports to conduct proactive outreach to patients and schedule needed follow-up. See more about this in the care team duties and recommended education resource.
However, different teams may adjust this role to fit their context. An alternative model ensures each care team includes staff with knowledge of the local environment and available resources to conduct telephonic outreach to higher needs patients and their families.
Train all outreach staff in cultural humility, motivational interviewing skills, and in the use of trauma-informed care. See Key Activity 10: Implement Trauma-Informed Care Approach Across the Patient Journey.
3. Supplement your reminder system for contacting various subpopulations.
Suggested team member(s) responsible: Population health specialist with guidance from implementation team and IT staff.
Reminders should be sent to all persons with an upcoming scheduled appointment. The clinic scheduling system will likely have a function for generating automated reminders with an option for patients to cancel or reschedule if they cannot keep the appointment. Reminders should also be sent to all patients who appear to have gaps in care and missed appointment reports. See more about updating your See Key Activity 3: Use Care Gap Reports or Registries to Identify All Patients Eligible and Due for Care to learn more about enabling setting up automated reminders.
Automated reminder systems can support efficiency and reliability. However, more intensive reminders where the patient receives a personalized telephone call from their care team may help patients who are at higher risks of nonattendance or being lost to care.[35]
FIGURE 14: EXAMPLE OF PROACTIVE OUTREACH AND ENGAGEMENT
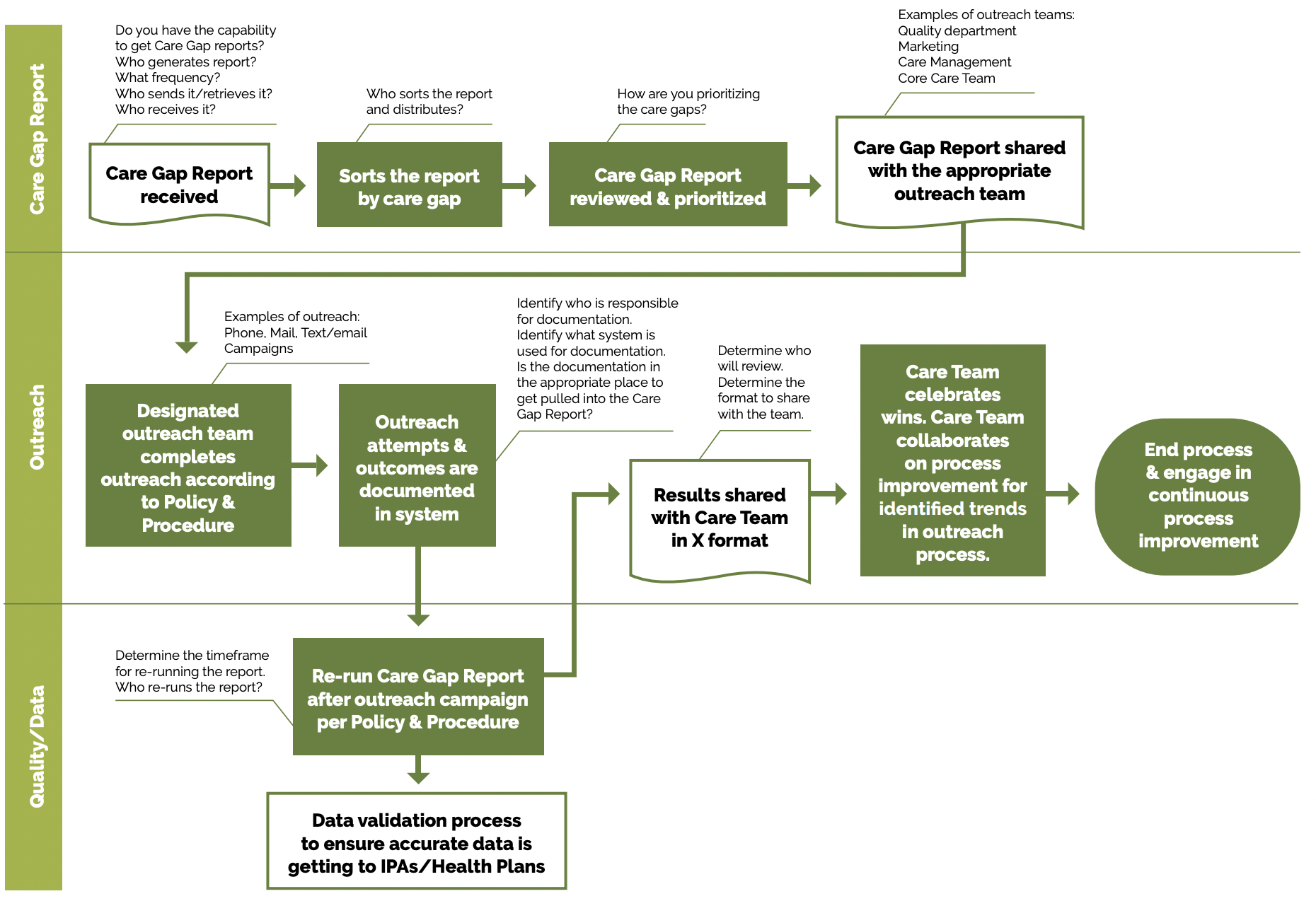
Peer example – outreach call script: San Francisco Health Network’s primary care provider visit call script for pediatric care. This script can be adapted or used to make outreach calls to schedule patient appointments.
Utilize multiple pathways to reach and engage patients. For example, a Swiss clinic used sequential appointment reminders consisting first of a phone call and, secondly, of an text massage, if patients did not answer the phone after three attempts. If the patient had no phone number listed, they received a reminder by mail two days prior to their appointment. The reminder system significantly reduced the rate of missed appointments and allowed the clinic to reallocate 28% of the canceled appointments.
Tip: Consider scheduling these outreached patients on days when you might experience a lower volume of activity in order to level the demand on the care team.
- Whether automated or manual, reminders should accommodate language requirements, as well as stated patient communication preferences (text, email, mail or phone). Reminders that include more than date, time and place and also include an orientation about what to expect and supporting clinical information may be more effective.[36]
4. Use touches that provide alternatives to the traditional office visit.
Suggested team member(s) responsible: IT staff, care coordinators, care team members.
Assess what types of interaction or care can be provided outside this setting and collaborate with patients as part of initial care planning to understand their preferences for communication and care team interactions. Examples include:
- Virtual visits with a provider or nurse.
- Group visits.
- Pharmacy visits.
- Digital communication through emails, texts and patient portals.
- Newsletters focusing on a specific condition.
- Social media that includes discussion groups relative to the management of conditions of focus.
- Home visits for high-risk, historically marginalized or mobility-challenged patients.
- Other technological solutions, such as apps focused on patient conditions which provide a vehicle for ongoing engagement.
5. Establish a process for engaging patients assigned to your practice by their managed care team who have not yet been seen by the practice.
Suggested team member(s) responsible: Multidisciplinary implementation team.
Depending on your agreement with the health plans, it is important for practices to make a proactive plan to build capacity to accommodate assigned-but-not-yet-seen patients in the clinic. Practices should develop strategies for outreach and engagement with these populations in order to shift them from not yet seen to fully engaged in primary care, as well as a process for not-yet-seen patients for whom outreach may be unsuccessful. These patients may be getting their pediatric care elsewhere though still assigned to the practice.
6. Continuously reassess outreach approaches with a goal of improvement.
Suggested team member(s) responsible: Community health workers, outreach workers and navigators, community partners.
- Test your collaboratively designed outreach approaches and measure the effectiveness of your approaches. Review data (e.g., missed appointments, numbers lost to follow up, etc.).
- Survey patients to obtain retrospective and prospective feedback on outreach efforts.
- Regularly update outreach strategies based on community feedback and changing demographics.
Implementation tips
- Providing more intensive outreach: For high-risk patients or patients with complex health and social needs, consider care management as a more intensive approach for facilitating ongoing communication and coordination. See Key Activity 19: Provide Care Management for more information.
- Exploring one-time outreach efforts: Where there is a backlog of patients due to address a gap in care, consider a campaign where you bring in all patients due or overdue for similar screenings, labs or vaccines.
- Back to school: For children and adolescents, certain times of the year create predictable demands on clinics (e.g., back-to-school forms, sports clearance forms). Clinics can use proactive and frequent outreach to help manage these demands by encouraging early action by caregivers and families.
- Going deeper with community partners: For going deeper in this area, consider Key Activity 15: Strengthen Community Partnerships to provide outreach to others outside of your patient population. Community partners can support outreach and health literacy efforts, participate in collaboratively design by providing insight around a particular patient population, and provide resources and supports for patients. Practices can provide education, interventions, outreach and programs in partnership with schools, local youth programming, churches, sports organizations, arts clubs, and other community organizations.
Examples from other organizations:
- West County Health Centers (WCHC) developed and refined workflows for WCVs and immunizations to improve efficiency and streamline outreach.
- The team created outreach lists for patients due for well-child visits using a Tableau dashboard based on claims and encounter information for ages three to six and patient-specific alerts in the EHR for children ages zero to three and over six years to create outreach lists for patients due. The front office staff conducts outreach (letters and calls) to these patients to schedule their well-child visits when due. Once an appointment is scheduled, the MA will conduct pre-visit planning chart preparation to determine and document what is due.
- A separate workflow for childhood immunizations outreach was led by the immunization coordinator. If a parent requests an exemption letter, an immunization committee comprised of medical directors follow guidelines to approve or decline the request and a standard form letter is completed. This process reduces pressure on the provider to approve exceptions when requested.
- Partnership Health Plan and Mountain Valleys Health Centers partnered to improve adolescent immunization rates. Some of the changes they tested included conducting adolescent immunization clinics early in the calendar year to allow for multiple doses required for measure compliance, distribution of gift cards, and accessing gap list members for focused outreach and more.
- Mountain Valleys Health Centers aimed to increase the rate of children and youth who complete WCVs. They tested grocery gift card incentives for completing WCVs and had population health advocate reached out by phone to 180 families to schedule visits alongside a social media campaign.
KEY ACTIVITY #9A:
Provide Caregiver Support to Overcome Vaccine Hesitancy
This key activity involves all seven elements of person-centered population-based care: operationalize clinical guidelines; proactive patient outreach and engagement; address social needs.
Overview
Vaccine hesitancy has been described as a behavior influenced by a number of factors. Vaccine-hesitant individuals are a diverse group with varying degrees of indecision about specific vaccines or vaccinations in general. Clinics may take many approaches to support vaccine-hesitant families of their patients to boost participation rates in well-child visits (WCVs) and immunizations.
Immunizations have resulted in a significant decrease in vaccine-preventable diseases and are one of the single greatest public health achievements of the last century. Over the past decade, however, the value of vaccines has been increasingly challenged. Some parents have concerns about the safety and necessity of vaccines, and those concerns have led to a range of behaviors from hesitancy about some immunizations to declination of all vaccines.
While the minority of parents who refuse all vaccines may be fixed in their beliefs (they may be described as vaccine-resistant), most vaccine-hesitant parents are responsive to vaccine information, will consider vaccinating their children, and are not opposed to all vaccines. Families need support in navigating information and processing the cognitive, emotional and psychological aspects of decision-making about immunizations.
Some populations experience vaccine hesitancy because of distrust of medical systems and research due to historical and existing racism, bias and discrimination. Practices should understand this root cause of vaccine hesitancy and learn from families and their local data if and how racism, bias and discrimination are contributing to vaccine hesitancy and inequities in immunization rates.
Unmet social needs can create barriers to immunization. Empathically assessing for and effectively responding to these needs may improve engagement in WCVs and completion of immunizations.
Additionally, some populations with a disproportionate burden of unmet needs may also be more likely to experience or endorse vaccine hesitancy.[37] Taking a holistic strengths-based and partnered approach to the care of the patient and family may lead to improved social needs and greater uptake of immunizations.
It is important that data fields and workflows are configured to accurately capture vaccine declination in order to understand and manage the problem. Patient outreach and engagement technologies can assist the care team in assessing vaccine hesitancy as well as delivering education, such as clinical templates and/or prompts in the EHR and care coordination applications, to guide provider and care team discussions. Care dashboards and quality reports can be utilized with data analytics to identify trends that might suggest population-level strategies.
FIGURE 15: EXAMPLE OF DOCUMENTING REASON FOR VACCINE DECLINATION IN EHR
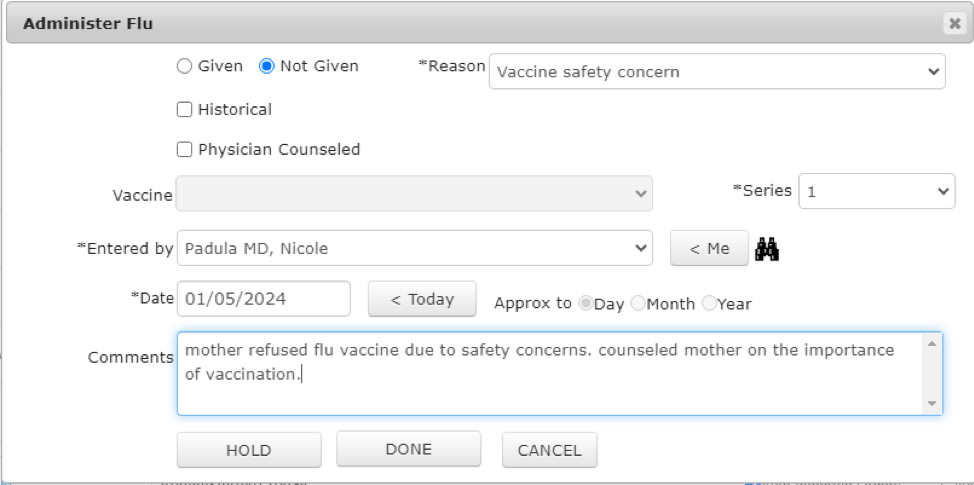
Action steps and roles
Adapted from: Ensuring COVID-19 Vaccine Equity for Children: Considerations for Pediatric Teams and Community Partners - CHCS Blog [Internet]. Center for Health Care Strategies. 2021. Available from: https://www.chcs.org/ensuring-covid-19-vaccine-equity-for-children-considerations-for-pediatric-teams-and-community-partners/
1. Determine current immunization completion rates by age group, by key sociodemographic characteristics, and by vaccine.
Suggested team member(s) responsible: Data manager or QI lead.
Segment the practice’s data on immunization and WCV completion rates to identify groups of children who are not meeting goals.
2. Listen to families, communities and clinic staff.
Suggested team member(s) responsible: QI lead and staff.
Identify barriers to immunization completion, including vaccine hesitancy and strengths-based, family-driven solutions, through trusted and authentic partnerships with families and communities. See Figure 16 for a compendium of reasons for vaccine hesitancy.
Also, examine the staff’s current comfort both with immunizations and with addressing parental concerns. Providing a psychologically safe environment for staff to express their own hesitancies and engage in respectful education and dialogue about immunizations can yield greater understanding, buy-in, and support from practice staff.
FIGURE 16: PARENTAL CONCERNS ABOUT VACCINES
Vaccine safety:
- Too many vaccines.
- Development of autism.
- Vaccine additives (e.g., thimerosal, aluminum).
- Overload the immune system.
- Serious adverse reactions.
- Potential for long-term adverse events.
- Inadequate research performed before licensure.
- May cause pain to the child.
- May make the child sick.
Necessity of vaccines:
- Disease is more “natural” than a vaccine.
- Parents do not believe diseases being prevented are serious.
- Vaccine-preventable diseases have disappeared.
- Not all vaccines are needed.
- Vaccines do not work.
Freedom of choice:
- Parents have the right to choose whether to immunize their child.
- Parents know what’s best for their child.
- Believe that the risks outweigh the benefits of the vaccine.
- Do not trust organized medicine or public health.
- Do not trust government health authorities.
- Do not trust pharmaceutical companies.
- Ethical, moral or religious reasons.
Reproduced from Edwards KM, Hackell JM. Countering Vaccine Hesitancy. PEDIATRICS [Internet]. 2016 Aug 29;138(3):e20162146–6.
3. Review current practices to identify key opportunities for improvement.
Suggested team member(s) responsible: QI lead with care team and families.
Catalog and develop process maps for the clinic and care team’s current practices related to presenting and educating caregivers and families on immunizations, addressing concerns and vaccine hesitancy, using support materials related to vaccine hesitancy, and tracking effectiveness of current practices. Consider how the use of standing orders integrates with this process.
4. Share information effectively to build vaccine confidence.
Suggested team member(s) responsible: Care team.
Develop clear, concise and accessible messaging to discuss vaccine safety and efficacy with families and to counteract persistent misinformation campaigns. When possible, review sources of information and misinformation with families who express hesitancy.
One way to quickly incorporate effective communication is to adapt language that has already been crafted to address families' concerns about immunizations. Use culturally sensitive language and tailor existing resources to reach specific communities, including Black and Hispanic or Latino/a communities, as well as refugee, immigrant and migrant communities. See Figure 17 for communication highlights related to vaccine hesitancy, as well as resources for this activity below.
FIGURE 17: COMMUNICATION HIGHLIGHTS
- Vaccines are safe and effective, and serious disease can occur if your child and family are not immunized.
- Vaccine-hesitant individuals are a heterogeneous group, and their individual concerns should be respected and addressed.
- Vaccines are tested thoroughly before licensure, and vaccine safety assessment networks exist to monitor vaccine safety after licensure.
- Nonmedical vaccine exemptions increase rates of unvaccinated children.
- Unvaccinated children put vaccinated children and medically exempt children who live in that same area at risk.
- Pediatricians and other health care providers play a major role in educating parents about the safety and effectiveness of vaccines. Strong provider commitment to vaccination can influence hesitant or resistant parents.
- Personalizing vaccine acceptance is often an effective approach.
- The majority of parents accepted the provider’s vaccine recommendations when they were presented as required immunizations to maintain optimal disease prevention.
- The current vaccine schedule is the only one recommended by the CDC and the AAP. Alternative schedules have not been evaluated.
Reproduced from Edwards KM, Hackell JM. Countering Vaccine Hesitancy. PEDIATRICS [Internet]. 2016 Aug 29;138(3):e20162146–6.
Tip: When talking to parents about vaccines for their child, it is a best practice to be clear and direct about what vaccines are due. For example, instead of asking, “What do you want to do about shots?” state, “Your child is due for three vaccines.” Instead of asking, “Have you thought about the shots your child needs today?” state, “Your child is due for Tdap, Hib, and hepatitis B shots today.”
5. Focus on the care team.
Suggested team member(s) responsible: Director.
Ensure that the care team is comfortable addressing vaccine hesitancy and other family concerns to foster an environment where all families feel supported. Consider offering training, such as the teach-back method.
Help staff vaccinate their own families by offering vaccine drives or additional paid time off. Offering opportunities for the care team to vaccinate their own families provides a space for staff to talk about the experience of vaccinating their families with the community they serve and signals the practice’s commitment to vaccination.
6. Measure progress, consider equity, and continuously improve your approach overall and for key subpopulations.
Suggested team member(s) responsible: Data manager or QI lead.
Whenever possible, track vaccination data in real time and collect disaggregated data by race and ethnicity, as well as by language spoken and geographies. Advocate for practices and policies that drive vaccine equity and benefit all families.
Special consideration for human papillomavirus (HPV): One special circumstance worth noting is the potential divergence between parental and adolescent immunization preferences with respect to HPV vaccination. The adolescent may, unknown to the parent, wish HPV vaccination, but the parent may not provide consent. Practices should adopt a consistent and systematic approach to when and how adolescent HPV immunization will be provided without parental consent, given existing CA law that permits this. Practices may want to be familiar with existing literature on adolescent consent for the human papillomavirus vaccine, including ethical, legal and practical considerations, and the HPV vaccine and parental consent. Most importantly, practices should be aware that California law allows adolescents to consent to HPV vaccination without parental consent.
Resources
AAP Immunization Website
The American Academy of Pediatrics (AAP) provides information on immunizations in general, plus a page with commonly asked questions from parents.
Evidence base for this activity
- Edwards KM, Hackell JM. Countering Vaccine Hesitancy. PEDIATRICS [Internet]. 2016 Aug 29;138(3):e20162146–6. Available from: https://pediatrics.aappublications.org/content/138/3/e20162146
- Gilmour J, Harrison C, Asadi L, Cohen MH, Vohra S. Childhood Immunization: When Physicians and Parents Disagree. Pediatrics [Internet]. 2011 Nov [cited 2019 May 5];128(Supplement 4):S167–74. Available from: https://pediatrics.aappublications.org/content/128/Supplement_4/S167
- Maglione MA, Das L, Raaen L, Smith A, Chari R, Newberry S, et al. Safety of Vaccines Used for Routine Immunization of US Children: A Systematic Review. PEDIATRICS [Internet]. 2014 Jul 1;134(2):325–37. Available from: https://pediatrics.aappublications.org/content/134/2/325
- Byington CL. Vaccines: Can Transparency Increase Confidence and Reduce Hesitancy? Pediatrics [Internet]. 2014 Aug 1;134(2):377–9. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4187240/
- Sahni V, Lai FY, MacDonald SE. Neonatal Vitamin K Refusal and Nonimmunization. Pediatrics. 2014 Sep 1;134(3):497–503. Available from: https://pubmed.ncbi.nlm.nih.gov/25136042/
Summary: Children whose parents refused vitamin K at birth are 14.6 times more likely to be unimmunized by age 15 mo. This provides an opportunity to identify a subset of likely vaccine-hesitant parents at birth and engage them with information in a focused effort. - Hendrix KS, Finnell SME, Zimet GD, Sturm LA, Lane KA, Downs SM. Vaccine Message Framing and Parents’ Intent to Immunize Their Infants for MMR. PEDIATRICS [Internet]. 2014 Aug 18 [cited 2020 Jan 20];134(3):e675–83. Available from: https://pediatrics.aappublications.org/content/134/3/e675
Summary: A survey found that parents who were informed about the MMR vaccine’s direct benefits to their child, rather than the vaccine’s benefits to society as a whole, were more likely to immunize.
KEY ACTIVITY #10:
Implement Trauma-Informed Care Approach Across the Patient Journey
This key activity involves all seven elements of person-centered population-based care: proactive patient outreach and engagement; care coordination; behavioral health integration; address social needs.
Overview
This activity provides guidance on concrete actions that practices can take to embed trauma-informed care into their daily workflows and interactions with patients.
Individual trauma is defined by the Substance Abuse and Mental Health Services Administration (SAMHSA) as follows: “Individual trauma results from an event, series of events, or set of circumstances that is experienced by an individual as physically or emotionally harmful or life-threatening and that has lasting adverse effects on the individual’s functioning and mental, physical, social, emotional or spiritual well-being.”[38] Toxic stress is similar: significant stress that is frequent or prolonged without adequate buffering protections. Many experiences may be traumatic, including but not limited to: physical, sexual and emotional abuse; childhood neglect; living with a family member with mental health or substance use disorders; sudden, unexplained separation from a loved one; poverty; racism, discrimination and oppression; and violence in the community, war or terrorism.”[39]
Trauma-informed care (TIC) is defined by the National Child Traumatic Stress Network as “medical care in which all parties involved assess, recognize and respond to the effects of traumatic stress on children, caregivers and healthcare providers. In the clinical setting, TIC includes the prevention, identification and assessment of trauma, response to trauma, and recovery from trauma as a focus of all services.”[40]
People can build trauma-informed healthcare organizations that create safe, caring, inclusive environments for all patients. A number of trauma-informed strategies exist that organizations can adopt to help people overcome the effects of trauma. These strategies range from organizational changes in the culture and atmosphere of a healthcare setting to the full adoption of practices to address trauma at the clinical level.[41]
Of note, the Pediatric ACEs and Related Life-events Screener (PEARLS) includes the following factors in its assessment:
- Abuse (e.g., physical, emotional, sexual).
- Neglect (e.g., physical, emotional).
- Dysfunction in the household among parents and caregivers (e.g., caregiver separation or divorce, domestic violence, substance misuse, incarceration, mental illness).
- Hardship (e.g., food insecurity, housing instability).
- Other significant life events (e.g., caregiver’s serious physical illness or death, community violence, bullying, discrimination).
Actions that support cultivating trauma-informed care include:
- Ensure patients are warmly welcomed on the phone or in person.
- Train all staff and providers in universal empathic communication and conveying respect, dignity and compassion to patients.
- Ensure that staff maintain healthy interpersonal boundaries and manage conflict appropriately.
- Strive for consistent patient scheduling and inform patients when appointments are running late.
- Offer sufficient apology and repair when scheduling or other changes are necessary.
- Maintain communication with patients and between the healthcare team that is consistent, open, respectful and compassionate.
- Be aware of how an individual’s culture affects how they perceive trauma, safety, resiliency and privacy.
- Enhance staff and provider skills in administering and responding to sensitive screenings, such as adverse childhood experiences, substance use disorders, and others.
- Inform patients that they have the option to complete or abstain from screenings (e.g., ACEs and other behavioral health, developmental and social needs) and connection to relevant, trustworthy resources, as needed.
- Ensure staff competency in skills to prevent and intervene early in escalations to ensure a safe atmosphere.
- Provide a safe environment, ensuring well-lit parking lots and supportive and adequate security measures.
- Provide a warm and calm environment from the waiting room to the exam room, with low noise levels and decor with warm colors and gentle images.
- Provide care that is sensitive to the patient’s racial, ethnic, and cultural background and sexual orientation and gender identity.
As the American Academy of Pediatrics acknowledges, pediatricians and other pediatric care providers (e.g., family physicians, pediatric nurse practitioners) are likely to be the first, and often only, professionals who encounter the 68% of American children who have experienced trauma, and have the greatest potential for early identification and response to childhood trauma. TIC is fundamentally relational health care – the ability to form safe, stable and nurturing relationships (SSNRs). Pediatric care providers can support the caregiver/child relationship, the context in which there can be recovery from trauma and the restoration of resilience.”[42]
Additionally, using a trauma-informed approach benefits not only patients but also providers and staff. For patients, TIC offers the opportunity to engage more fully in their health care, develop a trusting relationship with their provider, and improve long-term health outcomes. It may also help reduce burnout among healthcare providers, potentially reducing staff turnover.[43]
Racism, bias and discrimination are pervasive forms of trauma.[44][45] Providing TIC supports equitable outcomes and limits effects of racism, bias and discrimination in multiple complementary ways. For example, people affected by trauma may develop coping mechanisms to help alleviate the emotional and/or physical pain they feel as a result of trauma. Sometimes, these strategies involve maladaptive behaviors, such as unhealthy eating, tobacco use, or drug and alcohol use. These coping mechanisms may provide some relief, but they can also simultaneously contribute to anxiety, social isolation and chronic diseases.”[46] Of note, there is evidence to support the potential benefits of racial concordance between patient and provider; ensuring concordance, when possible, may be one strategy to support patients who disclose trauma related to racism and/or discrimination.[47][48][49]
Additionally, regardless of the type of trauma a person has experienced, traumatic experiences impact relationships. This includes, but is not limited to, relationships between people, communities, and the delivery systems that support individuals’ health and social needs. When a person experiences trauma, they may feel unsafe, betrayed, and/or have difficulty trusting others. This can lead to heightened emotions, such as anger or aggression, or a tendency toward shame, numbing and/or isolation. Within the context of healthcare, this can negatively impact the bond between a patient and their provider, and thus a patient’s engagement in care.[50]
Providing trauma-informed care is likely to boost care participation by patients and caregivers with social needs, since TIC practices are designed to welcome people into care by supporting them and avoiding retraumatization. Certain social needs may be an ongoing source of trauma. The more access people have to trauma-informed preventive care, the more opportunities practices will have to identify unmet social needs and connect patients and caregivers to needed supports and resources.
Consider how a trauma-informed approach applies to patients of different ages (e.g., young children, youth, young adults) and to parents or caregivers. All groups will benefit from recognition of trauma and the practice of trauma-informed care.
Technology can support trauma-informed care by delivering structured guidelines, protocols and clinical decision support to care team members responsible for carrying out assessments and incorporating standardized screening tools into EHRs and care management/care coordination applications. These screening tools can also be made available directly to patients through patient outreach and screening technologies. Recording information regarding trauma exposures in standardized ways is important in assessing their prevalence. Understanding their prevalence will assist in program and resource development to track impact on health outcomes and to incorporate into risk stratification. Health information technologies used to track referrals are also important in care management.
Action steps and roles
1. Build awareness and generate buy-in for a trauma-informed approach.
There are many ways to become a trauma-informed organization, and the process does not have to be a burden to adopt. Foundational steps that organizations can take to move toward fully adopting a trauma-informed approach to care include:
- Using existing meetings and initiatives to build awareness and generate buy-in for a trauma-informed approach.
- Supporting a culture of staff wellness.
- Hiring a workforce that embodies the values of trauma-informed care.
- Creating a safe physical, social and emotional environment.
The Trauma-Informed Care Implementation Resource Center, Center for Health Care Strategies, and the California Academy of Family Physicians provide a range of guidance and tools for getting started.
2. Provide TIC training to all staff.
Incorporate TIC training into new hire orientation, and require all staff to complete TIC training. Training sessions should include role play, patient and family testimonials, and reflection by staff members. Include examples of trauma-informed approaches in all staff roles, and discuss how specific practices may hinder patients’ and families’ resilience. Include focus on team members’ own well-being. The practice’s QI lead should include pre- and post-training feedback, including questions on staff confidence in implementing TIC practices.
The California ACEs Aware website has online access to free trainings.
A potential list of introductory topics could include:
- Introduction to trauma-informed care:
- What is trauma? Definition, types, and prevalence.
- The physical, emotional and psychological effects of trauma.
- Design principles and core values of trauma-informed care.
- How patients and the care team benefit from trauma-informed care.
- Trauma-informed care at a Community Health Center.
- Recognizing and responding to trauma:
- Trauma-sensitive communication: Effective ways to interact with trauma survivors.
- Signs and symptoms of trauma.
- Link between trauma and physical health conditions.
- Recognizing potential triggers for trauma survivors.
- Creating a trauma-informed environment:
- Establishing a safe and trusting atmosphere.
- Strategies to prevent retriggering trauma.
- Understanding the impact of cultural differences on trauma experiences.
- Ensuring patients have a say in their care.
- Trauma-informed practices at our practice:
- Screening for trauma.
- Trauma-informed intake.
- Trauma-informed care planning with patients.
- Linkage and referrals to experts on trauma-informed care.
3. Provide ongoing support to promote resilience among all staff.
Suggested team member(s) responsible: Human resources.
The practice’s human resources lead should periodically remind all staff of the array of confidential employment assistance available to them, as staff may be experiencing the impacts of childhood ACEs or ongoing sources of trauma, which will affect their health and well-being, as well as likely impact their ability to approach patients in a trauma-informed way. Likewise, personal development, team building, and practices aimed at boosting joy in work, if leveraged in trauma-informed ways, are all likely to support staff and limit the effects of trauma.
4. Provide ongoing supervision to all staff.
Suggested team member(s) responsible: Director.
Ideally, each staff member should have supervision time (perhaps twice monthly) with a TIC-trained direct supervisor to surface bright spots and challenges and work through questions toward professional development. Behavioral health and human resources leaders should assess supervisors’ ability to engage with patients, families and staff in trauma-informed ways, as well as guide others to do the same.
When one-on-one supervision time is lacking, explore ways to develop other supports around TIC implementation. This could include devoting portions of regular staff meetings to surface TIC implementation challenges and bright spots, leveraging and highlighting standout workers’ skills and capacities to support the wider staff’s ability to implement TIC, or incorporating short training modules during staff meetings.
5. Partner with patients and families to identify trauma-informed practices that support your patient populations and improve existing practices, including eliminating practices that reinforce trauma.
Suggested team member(s) responsible: QI lead.
As a foundational step, clinic leaders should invite families to shape TIC training topics and practices, with attention given to making it easy to participate in these sessions. This may mean scheduling after-hours, offering refreshments and childcare, and paying family representatives for their time.
Going deeper, your practice can work with experts, patients and families on eliminating practices that create or reinforce trauma and replacing them with trauma-informed practices. The Center for Care Innovations (CCI) offers guidance on becoming a healing organization. Consider using the capacity assessment tool for trauma and resilience-informed pediatric care. The Trauma-Informed Care Information Resource Center also offers an analysis of a host of tools to assess an organization’s uptake of trauma-informed practices.
6. Improve the clinic’s physical environment.
Suggested team member(s) responsible: Director, human resources staff, caregiver representatives.
The American Academy of Pediatrics recommends creating a safe environment using engagement strategies to build trust, focusing on strengths to empower patients and families, and having brief office-based approaches to promote a growth mindset.
Ensure that the clinic offers well-lit spaces from the parking lot to the examination rooms, that noise levels are low in the waiting room and all patient areas, that security is sufficient, and that decor integrates warm colors and gentle images.[51]
Partnering with caregivers to assess the current state, identify improvement opportunities, and shape improvements will build relevance and ownership of the changes.
7. Track the results of TIC training and implementation.
Suggested team member(s) responsible: QI lead, director.
QI leads should include pre- and post-training feedback, including questions on staff confidence, in their ability to recognize signs of trauma and implement TIC practices. Patient experience surveys should include questions about the patient’s and family’s level of comfort at the practice and their ability to get the care and support that they want and need when they want and need it. Rather than creating your own survey, consider implementing an existing survey.
Consider how you will track results. One option is to track the percentage of respondents who respond favorably, and responses could be segmented to identify groups of patients and families who respond negatively or less positively than others.
8. Develop formal and informal feedback loops with patients and the care team to understand the effectiveness of your approach to TIC.
Suggested team member(s) responsible: QI lead, director.
To help ensure that your approach is meeting the needs of patients and is consistently feasible for the care team, it is important to have both formal and informal feedback loops.
For patients, feedback loops might include:
- Patient satisfaction surveys (or similar).
- Follow-up calls with a subset of patients to understand what has been going well and what could be improved.
- Patient focus groups.
- Feedback from the practice’s patient advisory board (or similar).
Having an accessible, safe and robust patient complaint process is also a critical dimension to practice learning about TIC opportunities in conjunction with formal patient experience surveys. At the minimum, educate Medi-Cal patients about their rights to submit a grievance to the Medi-Cal managed care plan and submit complaints about discrimination to the DHCS Office of Civil Rights. However patients choose to express dissatisfaction, it is important to assure them that they will not experience any retaliation from their providers or health plan.
For the care team, feedback loops might include:
- Daily huddles.
- Existing or new staff satisfaction and feedback mechanisms.
- Supervisors and managers eliciting feedback and experiences from staff during one-on-one meetings.
- Regularly scheduled meetings and calls to get staff feedback on processes, methods and tools.
9. Align trauma-informed care and equity efforts.
Trauma-informed care and a trauma-informed culture must, by definition, also be equity-informed. Racism and discrimination are risk factors for toxic stress and have long-term health consequences. Additionally, through implicit bias and systemic racism, people of color have often been harmed in healthcare and social care systems. TIC efforts that are aligned with organizational equity efforts, such as diversity, equity and inclusion (DEI) work, and efforts to eliminate health disparities will strengthen both. Strategies include:
- Align and cross-support TIC task force aims with the DEI committee’s aims.
- Include anti-bias training for staff and providers within TIC training.
- Frame cultural humility as a central part of TIC.
Integrating trauma-informed care across care delivery
Coordinated care delivery that is trauma-informed may include:
- Screening for ACEs and recording screening results in the EHR. See more in Key Activity 7A: Develop a Screening Process for Social Needs and Adverse Childhood Experiences (ACEs) that Informs Patient Treatment Plans.
- Referring patients needing further support to specialist providers internal or external to the practice and/or to community organizations which can support social needs.
- Performing warm hand-offs of patients to needed providers of specialist or social support.
Importantly, there is no one workflow for implementing a TIC approach in the patient care journey within a practice. Rather, this endeavor requires proactively and intentionally integrating a TIC approach across all activities and interactions in patient care. While the awareness, training and support efforts may look similar across different sites of care, the starting place for implementing a TIC approach – and the subsequent opportunities for implementation – will likely be different across sites. For example, one clinic may choose to start by first implementing a TIC approach in their check-in process, whereas another clinic may choose to start with their newborn WCVs.
KEY ACTIVITY #11:
Coordinate Care
This key activity involves all seven elements of person-centered population-based care: proactive patient outreach and engagement; pre-visit planning and care gap reduction; care coordination; behavioral health integration; address social needs.
Overview
This activity will help you provide care that is person-centered and coordinated across all internal and external providers involved with the patient.
Care coordination involves deliberately organizing patient care activities and sharing information among all participants concerned with a patient’s care to achieve safer processes and more effective outcomes.
Care coordination is an integral part of providing high-quality population-based care in an ambulatory care clinic. In your practice, care coordination happens daily as part of standard work and includes activities such as assisting patients with referrals, managing patient messages and receiving incoming information from outside care partners, including pharmacies, specialists, hospitals and community partners (e.g. schools, employers, community-based organizations).
Managing care across multiple settings is often a source of frustration and dissatisfaction for both patients and providers. Lack of coordinated care can result in both duplication of services and lack of completion of needed services. When care is not coordinated, decisions can be made without a complete picture of the patient’s needs and goals. Practices that have effective care coordination processes often employ closed loop referrals as a best practice.[52][53] In a closed loop referral, a referring provider can track the status of the referral (e.g., completed or pending) as well as the outcome of the referral, including whether additional follow-up is needed. When closed loop referrals are implemented, both provider and patient satisfaction is enhanced.
There are four fundamental concepts when thinking about care coordination activities within your practice:[54]
- Accountability: A key to successful care coordination is accountability. Clinics and systems that excel at care coordination take ownership and assume responsibility for care coordination activities. Examples of care coordination processes include development of infrastructure for care coordination, identification of staff responsibilities, and relationship building with referral partners. Together, these actions create the ability to support referrals and transitions and track them to completion.
- Patient support: Referrals and transitions often raise questions for patients and families and can be a source of anxiety. Not only do the logistics of a referral or transition create questions, but also patients and their families can experience anxiety regarding the outcome or purpose of a referral or transition. When a practice can dedicate staff time to addressing the needs of patients and families, referrals and transitions are most likely to accomplish intended goals.
- Relationships and supports: Referrals and transitions work best when all parties – patients, primary care providers, and consultants – agree on the purpose and importance of the referral and the roles that each will play in providing care.
- Connectivity: Building relationships and agreements among providers, including community agencies, lead to shared expectations for communication and care. Connectivity includes developing referral relationships, accepting accountability, and creating data flow.
In order to conceptualize how practices can coordinate with community-based agencies (housing, food, income support), hospitals and ERs, and specialists, refer to the visual depiction of the care coordination model by the Center for Accelerating Care Transformation (ACT Center).
Care coordination can benefit all patients in your practice and care coordination processes, such as closed loop referrals, can be applicable to many practice activities. Common areas where care coordination can be enhanced include specialty referrals; referrals to social supports, such as transportation; and housing needs. Care coordination activities can also identify patients who need a higher level of support through a care management program (see more in Key Activity 19: Provide Care Management). Care management differs from care coordination in that a patient consents to and works directly with a care manager to create a care plan that is shared with an extended care team. While a practice can decide whether it has the resources to provide higher level care management services, care coordination is a foundational activity of effective population health management.
Care coordination for Medi-Cal patients
Patients with Medi-Cal have access to many resources that can support improved health outcomes and social needs. These Medi-Cal resources can be another opportunity to create care coordination processes in your practice; see Figure 18 for a partial list of Medi-Cal programs that involve care coordination. As of 2023, both doula care and community health worker services are a benefit of the Medi-Cal program. The services of CHWs, also known as promotores can be highly effective in helping to connect patients to resources and educational materials that are community-based and aligned with a patient’s values, language and cultural needs to further health equity. The California Health Care Foundation offers an overview of the CHW program, including potential hurdles.
Medi-Cal patients with high medical, behavioral health and/or social needs may be eligible for Enhanced Care Management and Medi-Cal Community Supports services (see going deeper activity Key Activity 19: Provide Care Management for more information on these programs).
There are also a number of Medi-Cal programs which provide services and support to Medi-Cal patients who qualify. Care coordination between the practice and these programs can result in more integrated care for eligible patients. Some examples include:
- California Children’s Services (CCS): Care coordination and support for eligible children with high levels of medical needs.
- Long-term services and supports (LTSS): These are available to support individuals in the community and include skilled nursing facility services, personal care services, self-directed personal assistance services, in-home supportive services, and home- and community-based services.
FIGURE 18: EXAMPLES OF MEDI-CAL PROGRAMS OR BENEFITS THAT INVOLVE CARE COORDINATION
- Enhanced Care Management
- Community Supports
- Community Health Workers
- Doula
- Long term services and supports (LTSS)
- California Children’s Services (CCS)
Effective care coordination helps your practice to better meet the broad range of patients' needs and preferences. It helps ensure that each patient's needs and preferences are known and communicated at the right time to the right people and that this information is used to guide the delivery of safe, appropriate and effective care.
Key outcomes of care coordination:
- Greater patient participation and satisfaction.
- Closed gaps and addressed inequalities that exist in access to care.
- Improved quality outcomes and the potential to leverage quality financial incentives.
- Decreased staff burnout and duplication of services (e.g., “Let the system do the work”).
Effective care coordination helps to reduce health disparities among different populations by better identifying and then working to address a broad range of patient needs. When care coordination is effective, the patient is at the center of care and the patient's cultural, social and health needs are incorporated into a plan of care. By identifying outside clinical supports (e.g., hospital care, specialist care) and social supports (e.g., housing assistance, transportation, food security, etc.) and creating pathways for coordination, the practice promotes equity by facilitating access to these services for all patients who need them. As part of a care coordination strategy, practices should consider the growing number of aggregator organizations (see resources section below) that partner with community-based programs and resources centered around addressing social needs such as housing, food and community. Many of these community-based programs are tailored for specific demographic groups and can support patients in meeting their needs in a culturally competent way.
Technology can be used to streamline and enhance care coordination. Care coordination technology tools can support care coordination activities, such as registry, clinical decision support, care gap reporting, and patient outreach engagement technology. See additional considerations under “Address connectivity” below.
Practices can use a care coordination self-assessment tool, such as those referenced in the action steps below, to determine if additional technology support would be indicated.
Registry and care gap reporting
Practices can use an analytics platform to identify patients and group patients together who have similar needs. Your practice can then tailor interventions to meet the needs of a population. For example, a practice can use data to identify those people who have not had a visit in the past year, or those who are due for colon cancer screening. Data can come directly from the medical records or from claims data that is submitted to the payor.
Care coordination software: Clinical decision support
Many EHRs have care coordination modules, which can be used to develop assessments and care plans. Alternatively, care coordination modules can be add-ons to EHRs. Care coordination software can support assessment, referral and coordination pathways (e.g., clinical decision-making support). Using a care coordination software module, a practice can develop an assessment with questions regarding a patient’s social health needs. If answers are positive, the software can be configured to provide referral pathways and prompt care coordination activities. For example, if a patient answers “yes” to questions on food insecurity, the assessment can prompt referral to local resources such as food banks, meal programs and nutritional supports. The system can also prompt the staff to reassess progress at the next visit.
While care coordination applications provide unique and useful functionality for structuring multidisciplinary care plans that bridge the health center with other relevant resources, care must be taken to avoid siloing of information or burdensome documentation workflows entailing duplicate data entry.
Action steps and roles
1. Establish a call to action for care coordination.
Suggested team member(s) responsible: Medical lead, care coordination staff, or QI staff.
To achieve effective care coordination, your practice needs to see yourself as a hub or center for coordination of patient care. While all providers within a patient’s support network need to collaborate, your practice should view itself as accountable for care coordination for empaneled patients and patients who have been assigned to your practice by their managed care plan.
- Identify a care coordination team who will be responsible for leading the evaluation, assessment and implementation of care coordination activities.
- Share with the care coordination team, why care coordination is important.
- Some areas to address:
- What is care coordination?
- Why does care coordination benefit staff and patients?
- Review proposed framework (assess, develop strategy, implement, monitor) to develop the care coordination activity.
- Identify and share some initial projects directed at enhancing care coordination.
- Invite and engage staff and patients to provide input on how they think care coordination can be enhanced.
- Discuss how to best incorporate feedback from patients.
- Use feedback from this activity and incorporate it into the assessment below.
2. Assess your practice’s current state of care coordination activities.
Suggested team member(s) responsible: Panel manager, QI lead.
- Begin by asking and answering the following questions:
- What does the practice hope to achieve by implementing interventions to change the care coordination process?
- Which patient needs are the responsibility of the practice to provide (e.g., care coordination within the practice)?
- Which patient needs will need to be addressed through external referral and collaboration (care coordination with entities outside the practice)?
- What resources are needed to improve the current state (e.g., data, input from care team members, input from care partners, such as hospitals, specialty, behavioral health, social needs)?
- Gather stakeholder input.
- Conduct interviews or surveys with patients and community members to understand their perspectives on current care coordination processes, challenges and areas for improvement.
- Conduct interviews with your care team to understand their perspectives on current care coordination processes, challenges, and areas for improvement.
- Analyze existing systems and processes.
- Review existing care coordination protocols, technologies and resources utilized by health centers.
- Explore how technology is currently being used to support care coordination. Then explore how technology could be harnessed to streamline care coordination, improve data sharing, and/or enhance communication among providers.
- Review existing formal and informal linkage agreements.
- Conduct an analysis to determine patient needs not yet fully addressed by existing agreements.
- Assess data on patient outcomes, satisfaction, and any existing quality improvement initiatives.
- The following resources can help your practice assess its current state:
- PhmCAT: Sections on population-based care, social health and behavioral health.
- Care Coordination Maturity Assessment: This resource addresses multiple domains that may be impacted as care coordination activities are undertaken.
3. Develop and implement a care coordination improvement strategy.
Suggested team member(s) responsible: Panel manager, QI lead.
- Develop your high-level care coordination improvement strategy.
- The high-level strategy is based on the results and insights from your care coordination assessment and your practice’s capacity or bandwidth.
- Establish clear objectives.
- Define specific, measurable, achievable, relevant, time-bound, inclusive and equitable (SMARTIE) goals for enhancing care coordination.
- Ensure that these goals align with the overall mission and values of your practice.
- Prioritize areas for improvement: Identify a limited set of key focus areas based on the assessment findings and your practice’s bandwidth, such as communication protocols, technology integration, staff training or patient engagement strategies.
- The following resources can help your practice develop your care coordination improvement strategy:
- Identify resources and infrastructure.
-
- As part of the implementation of the strategy, identify the resources and infrastructure needed to support care coordination at your practice.
- We have included in Figure 19 below some considerations by resource as you develop your care coordination implementation plan. Some of the resources may not apply to your practice.
FIGURE 19: CONSIDERATIONS FOR IDENTIFYING CARE COORDINATION (CC) RESOURCES
Resource |
Considerations |
|---|---|
Staff |
Dedicated time for the development, training and implementation of the CC activity. Defining ongoing staffing needs. |
Internal tools |
Electronic health record modifications. Data needs and technology needed to implement the CC activity. |
Process |
Development of workflows, training materials, communication plan, and job descriptions. Identification of what CC activities will be the responsibility of the practice staff. |
Funding and finance |
Explore benefits, such as Enhanced Care Management or community health workers, as well as financial resources that may be available through external partners, such as health plans or hospitals. |
Clinical decision-making support |
Medical staff, behavioral health, and patients as subject matter experts (SMEs). |
External support and data |
Information and resources required from the entity with which the clinic is coordinating (e.g., hospital, specialist, social health clinician). Data exchange requirements including the new California Data Exchange Framework (DxF) on privacy. |
- Develop staffing for care coordination.
- Determine who at your practice will be involved in care coordination.
- The PHMI Care Teams and Workforce Guide provides an overview on care coordination using a care coordinator or referral manager.
- Based on the population of focus and the intervention, develop staffing requirements and any job description changes to embed care coordination into your practice.
- The responsibilities of a person or people fulfilling care coordination roles should include, at a minimum:
- Manage the referral process.
- Assist patients with transitions; such as those to and from hospitals and other institutions.
- Help patients resolve logistical, financial and/or other barriers to a successful referral.
- Link patients with community resources.
- Follow up with patients within a few days of an emergency room visit, hospital discharge or discharge from a treatment facility.
- Ensure the safe transfer of patient data.
- Track progress (e.g., referral milestones).
- Assist patients who are having difficulties.
- Schedule follow-up and specialty appointments for and with patients
- Formalize this role through a job description or position description.
- Sample referral coordinator position description.
- Provide regular training and support to the care coordinator or referral coordinator (or similar).
- Develop or refine your policies and procedures for care coordination.
At a minimum, include all of the following:- Identifying patients who are eligible for care coordination.
- Defining the activities that are associated with care coordination (e.g., outreach, engagement, assessment, desired outcome).
- Managing the referral process.
- Ensuring the safe transfer of patient data.
- Tracking progress through closed loop referral (see referral milestones above).
- Identifying patients who would benefit from higher levels of care coordination, such as care management interventions, like Enhanced Care Management (ECM) (see the Key Activity 19: Provide Care Management).
- Develop or refine your referral protocols.
- Develop clear guidelines for when and how to make clinical referrals.
- Include criteria for urgent vs. nonurgent referrals.
- For each provider your practice will be referring to:
- Identify the information, format and process the provider requires to receive a referral.
- Share the information you will need back from the provider when the referral has been successfully made and/or once the service or support has been provided to ensure continuity of care and nonduplication of services.
- Formalize this through a written agreement or compact to ensure expectations on both sides of a referral are understood.
- In working with community agencies or organizations that provide social support, the specific information that can and should be shared will depend on the service. It is important to have a mutual understanding about that information, using a written agreement where possible. At minimum, if the referral did not include a warm handoff, there should be an expectation that the practice hears back from the organization to let them know whether the patient followed up on the referral. Sample primary care checklist suggestions for assessing referral process.
- An interoperable referral management system can help practices streamline the intake process, communicate with other providers and social service agencies, track the status and outcomes of referrals, and ensure that patients receive the appropriate level of care and support.
- Develop clear guidelines for when and how to make clinical referrals.
- Address connectivity.
For any providers that you are exchanging patient data with, your practice should develop formal agreements and processes. Here are some considerations to facilitate information sharing among providers involved in an individual’s care:- Integrate documentation platforms, where possible, and standardize how documentation is included in patient records.
- Ensure that behavioral health records are integrated into the overall EHR system to the extent permitted by law.
- Enable providers to access comprehensive patient information.
- Identify and assess participation in health information exchanges and/or social health information exchange systems, where feasible, to facilitate seamless sharing of patient information between clinicians. These exist in some communities and will develop over time. This explainer series from the California Health Care Foundation describes the new statewide health information exchange coming into effect in 2024.
- Understand when patient consent is required to ensure compliance with privacy regulations, such as HIPAA. Include consent processes in the referral protocols.
- Set expectations about the information that should be shared and develop processes for facilitating that exchange. As data that is used in a clinical setting will likely be different than information that is shared by community agencies or social support networks, it is imperative to have clear parameters around what types of information can be exchanged between your practice and your partners.
- Leverage community health information exchanges (HIE) to gain access to admission, discharge and transfer information. Absent being able to access an HIE, establish relationships with your local hospitals to be able to gain daily notification of your patients being discharged.
- Provide care coordination to patients.
- Provide care coordination to patients who need it in accordance with your care coordination policies and procedures and referral protocols.
- Embed care coordination into your practices daily workflow, including pre-visit planning. See Key Activity 5: Develop or Refine and Implement a Pre-Visit Planning Process.
- Provide referrals to care management (discussed in going deeper Key Activity 19: Provide Care Management), such as ECM for patients who require more intensive support.
- Discuss each referral with the patient to ensure the patient understands the reason for the referral.
Below is an example of a care coordination quality improvement strategy.
FIGURE 20: EXAMPLE OF CARE COORDINATION, QUALITY IMPROVEMENT STRATEGY
Area of Improvement |
Goal |
Why It is Important |
|---|---|---|
Development of registries and process to outreach to empaneled patients who have not engaged in care. |
Bring children and caregivers into care, and screen for social health needs or barriers. |
Supports increased access to preventive medical care and addresses barriers related to social health. |
Development of a closed loop referral pathway for social services when social health barriers are identified. |
To support patients and families in receiving services that will be beneficial to addressing social health barriers, including those that are culturally aligned and based in communities where they live. |
Health outcomes, including health equity and access, are improved when social health needs are met. |
Development of a referral pathway to specialty providers and the creation of a pathway to receive consult results. |
To optimize access to specialty services, including urgent referral, and to ensure consultation results are available to PCP. |
To ensure timely access for services, including urgent referrals. Receipt of consult information saves time and prevents duplication of services. |
Development of a process to follow up with patients after transitions of care, post hospitalization. |
To support optimal outcomes for patients post hospitalization and decrease the chance of rehospitalization. |
Transition from the inpatient (hospital) setting back to home often results in poor care coordination, which can lead to medication errors, repeated or incomplete diagnostic workup, and lack of clarity regarding what a patient needs post hospitalization. |
4. Monitor: Continuous quality improvement of care coordination.
Suggested team member(s) responsible: QI lead.
- Develop both formal and informal mechanisms to obtain feedback from providers, staff and patients on the effectiveness of your practice’s care coordination efforts and to identify areas for improvement.
- Establish key performance indicators related to care coordination. Consider using the Agency for Healthcare Research and Quality (AHQR)’s Care Coordination Quality Measures in Primary Care (CCQM-PC). Your performance indicators will vary based upon your improvement strategy and the needs of patients, but may include metrics, such as:
- Number of assigned patients engaged in care.
- Number of individuals with hypertension whose blood pressure (BP) is controlled.
- Percent of closed loop referrals by referral entity. Monitor and analyze metrics to gauge the effectiveness of your internal systems and how well each referral partner is promoting coordination and collaboration.
- Continue to build relationships with providers and community support agencies that are available to provide services to Community Health Center (CHC) patients.
- Consider developing and using a care coordination variance report. Here is a sample patient care coordination variance report.
Resources
KEY ACTIVITY #12:
Expand Family-Friendly Access to Care
This set of foundational activities provides two key ways that clinics can improve access to care for families.
KEY ACTIVITY #12A:
Provide Clinic Hours Beyond the Typical Work Day
This key activity involves all seven elements of person-centered population-based care: address social needs.
Overview
Practices may take many approaches to provide family-friendly access to care. A potentially transformative approach is to shift clinic hours beyond the typical work hours. For example, you may choose to offer early morning hours or evening hours at your clinic a couple of days a week, as needed.
Telehealth technology may also be used to supplement and provide flexible hours, as clinicians or other staff may be more able or willing to work early or late hours from their homes. By enabling clinicians to see patients remotely or off-site, telehealth also can reduce the overhead costs of running the practice for longer hours.
Families need accessible healthcare to ensure that children have the opportunity to grow and develop to their fullest potential. Meeting the twin goals of on-time well-child visits (WCVs) and childhood immunizations requires that children and families have access to preventive care. Flexible clinic hours can expand families’ access to care and could be a good match for staff preferences as they balance work and life responsibilities. As such, the AAP includes family-friendly office hours in its list of office strategies for improving immunization rates.
Beyond flexibility, practices should try to be compliant with DMHC timely access standards for appointment availability. All licensed CA managed care plans are accountable for providing this level of access to their members and annually monitor their contracted primary and specialty providers on these standards. Moreover, Federally Qualified Health Centers (FQHCs) also need to be in compliance with Health Resources & Services Administration (HRSA) requirements for hours of operation, which generally means providing extended hours.
Incorporating family preferences for expanded clinic hours is a strategy to foster equitable health outcomes through expanded access to care. Families with low-income or shift work may have very little flexibility with their working hours and multiple competing priorities for their time. Consider providing increased late afternoon and evening access on weekdays to accommodate higher numbers of visits during after-school and after-work hours. Additionally, consider providing weekend hours, such as limited Saturday morning to early afternoon hours.
In addition, this population may face multiple other obstacles to participating in regularly scheduled preventive care visits that are important to learn about, including need for medical interpreter services for non English-speaking members. Of note, the DMHC and DHCS mandate that medical interpreter services are available when needed during all appointments.
Action steps and roles
1. Review current clinic operating hours and available data on missed appointments.
Suggested team member(s) responsible: Director or QI lead
The practices’ data manager or QI lead should stratify the data on WCV completion and immunization rates to identify groups of children who are not meeting goals. Be sure to filter the data by patient demographics to identify subpopulations of children who are unable to keep appointments in the current system.
2. Learn family preferences about clinic hours.
Suggested team member(s) responsible: Staff member
Practice leadership should identify a staff member or peer leader who is very skilled in empathic listening to reach out to parents and families to learn what gets in the way of children participating in WCVs and being immunized. Ask open-ended questions about families’ preferences for accessing care. You could include specific questions about times that would be convenient to the family.
3. Query staff to learn their preferences about working hours.
Suggested team member(s) responsible: Human resources staff or clinic leadership.
Clinic leadership or human resources staff may query the staff team along similar lines, asking about their perception of what gets in the way of families participating in care and their preferences about working hours.
4. Test flexible clinic hours.
Suggested team member(s) responsible: Director
Review what you learned and run a small-scale test, scheduling families to fill slots in one or two shifts of the preferred flexible clinic hours. Continue testing different time slots until the team is satisfied that you have learned as much as you need to designate an expanded clinic schedule. Be aware that this step may need to be repeated at intervals to gauge emerging preferences of patients and staff.
5. Designate an expanded clinic schedule and track the results.
Suggested team member(s) responsible: Director, human resources staff, QI lead
Implement a clinic schedule that incorporates the most-attended appointment windows. Draw staff time based on staff preferences to the extent possible and partner with staff to minimize disruptions in work/life balance. QI lead should review the rate of kept appointments during the flexible hour windows, and compare them to the rate of kept appointments during usual business hours.
For additional interventions to improve appointment access, consider open access scheduling and/or same-day appointments, using a similar careful testing and implementation approach.
Resources
KEY ACTIVITY #12B:
Incorporate Prevention Activities within Sick Visit Appointments
This key activity involves all seven elements of person-centered population-based care: operationalize clinical guidelines; behavioral health integration; address social needs.
Overview
Ensuring that prevention activities are incorporated into sick visit appointments expands access to care and facilitates a whole-person care approach. This creates opportunities to build interventions that are responsive to patients’ and families’ needs and preferences for engaging in the health system.
Sick visits provide a chance for pediatric care providers to incorporate elements of well-care visits:
- Health history.
- Physical developmental history.
- Mental development history.
- Complete physical exam.
- Health education and anticipatory guidance.
The American Academy of Pediatrics and the American Academy of Family Physicians recommend that children with mild illnesses receive vaccinations on schedule. Importantly, there is no health benefit to waiting to vaccinate, if a child has a mild illness. In fact, it is vital that children receive recommended vaccines on time so they are protected against serious disease.
Children can still be vaccinated if they have:
- A low-grade fever.
- A cold, runny nose, or cough.
- An ear infection (otitis media).
- Mild diarrhea.
Providing essential elements of WCVs during sick visits meets the patient and/or family where they are and maximizes the value of their time in the clinic with a focus on prevention. A sizable percentage of a clinic’s patient population will only seek care when they require a sick visit, so it makes sense to provide as much opportunity for quality care during these visits as possible.
Patients and families with lower socioeconomic status are likely to benefit from accessing preventive care whenever they are able to make time to visit the clinic. For example, caregivers who balance competing demands may struggle to keep scheduled well-child visit appointments and benefit from their child having the opportunity to engage in preventive care during a sick visit. Due to financial constraints, patients and their families also may prioritize urgent care over routine or preventive care.
Clinical decision support to prompt the care team to attend to well-child or preventive care during all visits is an effective strategy. Ideally, these could be positioned to be available to the extended care team and not restricted to the medical provider. Prompting strategies can be reinforced through the availability of care guideline-driven order sets and standing orders (see above) available in the EHR.
Care quality and care gap reports, analyzed against visit history can be utilized to track progress by provider and care team in leveraging sick visit opportunities to meet guidelines.
Action steps and roles
1. Consider providing additional time for sick visits that will include WCV activities when scheduling the appointment.
The office staff who are scheduling sick visits can be helpful at that by identifying that the child is due or overdue for well-child care and booking the visit as a well-child visit and problem-directed visit and providing a longer visit. Additionally, office staff can use patient messages, medication refill requests, and phone calls as touchpoints to screen for preventive care needs and opportunities.
2. Use pre-visit planning.
Suggested team member(s) responsible: QI lead, care team lead, frontline staff.
Use a pre-visit planning process to identify which patients with scheduled sick visits would benefit from the inclusion of well-care visit (WCV) activities. Determine priority WCV activities to include for each sick visit, such as administration of recommended immunizations. See Key Activity 5: Develop of Refine and Implement a Pre-Visit Planning Process for more information.
3. Empower rooming staff to engage patients in the decision to do the preventive care activity.
Suggested team member(s) responsible: Director or care team lead.
Screenings, especially behavioral health screenings, require rooming staff to read the room to decide whether to go ahead with the screening. Considerations include that screenings can lengthen a visit and/or raise topics that patients may not be prepared to tackle when feeling unwell. Parents may also be more stressed, sleep-deprived or worried during a sick visit, potentially biasing results of screening. Care team leaders can empower rooming staff to offer screenings and to express the importance of patients’ own priorities, especially if patients feel limited by their time or are feeling too unwell to complete screenings.
4. Test new and adapted practices and processes to develop improved workflows and standard protocols for implementing WCV activities during sick visits, focusing first on prioritized areas for improvement.
Suggested team member(s) responsible: QI lead with frontline staff (as appropriate for the WCV activity of focus) and patients their families.
Coordinate with the clinic’s efforts to improve reliability in meeting WCV recommendations. Consider using the individual WCV resource pages at AAP’s parent-facing website HealthyChildren.org to design, organize, and improve the inclusion of WCV activities during sick visits. Consider testing different versions of who does what, where, when, and how, and you might be able to leverage technology to automate or partially automate some of WCVs. See Key Activity 2: Assess and Improve Reliability in Meeting Well-Child Visit (WCV) Recommendations.
Ensure that your practice is benefiting from billing for a concurrent WCV and evaluation and management (E/M) services, for which higher reimbursement is available, if correctly coded.
You may also consider extending these workflows and protocols to implement WCV activities during other visit types as well, including nonurgent follow-up visits for chronic conditions (e.g., asthma, ADHD).
Peer example: At Children’s Hospital Primary Care Clinic (CHPCC) at Vanderbilt, a quality improvement team developed key drivers and used a people-process-technology framework to devise three interventions to reduce missed opportunities for WCVs at acute visits for patients overdue for those services. Key drivers included: an electronic indicator based on novel definitions of early and periodic screening, diagnosis and treatment (EPSDT) status (e.g., up-to-date, due, overdue, no EPSDT); a standardized scheduling process for acute visits based on EPSDT status; and a dedicated nurse practitioner to provide WCVs at acute visits. Data were collected for one year after full implementation. Implementation of interventions focused on people, process and technology significantly increased WCVs at acute visits within a feasible and practical model that may be replicated at other academic general pediatrics practices.
Going Deeper Key Activities
These are more advanced activities that build off of the foundational activities. They will help ensure your practice can achieve equitable improvement in your children's immunization and WCV rates.
KEY ACTIVITY #13:
Coordinate Care with Home and Community Visiting Services
This key activity involves all seven elements of person-centered population-based care: proactive patient outreach and engagement; care coordination; address social needs.
Overview
This key activity provides tips and considerations for expanding access to home visiting services, which may be available to patients as a managed care plan benefit or through other public services.
Home visiting is an evidence-based strategy in which a professional or paraprofessional renders a service in a community or private home setting. Home visiting programs employ home visitors as a central component of a comprehensive service plan and vary widely with regard to population of the focus and goals. Home visiting initiatives are most effective when they are components of a comprehensive community-level early childhood system that reaches families as early as possible with needed services; accommodates children with special needs; respects the cultures of the families in the communities; and ensures continuity of care in a continuum from prenatal life to school entry.[55] As of 2020, 21 home visiting models met the criteria of the U.S. Department of Health and Human Services for evidence of effectiveness through the Home Visiting Evidence of Effectiveness (HomVEE) review.[56]
Home visiting can be an effective strategy for improving health and health equity for populations. Home visiting can involve a range of skill sets, qualifications and expertise of the individuals conducting the home visit and address a range of purposes or topics. Home visiting programs are an evidence-based method to enhance school readiness and reduce child maltreatment,[57] as well as a promising strategy to buffer the effects of stress related to social needs, including poverty. Multiple types of home visiting programs are covered under Medi-Cal.
Pediatric clinics are essential to the success of home visiting programs, serving as a referral source to home visiting programs as a strategy to engage families in services and strengthen the connection between home visiting and the medical home. In their role, clinics provide community-based leadership to promote home-visiting services to at-risk young pregnant people, children, and families; can develop the capacity to identify and refer eligible children and pregnant people to state and local home-visiting programs; and may consider opportunities to integrate or co-locate home visitors in their clinic. Notably, one of the CalAIM Community Supports is home visiting and remediation for asthma.
For children and youth, home visiting can help buffer the negative health effects of poverty and boost lifelong health and well-being. Home visiting can promote child development, early literacy, school readiness, informed parenting, and family self-sufficiency.[58] Home visiting is most effective when it is integrated with the family-centered medical home in a community-based system of care for families with young children.[59]
Depending on the structure and content of the home visiting program, home visiting can help families attain economic stability by connecting them with community support services while also encouraging parents to enroll in training opportunities that lead to employment. High-quality home-visiting programs “deliver family support and child development services that provide a foundation for physical health, academic success, and economic stability in historically marginalized families that are at risk for the adverse effects of poverty and other negative health-related social needs.[60]
Implementation tips
Understand what home visiting services may be available to your patients, both through the health plan or in your community as a public benefit. For newborns, the California Home Visiting Program (CHVP) is an excellent resource. Examples of covered Medi-Cal benefits which also have home visiting components include:
- Enhanced Care Management and Community Supports (such as asthma home remediation, home-delivered medically tailored meals, respite care, etc.
- Early and periodic screening, diagnosis and treatment (EPSDT) home visiting nurse and health aide services.
- Durable medical equipment assessments.
- Intensive home-based services for those with specialty mental health needs.
- Home-based primary care programs (where offered by the patient’s health plan).
- Hospital at-home programs where available.
- California Children's Services.
- Personal care, homemaker care and respite services.
- Palliative and hospice care.
- Long-term care.
Resources
KEY ACTIVITY #14:
Provide Tailored Outreach, Screening and Managing of Treatment for Adolescent Behavioral Health
KEY ACTIVITY #14A:
Provide Proactive Inreach and Outreach to Help Adolescents Engage in Behavioral Health Care
This key activity involves all seven elements of person-centered population-based care: operationalize clinical guidelines; behavioral health integration.
Overview
The COVID-19 pandemic spurred rising rates of mental health disorders and distress, including a marked increase in adolescent emergency room (ER) visits for mental health conditions.[61] This reality heightens the need for effective inreach and outreach to adolescents needing behavioral health services.
Outreach consists of identifying the behavioral health (BH) care needs of adolescents in the community, while inreach involves identifying the same among your practice’s adolescent patients. An initial step in both inreach and outreach is communicating with the community and your adolescent patients and their families about behavioral health conditions and the availability of BH services.
In California, a large statewide investment for providers of pediatric services to be aware of is the Children and Youth Behavioral Health Initiative (CYBHI), which is aiming to expand access to school-based mental health counseling, as well as virtual behavioral health services and e-consults, regardless of insurance coverage. See the resources below for more information about this initiative.
How are inreach and outreach different for adolescents?
Adolescence and early adulthood is a time in life when mental health problems may arise for the first time, though the age of onset varies with the particular behavioral health diagnosis.[62] While significant numbers of adolescents experience behavioral health needs, young people seeking care from mental health professionals often report that their concerns are invalidated by healthcare practitioners.[63][64] Contact with mental health and health care providers can threaten young people’s sense of agency, turning them away rather than towards connecting with mental health services. School-based counselors can be instrumental in providing effective outreach and inreach to adolescents.
These help-seeking patterns are complicated by the fact that many adolescents may be struggling with multiple sensitive issues, including but not limited to substance use, emerging ideas about sexual orientation and gender identity, bullying and abuse, body dissatisfaction, relationship issues, and changing physical development. Unfortunately, these are topics that not all adults feel comfortable discussing.
Implementation considerations
Rather than make singular recommendations regarding inreach and outreach to adolescents, teams should consider the combination of their patient and family needs and staff capacity. Adolescence is not a single entity. The social and emotional needs of a patient at age 12 differ from that of a 17-year-old and, therefore, their relationships to family and peers change, as well. Additionally, not all adolescents' developmental stages correlate with their chronological ages. Teams should consider opportunities for inreach and outreach that reflect these variations and nuances, especially when determining whether or not outreach is directed at the family unit or to the individual adolescent.
Inreach (reaching adolescents within the practice):
- Train primary care providers and medical assistants in nonjudgmental, empathic communication in order to increase the likelihood of adolescents disclosing when they are having mental health or other difficulties.
- Develop patient-facing materials for adolescents, including posters in the waiting room and brochures in exam rooms, affirming the confidentiality of disclosures made to the healthcare team and behavioral health services available at the practice. Additional considerations and resources around consent for adolescents are discussed in Key Activity 14C: Manage Treatment of Adolescents’ Behavioral Health Needs in Integrated Person-Centered Ways.
- Universal screening for behavioral health difficulties is a core part of an inreach strategy. See Key Activity 14B: Screen Adolescents for a Range of Behavioral Health Needs.
Outreach:
- As suggested above, many adolescents do not seek help for behavioral health from their primary care provider. The practice may consider partnering or building on existing partnerships with organizations such as schools, churches or community centers to promote the availability of behavioral health services and care. Potential community partners will vary based on a clinic’s setting and should be contextually driven.
- Practices can offer community presentations, workshops or classes directed at parents within the community to share supportive information and resources for families with adolescents.
Implementation tips
- Engage staff who are closer in age to adolescents and can incorporate communication strategies that better reflect adolescent preferences.
- Develop adolescent-specific treatment competencies with existing staff or consider hiring employees who come into practice with those skill sets and experience.
Resources
KEY ACTIVITY #14B:
Screen Adolescents for a Range of Behavioral Health Needs
This key activity involves all seven elements of person-centered population-based care: operationalize clinical guidelines; behavioral health integration.
Overview
This activity provides general recommendations on screening for behavioral health needs for adolescents (ages 12 to 18 years). This guide uses depression as an example, as most practices begin behavioral health screening with depression. As the clinical team develops skills and familiarity with screening adolescents for depression and staffing on teams includes individuals with expertise in treating and supporting adolescents with their mental health needs, the goal is to incorporate additional behavioral health screening strategies, such as screening for anxiety, suicide and unhealthy substance use. Patient concealment about depression, substance use and previous trauma history can be high for fear that report of such experiences will lead to emergency response and/or reporting to protective services. Developing trust with adolescents can be effective in combating this common and understandable inclination. Additionally, as mentioned elsewhere, giving adolescents the option to engage or not in screening and a further option to answer screeners through self-report via methods, such as tablet that protect confidentiality, may help.
Depression is among the leading causes of disability for all ages in the U.S. Children and adolescents who experience depression frequently have functional impairments in their school performance and in interactions with peers and family members. Depression can have long-term impacts and negatively affect children’s developmental trajectories. Children and adolescents with major depressive disorder (MDD) have higher rates of recurrent depression in adulthood, other mental disorders, and an increased risk for suicidal ideation, suicide attempts, and suicide completion.
Nationally, suicide is the second-leading cause of death among youth ages 10 to 19. Psychiatric disorders and previous suicide attempts increase suicide risk. Rates of suicide attempts and deaths vary by sex, age, race and ethnicity.
Developing a process for reliably screening all adolescent children for behavioral health conditions is important because recent research reports higher rates of depression, suicide attempts and suicide rates among Black children, compared to the past. Reasons are likely multifactorial and include factors such as socioeconomic status, experiences of structural and overt racism, family structure, neighborhood effects, and childhood adversity. Adverse childhood experiences (ACEs) have been shown to influence the likelihood of experiencing mental health conditions such as depression. Some hypothesize that lower engagement with mental health services, combined with adverse childhood experiences, result in high levels of unmet need in Black youth. Mental health disorders in Native American/Alaska Native youth likely arise from similar patterns of historic trauma, adverse childhood experiences, and substance use.
Implementation considerations
Implement universal screening and follow-up for adolescents, starting with depression screening.
As with depression screening for adults, the most commonly used instrument for depression screening in adolescents is the PHQ-9. Teams often start with one depression screening questionnaire for all age groups and then, as they develop skills and internal capacity at screening and managing behavioral health care, they consider utilizing tools specific to different age groups or populations. The PHQ-A is an adolescent-specific version of the PHQ-9 and, therefore, is a natural tool to transition to when seeking a screening tool more specific to adolescents. There are two HEDIS measures for depression screening, one specific to a validated measure of depression and another specific to the PHQ-9. While, in general, PHMI advocates the use of the PHQ-2 or PHQ-9 for depression screening, more generally, there are some practices who have developed familiarity and ease with utilizing other validated tools. For a summary of additional validated tools for mental health screenings for adolescents, the American Academy of Pediatrics compiled this table. As with depression screening for adults, it is important to use a validated tool for which staff have been adequately trained to administer, score and interpret.
For adolescents, screening responses can come from the patient or their caregiver but ideally adolescents are interviewed separately from their parents/caregivers. All positive screening results should lead to additional assessments to confirm diagnosis, determine symptom severity, assess suicide risk and identify comorbid psychological problems.
While it is an important practice to screen for depression, not all young people at risk for suicide will endorse or experience symptoms of depression. Depression screening is best utilized alongside suicide risk screening; for instance, using the PHQ-A and the Ask Suicide-Screening Questions (ASQ). As mentioned above, screening for suicide alongside depression screening may be achievable as your integrated behavioral health care model evolves or may be something that your team is ready to test now.
As your team develops confidence to assess and manage depression, expand to screen for other BH needs, such as anxiety and attention deficit hyperactivity disorder (ADHD). Consider tools, such as the adverse childhood experiences screen for adolescents (PEARLS), the Pediatric Symptom Checklist (PSC) and/or the CRAFFT for substance use.
Implementation tips
The workflow for depression screening among adolescents includes the following:
- Training staff on implementing adolescent-specific tools. This includes training staff to ask and score the tool and workflow considerations about identifying and implementing a different tool for patients as they age.
- Incorporating strategies into well and sick visits that normalize and help families prepare for interviewing adolescents alone. For example, letting families know at the 11-year-old’s well-child visit that next year’s visit will include a portion when the adolescent is interviewed alone and discussing what will be covered and legal rights around confidentiality.
- Troubleshooting with staff about what to do if families or adolescents do not agree with allowing the adolescent to be interviewed separately, such as normalizing the activity, suggesting for future visits and responding to family concerns and reservations.
Resources
Evidence base for this activity
- Garcia JL. Historical Trauma and American Indian/Alaska Native Youth Mental Health Development and Delinquency. New Directions for Child and Adolescent Development. 2020 Jan;2020(169):41–58.
- Patra KP, Kumar R. Screening For Depression and Suicide in Children [Internet]. PubMed. Treasure Island (FL): StatPearls Publishing; 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK576416/
- Viswanathan M, Wallace I, Middleton JC, Kennedy SM, McKeeman J, Hudson K, et al. Screening for Depression, Anxiety, and Suicide Risk in Children and Adolescents: An Evidence Review for the U.S. Preventive Services Task Force [Internet]. PubMed. Rockville (MD): Agency for Healthcare Research and Quality (US); 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK585407/
- Zuckerbrot RA, Cheung A, Jensen PS, Stein REK, Laraque D. Guidelines for adolescent depression in primary care (GLAD-PC): Part I. practice preparation, identification, assessment, and initial management. Pediatrics [Internet]. 2018 Feb 26;141(3):1–21. Available from: https://pediatrics.aappublications.org/content/141/3/e20174081
KEY ACTIVITY #14C:
Manage Treatment of Adolescents’ Behavioral Health Needs in Integrated, Person-Centered Ways
This key activity involves all seven elements of person-centered population-based care: operationalize clinical guidelines; behavioral health integration.
Overview
This activity provides general recommendations on treatment of adolescents’ behavioral health needs in integrated and person-centered ways. As with adults, evidence-based care practices include the following singularly or in combination:
- Psychopharmacology, including referring out or leveraging same-day consults with child psychiatrists (described below) when needed.
- Behavioral health interventions such as Motivational Interviewing, Acceptance and Commitment Therapy, Problem Solving Therapy-Primary Care, Cognitive Behavioral Therapy, Interpersonal Counseling, Behavioral Activation, Dialectical Behavior Therapy (DBT), and Acceptance and Commitment Therapy (ACT).
- Peer support.
For additional information regarding behavioral treatment in general, please refer to the PHMI People with Behavioral Health Conditions Guide activity around embedding evidence-based care practices. The provision of these services differs for adolescents, as it is ideally provided by clinicians who have training, experience and comfort in responding to the behavioral health needs of adolescents.
Model recommendations for treatment that resonate with youth include:
- Involving youth as partners in project design.
- Implementing and monitoring recommendations made by youth.
- Considering the ways that a fundamental understanding and respect for youth can be incorporated into ongoing outreach efforts.
Confidentiality and adolescent care
Youth list concerns about confidentiality as the number one reason they might forego medical care. For this reason, youth need assurances of privacy and confidentiality from their healthcare providers. However, many providers feel overwhelmed or in the dark about the myriad of laws governing confidentiality and their responsibilities in minor consent laws and reporting child abuse. It is beyond the scope of this activity to include all relevant details, but it is encouraged that teams take advantage of resources, such as Understanding Confidentiality and Minor Consent in California: An Adolescent Provider Toolkit and familiarize themselves with charts, such as California Minor Consent and Confidentiality Laws. Given that parents’ rights to access adolescent medical records depend upon the health service provided, who consented or could have consented for the service, and the service provision site, in most cases, parents will have a right to access their child’s records. However, in some cases, parents cannot access records until their teen provides them with written authorization.
Teams need to consider what processes and workflows are necessary to maintain confidential records in the EHR setting. This includes training staff to know how to document in a manner that maintains adolescent confidentiality. In addition, they should provide education about parental access to medical record information to adolescents and their families. As communication such as texting and portal emailing become more ubiquitous, teams must consider alternative mechanisms by which to communicate with adolescents about the elements of their medical record that they want to be kept confidential.
Implementation tips
As patients need a greater level of psychiatric care than can be provided in the health center setting, practices should refer and connect them with county-level mental health plan services. The mental health plan (MHP) in each county is responsible for providing or arranging for the provision of specialty mental health services (SMHS) to Medi-Cal beneficiaries in their county. SMHS are meant to support a beneficiary when the impact of their condition is severe enough for them to require the services of a specialist as opposed to a generalist in the field of mental health. The health center team continues to provide integrated care with an emphasis on care coordination rather than treatment provision. As an individual’s severity of mental health needs wax and wane, the health center could again be the provider of behavioral health treatment and support.
Many practices are not able to employ staff who have training and experience in working with adolescents. To address the dual pressures of the behavioral health workforce shortage and increasing rates of childhood mental health struggles, 37 states and the District of Columbia staff psychiatric consultation lines that offer free same-day telephone consultation with child psychiatrists.[65] In California, this resource has been offered since 2019 by the UCSF Benoit Children’s Hospital. UCSF Child & Adolescent Psychiatry Portal (CAPP) provides telephone consultation for pediatric primary care providers (PCPs) to help them manage common mental health conditions in their patients.
In addition, CAPP offers continuing medical education (CME) for PCPs, website resources for PCPs, patients and families, and direct virtual psychological consultation for families, and aids with care coordination for families having difficulty accessing needed mental health resources.
DHCS’s new Behavioral Health Virtual Services Platform launched for public consumption in January 2024 and offers technology-enabled behavioral health tools and services focused on adolescents and young adults: BrightLife Kids for parents and caregivers, young children, and adolescents and Soluna for teens and young adults.
In addition to knowing that such a service is available, integrated teams should consider familiarizing themselves with how to access such resources (e.g., typical wait times for connecting, conditions best suited for referral, etc.). In addition, teams can consider how to incorporate consultancy notes from the psychiatric consultation lines into the clinic records, including who has visibility, etc.
Resources
Evidence base for this activity
Zuckerbrot RA, Cheung A, Jensen PS, Stein REK, Laraque D. Guidelines for adolescent depression in primary care (GLAD-PC): Part I. practice preparation, identification, assessment, and initial management. Pediatrics [Internet]. 2018 Feb 26;141(3):1–21. Available from: https://pediatrics.aappublications.org/content/141/3/e20174081
KEY ACTIVITY #15:
Strengthen Community Partnerships
This key activity involves all seven elements of person-centered population-based care: proactive patient outreach and engagement; care coordination; address social needs.
Overview
Strengthening partnerships with community-based organizations that share the practice’s vision and goals for their patient population enables the practice to provide more holistic care to patients and leverage many of the strengths and resources available in the community. These partners provide various services and programs to the community, such as education, housing, food, transportation, employment and social support.
This activity provides considerations and tips for strengthening partnerships, although note that deep engagement in this work can require significant resources from your practice.
Many community-based organizations have a deep understanding of the needs and preferences of specific subpopulations and the resources and challenges that exist in the local context. They can support outreach and health literacy efforts, participate in collaboratively design by providing insight around a particular patient population, and provide resources and supports for patients.
Building and strengthening relationships with community-based partners can extend the reach and impact of practices by facilitating patient access to services that the practice is unable to provide. Through partnerships with organizations that provide housing supports, nutrition assistance, transportation, and other social health supports, practices can play an active role in helping to address the social needs of their patients. The PHMI Equity Framework and Approach should inform partnership development to ensure the work of partnership building is prioritizing community groups that experience injustice and structural violence.
Action steps and roles
1. Start by understanding the resources and partnerships available through Medi-Cal.
Suggested team member(s) responsible: Clinic operations and leadership staff who will liaise with community partners.
Resources include supports that are available to all Medi-Cal patients, such as transportation to medical appointments, as well as Medi-Cal Community Supports for eligible individuals with higher levels of social needs. The following is a list of social support resources that are available to Medi-Cal patients when eligibility criteria are met.
- Transportation to medical and other Medi-Cal-covered appointments.
- In-home supportive services, such as personal home care assistance for those who qualify.
- Community-based adult services, such as day programs outside the home for individuals who need assistance with activities of daily living.
For individuals with the highest needs, the 14 Medi-Cal Community Supports are:
- Housing transition navigation services.
- Housing deposits.
- Housing tenancy and sustaining services.
- Short-term post-hospitalization housing.
- Recuperative care (medical respite).
- Day habilitation programs.
- Caregiver respite services.
- Nursing facility transition or diversion to assisted living facilities.
- Community transition services or nursing facility transition to a home.
- Personal care and homemaker services.
- Environmental accessibility adaptations (home modifications).
- Medically supportive food and meals or medically tailored meals.
- Sobering centers.
- Asthma remediation.
For specific providers in your area, contact the provider services department of your Medi-Cal managed care plan to learn more about the providers of these services. With a list of contracted community-based organizations, your practice can start to build relationships and support ongoing social needs for your patients.
For an overview, DHCS has provided information about the current state of Enhanced Care Management and Medi-Cal Community Supports in the Community Supports Year 1 Summary and the Enhanced Care Management Year 1 Summary.
2. Complete an environmental scan to understand who your patients identify as trusted messengers and resources in their community.
Suggested team member(s) responsible: Health center leadership, community health workers, care coordination staff.
This can be completed by interviewing patients and families, especially with the assistance of community health workers as adept listeners. Confirm existing partner relationships. After that, a stakeholder map and community profile of key current and prospective partners can be developed.
For pediatric populations, key community partners include schools, libraries, child welfare agencies, food assistance programs, and community-based programs (e.g., early literacy, youth activities).
3. Convene partners as a work group to develop strategies and interventions to address health-related social needs.
Suggested team member(s) responsible: Health center leadership.
In some cases, your practice may serve as a convener, bringing partners together for collaboration to avoid relying on individual relationships with external organizations. Be clear on your asks and offers to ensure the relationship will be mutually beneficial.
Develop a shared aim statement with your partners as to why this work is important and your vision of what you hope to achieve. Following the aim statement and formalize your structure and system of collaboration accountability for progress in the form of ongoing pacing of meetings on a regular basis rather than relying on transactional relationships.
To ensure proper understanding of expectations, roles and commitments, memorandums of understanding should be developed. Of note, California has data-sharing requirements for clinics and community-based organizations that help with referrals, coordination and data-sharing. Some organizations will be required to share data through the California Data Exchange Framework (DxF) starting in January 2024.
4. Collaborate with your partners to co-develop and deliver on a shared set of strategies on a community approach to address health-related social needs.
Suggested team member(s) responsible: Health center leadership.
The practice should benchmark and collate approaches to identify potential interventions for addressing health-related social needs. Developing a driver diagram can help guide your efforts and to set priorities. Leverage CalAIM resources as part of your intervention plans.
Use workflow mapping tools, swim lane diagrams and checklists that clarify roles and plan initiatives. This allows for the practice to develop clear action plans clarifying leaders of intervention strategies, timetables and measures of progress and success.
Implementation tips
- Health centers are very adept at developing relationships in the community, but often are challenged in nurturing partnerships for a variety of practical reasons. A partnership starts with relationships, moves beyond referral for resources or support, and results in co-ownership for addressing community challenges.
- Be clear on being able to have an offer as well as ask when approaching a prospective partner. Nurture the relationships and avoid becoming transactional, ensuring the partnership has value for all parties and helps others fulfill their mission.
- Seek to understand your partner’s needs for results, data and reporting. Explore how the partnership can help your partner meet a need or pain point in their core business mission.
- Learn what is in place for your county through the Medi-Cal program and your managed care plans. If resources are not available, explore technologies that facilitate community referrals such as findhelp.org (formerly Aunt Bertha’s) and UniteUs cross-sector collaboration software.
- Going deeper in strengthening partnerships: Addressing community needs requires sustainable and effective partnerships over time. A future activity includes how your organization works with other community partners in an ongoing forum to address community needs. This often involves the health center as a backbone organization supporting a local collaboration governance structure for shared prioritization and action planning.
- On the horizon in strengthening partnerships: A mature partnership system in a health center includes assessing the effectiveness of the partnerships and finding ways to continuously ensure alignment so that partnership remain a positive force for all participants. Where possible, making adjustments that strengthen the partnerships can be explored (e.g., improved data sharing, pooling of resources to increase leverage in the community).
Resources
KEY ACTIVITY #16:
Offer Nonpractice-Based Access to Immunizations
This key activity involves all seven elements of person-centered population-based care: operationalize clinical guidelines; proactive patient outreach and engagement; address social needs.
Overview
Reliable, timely access to immunizations remains difficult for many patients and families for a variety of reasons. During the COVID-19 pandemic, childhood immunization rates declined, particularly for children in families living below the federal poverty limit and in rural areas. Practices can consider promoting vaccinations at community-based pharmacies or developing mobile vaccination centers as potential strategies to provide access to recommended immunization for children and youth.
Leveraging this intervention to improve equitable health outcomes and social needs
Children from families with lower socioeconomic status are less likely to complete all well-child visits (WCVs) and therefore less likely to benefit from vaccination strategies that revolve around use of WCVs. Providing alternate means for vaccination reduces barriers to access and can contribute to mitigating inequities in health and well-being experienced by children based on race, ethnicity, and class. This intervention may be particularly relevant for children living in rural areas, given that they have experienced lower childhood immunization rates than children living in non-rural areas.
Implementation tips
Pharmacy-based vaccinations: In many communities, pharmacies are widely and consistently accessible. In California, pharmacists may administer vaccines for persons three years of age and older if they meet certain requirements. Pharmacies must enter the immunization data into CAIR and inform the PCP within 16 days.[66]
One positive side effect from the COVID-19 pandemic is that more individuals and families are accustomed to receiving immunizations from a local pharmacy. Pharmacies are allowed to enroll in the Vaccines For Children program and administer childhood vaccines (three to 18 years) through 2024 as a result of the 2020 Public Readiness and Emergency Preparedness (PREP) Act.
Mobile vaccination centers: Tips and resources for designing and planning mobile vaccination are available through multiple sources, including the American Academy of Pediatrics (AAP) and the Centers for Disease Control and Prevention (CDC), among other organizations. Additionally, learn from others who have developed and executed similar interventions.
- The AAP offers guidance and supports, including but not limited to Planning an Influenza Vaccination Clinic and Checklist for Planning and Implementing a Flu Vaccination Clinic.
- The CDC also offers guidance and support, including but not limited to Planning Activities, Considerations for Planning Curbside and Drive-Through Vaccination Clinics, and Satellite, Temporary, and Off-Site Vaccination Clinic Supply Checklist.
- The California Department of Public Health also offers guidance and support on their website, The Immunization Branch of the California Department of Public Health.
- National Association of County and City Health Officials (NACCHO) also offers guidance and support, particularly for school-based vaccination clinics in their School-Located Vaccination Clinic Toolkit.
- The University of Minnesota National Resource Center for Refugees, Immigrants, and Migrants (NRC-RIM) provides examples of mobile vaccination as well as concrete tips and resources.
The academic literature provides evidence-based examples:
- Leibowitz A, Livaditis L, Daftary G, Pelton-Cairns L, Regis C, Taveras E. Using mobile clinics to deliver care to difficult-to-reach populations: A COVID-19 practice we should keep. Preventive Medicine Reports. 2021 Dec;24(101551):10155
KEY ACTIVITY #17:
Expand Dyadic Care to Provide More Comprehensive Social and Behavioral Health Services
Overview
The Center for Advancing Dyadic Care in Pediatrics offers the following summary of dyadic care: “Infant and early childhood practitioners recognize the inextricable link between a young child and their caregiver and caregiving environment, making the relationship between the child and their caregiver and environment the focus of interventions. Dyadic care in pediatric primary care means expanding the focus of pediatric visits to include screening and support for caregivers, families and other environmental factors that will inevitably impact child health. Typically, dyadic care is provided by another member of the healthcare team, such as a licensed behavioral health provider or a community health worker who works alongside a pediatric healthcare provider.[67]
Why this matters
Dyadic care supports child development and mental health by treating children and caregivers together. Dyadic therapy models, such as HealthySteps and child parent psychotherapy (CPP) have a strong evidence base[68][69] for focusing on the dyadic infant and caregiver relationship to mitigate effects of trauma and adversity experienced in early childhood.
Technology Considerations
Technology-enabled screening can be utilized to screen caregivers directly in the EHR, in applications used by care coordinators, and directly to patients via patient-facing outreach and engagement technologies.
Screening results may already exist for caregivers who are already enrolled patients. Health centers will need to determine a strategy to link results to the pediatric record and, where possible, to the caregiver’s record and manage any needed referrals.
Implementation tips
Medi-Cal reimbursable dyadic services, which may be available through your MCP, include:
- Dyadic behavioral health (DBH) well-child visits, which can be delivered as part of the HealthySteps program, a different DBH program, or in a clinical setting without a certified DBH program, as long as a number of key components are included.
- Dyadic comprehensive community supports services focused on supporting coordination and access to clinical and community-based services.
- Dyadic psychoeducational services.
The dyadic care benefit does not require a documented behavioral health diagnosis, given the recognition that these services, directed to a high-risk caregiver, are medically necessary for the child’s well-being.
Family therapy is also covered as a Medi-Cal benefit.
In addition, several services provided to the caregiver during a child’s visit are covered, regardless of whether the caregiver is a Medi-Cal member, including:
- Brief emotional and behavioral assessment.
- ACEs screening.
- Alcohol and drug screening, assessment, brief interventions, and referral to treatment.
- Depression screening.
- Health behavior assessments and interventions.
- Psychiatric diagnostic evaluation.
- Tobacco cessation counseling.
DHCS details dyadic services and their coverage in All Plan Letter 22-029. See the PHMI People with Behavioral Health Conditions Guide for more nuance about depression and alcohol and drug screening for adults.
Resources
KEY ACTIVITY #18:
Continue to Develop Referral Relationships and Pathways
This key activity involves all seven elements of person-centered population-based care: operationalize clinical guidelines; pre-visit planning and care gap reduction; care coordination; address social needs.
Overview
Delivery of primary health care encompasses not only preventive services and coordination of medical and behavioral healthcare but also referrals for social supports, dental care and other needs of patients, such as weight management or parenting programs. As a result, coordination of care is more complex and often involves referrals outside the practice structure. Examples include referrals from the practice to a provider, such as medical specialty providers, behavioral health, and social services providers, such as the Supplemental Nutrition Program for Women, Infants, and Children (WIC), CalFRESH, CalEarn, the Employment Development Department (EDD) for paid family leave or to a program which will support health and well-being. A referral network also includes acute and subacute facilities, such as hospitals, emergency departments and residential treatment facilities where a patient may receive treatment and the outcome of treatment is necessary for the ongoing care of the patient in the practice.
This activity addresses common steps that your practice can take to optimize both the referral pathways and outcomes. The practice of closed loop referrals in which there is a feedback mechanism to ensure that a referral made by one provider to another is completed and followed up appropriately leads to greater patient and provider satisfaction. This activity builds on an inventory of existing referral services outside the clinic and identifies steps that can be taken to support the systematic management of the referral process.
When a patient requires a referral to obtain needed services outside the clinic, the process is a point of vulnerability and a significant percent of specialty referrals aren’t completed, in part due to missing information, misguided referrals and faulty communications.[70][71] If a referral is not completed, patients may not receive needed services, which can lead to decreased quality of care, decreased patient and provider satisfaction and ultimately poorer health outcomes.[72] The National Committee for Quality Assurance (NCQA) recognizes the importance of referral networks and their management as a core component of person-centered medical home activities.[73] Building a reliable network of service partners and processes to provide information necessary to inform referrals, as well as having mechanisms to track referral results, is an important part of providing coordinated care that is person-centered.
A major contributor to inequity in health outcomes is unequal access to specialty services and resources to help patients with their condition.[74] The heart of this activity is to empower both the care team and patients through development and maintenance of a robust process to help patients access medical, behavioral health and community resources.
Many factors can impact whether or not a patient accesses a referral, including language, culture and lack of understanding of why the referral is being requested. Lack of understanding of why a referral is being sought is often a barrier for patients to follow up with a referral, particularly if a patient is not experiencing symptoms.
When appropriate, referrals for social needs and to community health programs can help address barriers, including those around transportation, language, and basic needs of food and housing stability, all of which are associated with poorer health outcomes.
Electronic support for providing access to the care team of referral sources is important in the EHR (requiring continuous updating of the database) and for care managers. For care managers/coordinators, externally maintained electronic referral databases are available.
Ability to track referrals (closed loop) remains challenging for most EHRs, and often requires partially manual processes in EHRs and care coordination/population management applications. These manual processes are often facilitated through the construction of a separate registry in which teams can log appointments, track the referral and document completion. This approach requires some process for documenting and updating status in the orders in the EHR.
Action steps and roles
1. Identify types of referral partners that your practice needs and gaps in resource availability.
- Some examples to consider: High volume specialties (e.g., allergy, behavioral health, occupational therapy, physical therapy, pulmonology), parenting support programs, and social services providers.
- In areas where you have gaps in referral providers, telehealth services may be an option. For further information on telehealth services, including e-consult, synchronous, asynchronous, and e-visits, contact your managed care plan and/or refer to Telehealth Reimbursement Guide (Pages 14-16). Referral processes and tracking are also important to establish for telehealth as well as in-person services.
- Note that there is a shortage of behavioral health clinicians in many parts of California. As you continue to expand your network of off-site behavioral health providers to meet pressing behavioral health needs, also consider behavioral health integration strategies, including expanding your practice’s capacity for providing integrated behavioral health services. See the PHMI People with Behavioral Health Conditions Guide for more about deepening and expanding integrated care.
- Work with the pediatric care teams to identify gaps in referral resources that could enhance implementation of evidence-based care.
- Use social health screening results that have been disaggregated by REAL and SOGI alongside patient and family feedback to identify unmet needs for which resource relationships have not been established.
2. Assess what tools would be beneficial for the core elements of your referral process.
Examples include (see resources below):
- Referral request form.
Determine what information is required for the provider who is receiving the referral. Information may include the requested service, timing (urgent vs. standard), minimum necessary information, such as patient contact information and applicable demographics, and appropriate clinical and social support questions.
- Referral tracking spreadsheet or software.
Information in a tracking system can include the date of referral, appointment status, and whether follow up is needed. Reach out to your Medi-Cal managed care plans as you are developing referral tracking processes. The MCPs are required to show that Medi-Cal patients are being connected to the services that they are eligible for and referred to; this includes preventive services, specialty services and social services. The MCP may be a good resource for tools such as those needed for tracking and reporting.
- Referral workflow diagram.
A visual representation or workflow diagram can support staff in the referral process. IHI’s Closing the Loop: A Guide to Safer Ambulatory Referrals in the EHR Era provides a visual 9-step closed loop referral process for specialty referrals as well as suggestions for improving the process.
3. Assess what tools would be beneficial in enhancing and tracking your referral process.
- Referral guidelines:
- For social services, positive responses to screening questions and tools may be the prompt for referral.
- Other types of referrals may be optimized by having documented referral guidelines, such as information needed by specialty provider in order to best answer referral questions.
- Communication templates:
- For high volume or frequent referral types, a standardized template for communication between the clinic and referral staff can help ensure that that essential information is conveyed efficiently. Examples may include referral letters, progress notes, post visit summaries of plan of care.
- Patient education materials (develop in conjunction with referral network):
- Educational materials and resources for patients that explain the referral process and what to expect can enhance patient understanding and support referral completion. In addition, consider training medical assistants as well as any dedicated care coordination staff in evidence-based communication techniques such as teach-back or motivational interviewing to leverage team based-care in supporting the patient to follow through with the referral after the visit.
4. Develop approaches to fill resource gaps.
- Outreach to your Managed Care Plan (MCP) to understand what resources are available. MCPs are required to have on-line provider directories which include specialists, which can be a resource used by a clinic to help find contracted specialists near the patient's home. In addition to comprehensive networks of over a dozen core specialty providers and information on behavioral health and substance use resources, many MCPs are building links to access community based resources in addition to the 14 Medi-Cal Community Supports through referral platforms that act as a “hub” to coordinate social needs for patients.
- Identify external providers and community resources that can serve as partners in care, and use the established referral process to fill gaps in care they can address.
- Meet/schedule time with high volume providers, including community based organizations to develop a mutual understanding of goals of referrals and opportunities for development of shared process (e.g. referral form).
- The American Academy of Pediatrics offers a sample tool to develop a resource list.
5. Regularly review and update the referral processes and network.
- As new patient needs are identified, use that opportunity to identify potential resources and expand the referral network. If practices have trouble accessing a contracted specialist for their patient because of either overly long wait times or that they are longer accepting new patients, the MCP is required to approve an out-of-network referral to a more available specialist.
- On a periodic basis, review referral tracking reports to identify referral resources that are used most frequently and use that information to reinforce the relationships and provide feedback on value.
- Review referral tracking reports to identify resources for which loop closure is lacking or from whom required information is not being received on a regular basis. Outreach to these organizations to reinforce expectations or if necessary, identify a replacement resource for the network
- For going deeper in tracking quality improvement metrics, practices can develop metrics to assess the effectiveness of the referral network. This might include tracking referral completion rates, patient satisfaction, and time from referral to specialist appointment.
Resources
KEY ACTIVITY #19:
Provide Care Management
This key activity involves all seven elements of person-centered population-based care: operationalize clinical guidelines; proactive patient outreach and engagement; care coordination; behavioral health integration; address social needs.
Overview
Led by a care manager – a licensed clinician or a nonlicensed trained individual under clinical supervision – care management is an intervention intended to support the highest need individuals within your practice. Typically, these are individuals with multiple complex chronic illnesses and/or comorbid chronic medical and behavioral conditions. The services are more focused, require the development of a person-centered care plan, and are of higher intensity than care coordination services. A patient must consent to participate in care management activities. A care manager works directly with the patient and multidisciplinary care team members to identify, plan and implement person-centered goals and care. The care manager supports the individual in identifying and coordinating resources and referrals, as well as supporting self-management activities to attain optimal wellness.
There are varieties of care management, which differ in the population of focus, goals and intensity of support. The National Committee for Quality Assurance (NCQA) designates the following designations for care management programs:
- Complex case management.
- Transitional case management.
- High-risk and high utilization.
- Hospital case management.
- Organization-defined programs.
The DHCS Enhanced Care Management benefit is available to a range of high needs Medi-Cal MCP enrollees. With respect to pediatrics, children who are eligible for ECM have complex physical, behavioral, developmental and/or oral health needs (e.g., California Children Services, foster care, youth with clinical high-risk syndrome or first episode of psychosis).
Care management provides a higher level of support to individuals who have medical, behavioral health and/or social needs that impact their ability to access appropriate levels of care. Individuals may be receiving frequent ER and hospital care that could be avoided with care management activities and/or patients may have significant social barriers (e.g., housing, food, substance use) that prevent them from accessing preventive and wellness care.
As part of care management, the patient’s medical, behavioral health and social health needs are directly addressed as part of the assessment and prioritized according to the patient's goals. For example, supporting the patient’s concerns around securing stable housing may be a first step to achieving better health. Addressing health-related social needs helps in reducing health disparities among different populations. Individuals with lower socioeconomic status or limited access to resources can be provided with resources to support these areas.
What patients are eligible for care management?
Individuals eligible for care management have high levels of need in one or more of the domains of medical, social or behavioral health. Children with complex medical needs or who require intensive support post hospital discharge may be eligible.
Medi-Cal members can also be connected to community support services to help address their health-related social needs, such as access to healthy foods or safe housing, to help with recovery from an illness.
What patients are eligible for Enhanced Care Management?
In California, Medi-Cal beneficiaries who experience high care management needs may be eligible for a Medi-Cal benefit known as Enhanced Care Management or ECM. Your MCP can provide you with details on patient eligibility and the requirements needed to provide ECM services to your patients. ECM is available to specific groups of Medi-Cal members, including the following, which pediatric practices may encounter:
- Adults, unaccompanied youth and children, and families experiencing homelessness.
- Adults, youth and children who are at risk for avoidable hospital or emergency department care.
- Adults, youth and children with serious mental health and/or substance use disorder needs.
- Children and youth enrolled in California Children’s Services (CCS) or CCS Whole Child Model with additional needs beyond their CCS condition(s).
- Children and youth involved in child welfare (foster care).
- Adults and youth who are transitioning from incarceration.
- Pregnant and postpartum individuals; birth equity population of focus (starting in 2024).
How do we refer a patient who we think would benefit from ECM?
If you have a patient who may be a candidate for ECM or Community Sspports, you should contact the Medi-Cal managed care plan to inquire about services available through the patient’s health plan.
How can we provide care management services, including ECM services, in our practice?
Community practices are often well situated to provide care management services, as they are the site where patients seek or can be connected to care. Clinics may decide that they want to provide care management services, including ECM services. The following resources can help assess your capacity to provide care management services within your clinic structure.
Resources
Evidence base for this activity
- Chuang E, Pourat N, Haley LA, O’Masta B, Albertson E, Lu C. Integrating Health And Human Services In California’s Whole Person Care Medicaid 1115 Waiver Demonstration. Health Affairs. 2020 Apr 1;39(4):639–48.
- Tomoaia-Cotisel A, Farrell TW, Solberg LI, Berry CA, Calman NS, Cronholm PF, et al. Implementation of Care Management: An Analysis of Recent AHRQ Research. Medical Care Research and Review. 2016 Oct 23;75(1):46–65.
KEY ACTIVITY #20:
Strengthen a Culture of Equity
This activity builds off of Key Activity 4: Use a Systematic Approach to Decrease Inequities to provide strategies and in-depth resources that can help create or strengthen a culture of equity in your practice. The PHMI Equity Framework and Approach emphases that achieving long-term and sustainable improvements to health and racial equity for patients and the broader ecosystem requires a transformational shift at the organizational level. The following strategies can help practices strengthen a culture of equity:
- Demonstrate senior leadership ownership for and commitment to improving health equity.
- Understand and address internalized, personally mediated and institutionalized racism.
- This should include ongoing learning and development activities on the full range of health equity topics (e.g., anti-bias, structural racism, race-based algorithms).
- Build organizational capacity to support efforts to improve health equity.
- Establish practices and policies to promote workforce diversity and provide culturally and linguistically appropriate care.
- Support policy efforts to eliminate inequities driven by social drivers of health.
- This can take the form of joining advocacy efforts or participating in benefits created by recent policy reforms, such as connecting patients with Medi-Cal Community Supports for housing, asthma remediation or medically tailored meals. See Key Activity 7A: Develop a Screening Process for Social Needs and Adverse Childhood Experiences (ACEs) that Informs Patient Treatment Plans for a discussion on social needs.
Resources
Appendices
APPENDIX A:
Sample Idealized System Diagram
FIGURE 21: WEAVING YOUR MEASUREMENT STRATEGY AND LEARNING SYSTEM INTO PRACTICE OPERATIONS
The below graphic provides an example to visualize the flow of information between a practice’s measurement strategy and actions at the practice and care team levels, including how to use the information for continual learning and improvement.
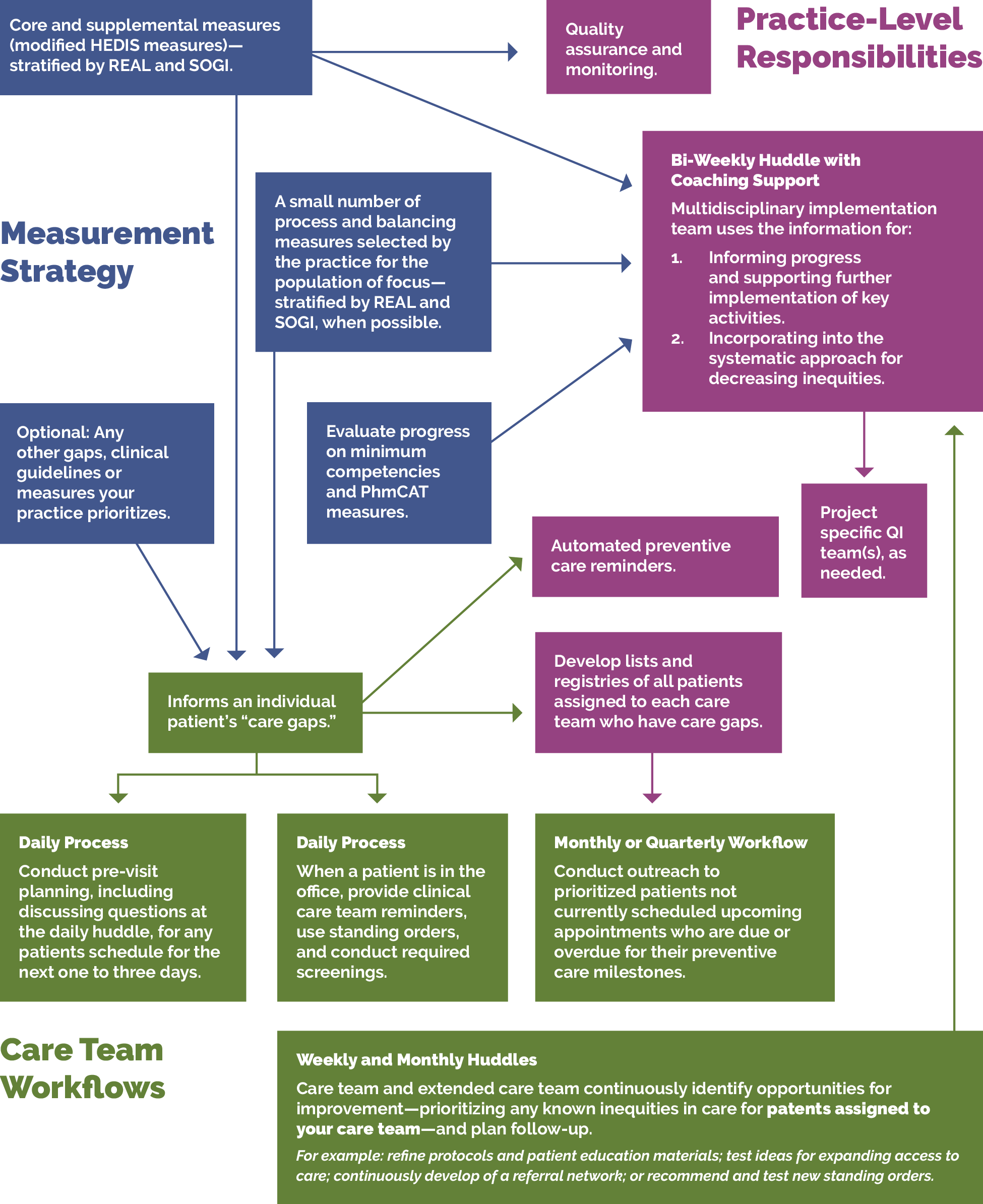
APPENDIX B:
Theory of Change
The key activities in this guide align with the PHMI theory of change for how practices can increase children’s immunization and well-child visit rates through three main drivers:
- Effective implementation of well-visit protocols.
- Patients eligible and due for visits and immunizations have the information, education and access needed for screening.
- Practices have needed resources and support.
FIGURE 22: PHMI CHILDREN DRIVER DIAGRAM
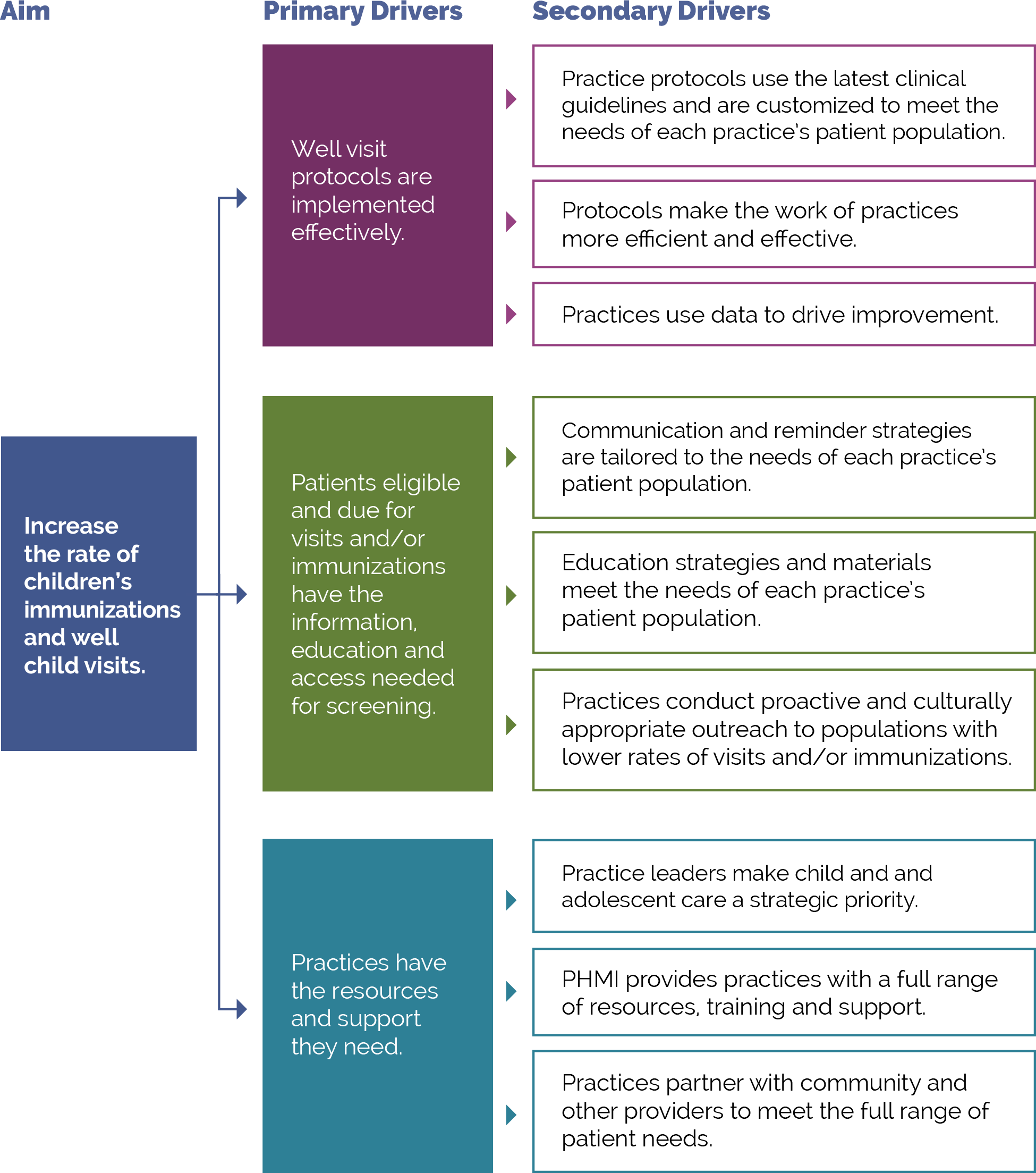
APPENDIX C:
C: Developing a Robust Measurement Strategy
FIGURE 23: DEVELOPING YOUR MEASUREMENT STRATEGY MILESTONES
The visual below illustrates the key milestones in the development of a robust measurement strategy.
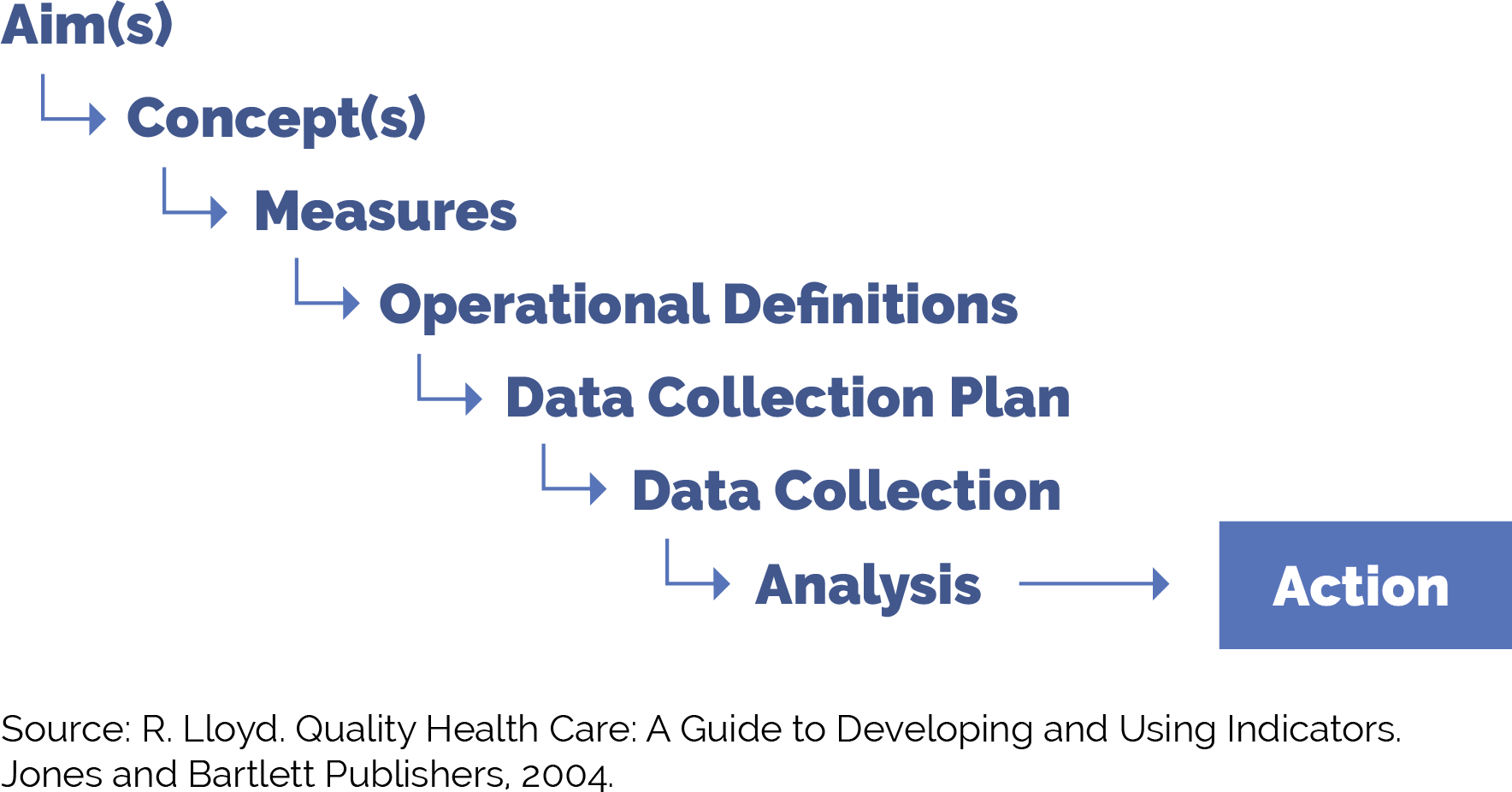
FIGURE 24: DEFINITION AND EXAMPLES FOR MEASUREMENT STRATEGY MILESTONES
Figure 24 provides guidance on each of these milestones as you work to put in place a robust yet practical measurement strategy.
Milestone |
Definition |
Example |
|---|---|---|
Aim(s) |
The overall goal(s) of the improvement effort. “What are we trying to accomplish?” We often recommend sub-aims to focus your team on intermediate goals. You can develop data-informed specific, measurable, achievable, relevant, time-bound, inclusive and equitable (SMARTIE) goals focused on increasing adherence to specific AAP preventive care guidelines year over year among attributed patients or subpopulations of patients. |
Our overall aim is to increase adherence to AAP preventive care guidelines among patients. Example sub-aims: By December 2025, 95% of children 18 months of age will receive all recommended measles-mumps-rubella (MMR) vaccines or have documented parental declination. By December 2025, we will increase the percent of children zero to 30 months of age whose parents have Spanish as a preferred language who were sent a reminder in Spanish for recommended immunizations during the measurement year. |
Concept(s) |
A general abstract notion (approach, thought, belief or perception) related to the aim(s) of focus. |
|
Measures |
Specific objective ways to determine the extent to which an aim has been met or to determine if there has been improvement in the concepts of focus. Measures help us to answer the second question in the model for improvement: “How will we know that a change is an improvement?” Measures generally fall into one of three types:
|
See below for example outcome, process and balancing measures. For the following examples, we will examine the percentage of two-year-old children who have received the 10 HEDIS-reported vaccinations. |
Operational definitions |
Detailed descriptions in quantifiable terms of what to measure and the steps to follow to do so consistently each time and over time. The operational definitions help make the measures clear and unambiguous and often contain criteria for inclusion and exclusion and numerator/denominator. |
Percentage of two-year-old children who have received the 10 HEDIS-reported vaccines, operational definition. See CMS117v11 for more information. Stratifying these data by type of vaccine (e.g., Hib, MMR) can provide additional information and insight to inform improvement efforts. |
Data collection plan |
A detailed set of instructions that generally includes:
|
Percentage of two-year-old children who have received the 10 HEDIS-reported vaccines, data collection plan. Who:
How:
Where and how the data will be stored:
When the data will be collected:
How often:
|
Analysis and action |
The process of analyzing the data, including instructions for the analysis and visualization of the data, disseminating the data to relevant parties, and using the data to track progress and guide improvement efforts. |
The improvement team reviews the percentage of two-year-old children who have received the 10 HEDIS-reported vaccines on a monthly basis, and the care team and panel manager review the data subsequently once per quarter or every six months for ongoing monitoring. |
POPULATION HEALTH GUIDE FOR UNDERTAKING 3 PART DATA REVIEW
The three part data review is a tool that can be used to advance work related to population health. It draws on asset-based inquiry, to surface to identify needs and opportunities to understand the ways in which systems have discarded or undervalued the assets of individuals and communities. Groups can then work together to ensure that all can contribute to advancing population health and well-being and dismantling inequities. Access the full resource.
APPENDIX D:
Guidance on Technological Interventions
EHRs were primarily designed to manage individual patients rather than groups of patients. However, over time EHRs have increasingly added functionality for population-level quality reporting and management and some degree of care planning and care coordination, especially to support value-based care tracking and reporting. Practices should evaluate your EHR capabilities against specifically designed population management applications. While these applications require interface with the EHR, they generally offer additional functionality. While EHR solutions are integrated with EHR data, they still usually require import of data from outside sources to be optimally useful. Managed care organizations may provide care coordination and population management applications, but usually only for their own enrolled patients. EHR-based solutions may also pose challenges where groups of practices using different EHR solutions are collaborating in value-based care contracts.
In value-based care arrangements, practices are responsible for attributed patients who may have never been seen. Since these patients do not have records in the EHR, practices need to consider how they can manage these patients to engage them into care at the practice in the absence – at least initially – of the patients having records within the EHR. If your practice is using freestanding applications for this, they need the capacity to handle these attributed patients who have not been registered as patients.
FIGURE 25: CORE POPULATION HEALTH MANAGEMENT FUNCTIONALITY REQUIREMENTS
Figure 25 includes the technical functionalities required to support population management for pediatrics. These requirements can guide the evaluation of existing solutions or guide the development of requirements in evaluating potential new applications. The table also indicates the data sources required to enable the functionality.
# |
Functionality |
Population Health Management Requirement Description |
Data Acquisition Dependency |
|---|---|---|---|
1 |
Care guidelines |
Identify care gaps for all people with behavioral health conditions against care protocol. Care guidelines may be presentable to the clinical provider or support team at point of care through the EHR, in visit workflow as pre-visit prep or team huddle, through registries as above, and aspirationally as prompts to patients and caregivers. |
Commercial EHR-embedded guidelines provided by the vendor or customized by the practice. External source guidelines (clinical guidelines). Reference sites made available electronically. |
2 |
Registries |
Ability to produce registries (list or cohort of patients) organized to facilitate population management (e.g., children in age ranges relevant to measures and/or clinical standards, children sharing designated high risk criteria, such as medical, behavioral, social needs). Considerations for recognizing connection to the birthing person also include linking to registries of recently postpartum patients and pregnant patients in late third trimester or postpartum without delivery information, possibly due to delivery occurring at outside hospital system or birthing center. These registries should contemplate inclusion of functionality to trigger automated pre-defined action(s) and/or human-initiated action(s) for all or a defined subset of patients comprising the registry. A final consideration is the ability to manage children in the context of their families, requiring the ability to relate children to siblings for management purposes. Suggested HIT assets that can be leveraged to achieve this function include: EHR: Generate a list of patients who meet the criteria for inclusion in the population of focus. Track using an external database. Consider merging patients from an external data source, such as a payor, to have a complete roster. Population health management tool: |
EHR: Clinical data; scheduling data for appointments (e.g., how the WCVs are distinguished from other appointments or postpartum visits); pediatric-specific data (e.g., growth parameters, immunization data); immunization data; and screening data (see below). External data sources, such as: prenatal records, reference labs, specialty care, immunization registries, school health records, and social service providers’ data.. |
3 |
Clinical decision support (CDS) |
Care gaps should be displayed based on what is due with insight into previous results to support clinicians' ability to make decisions at the point of care for the provider and care team members supporting non-point of care management. Care guidelines may be presentable as clinical decision support to the clinical provider or support team at point of care, in visit workflow as pre-visit prep or team huddle, through registries as above, and as aspirational prompts to patients and caregivers. While her-based prompts are usually thought of as ideal, team-based care presents an opportunity for CDS to be presented to other members of the care team through other channels. The Five Rights Framework Clinical Decision Support: More Than Just ‘Alerts’ Tipsheet—September 2014 (cms.gov)is useful guidance to help health centers support decision-making across a wide range of the care delivery lifecycle, broader teams, and technology other than the EHR to look beyond office visits and providers. This is especially important to avoid alert fatigue and burnout. |
Internal EHR data. External source clinical data. Claims data (clinical lag should be noted). Electronic guideline specifications. Patient-contributed data. |
4 |
Care dashboards and reports |
Pediatrics dashboard: Population view by eligible study with sorting and filtering capability based on characteristics to be defined by the practice with the ability for the care team and case managers to document the actions completed; ability to see care gaps at a patient level and population level according to health center-prioritized care guidelines. Note that, to automate these reports, it is necessary to apply standardized data collection strategies against electronically specified protocols. |
Same as above (e.g., EHR data and external data sources, data from other sources of care). Claims data. |
5 |
Quality reports |
Same as above by quality measures, as opposed to care guidelines; ability to track HEDIS as well as customized measures and UDS. |
Quality measure specifications. Same as above (e.g., EHR data and external data sources, data from other sources of care). Claims data. |
6 |
Risk stratification |
The ability to categorize risk for patients and develop lists according to risk classification (e.g., tie to registry). Can be imported as externally generated risk score or calculated internally according to proprietary or customized risk algorithm. |
Data acquisition platform ingestion (already curated high-risk list ingested and utilized downstream in the journey). and/or Additional internal and external data sources to populate defined risk model. |
7 |
Inreach and engagement |
Allow for outreach to support pre-visit planning or post-visit care needs, such as assessments. Technology channels include population registry outputs; patient-facing applications, such patient portal; freestanding text messaging; and self-assessment or self-management applications. |
Same as above (e.g., clinical, EHR, etc.). Claims. |
8 |
Care management |
Allow for management of specific and unique care needs for high-risk patients. Care management requires the ability for multiple members of the care team to contribute to and rack elements of the plan. Challenges with freestanding care management applications include access to data from other sources of care, including the ability to track referrals, and workflow burden of staff utilizing multiple applications. Ability of the care management application to draw from and write back to the EHR is desirable but difficult to achieve. |
Care management protocols and appointment data (internal and external). Clinical data from external service providers. |
FIGURE 26: USE OF TECHNOLOGY FOR RECOMMENDED SCREENING FOR FOUNDATIONAL KEY ACTIVITIES
This table identifies strategies for using digital tools to complete appropriate screeners as recommended by clinical guidelines. Using technology to facilitate screening may streamline the workflow and preserve patient confidentiality where necessary.
ID |
Focus Area |
Completion of Digital Screeners |
Data Acquisition Dependency |
|---|---|---|---|
1 |
Depression screening |
In-office tablet-based screening and/or remote patient-facing application-based self-completed screening.* |
Population health and EHR integration of screener responses or, at minimum, scores. |
2 |
Anxiety screening |
In-office tablet-based screening and/or remote patient-facing application-based self-completed screening.* |
Population health and EHR integration of screener responses or, at minimum, scores. |
3 |
Unhealthy substance user screening |
In-office tablet-based screening and/or remote patient-facing application-based self-completed screening.* |
Population health and EHR integration of screener responses or, at minimum, scores. |
4 |
Social needs screening |
In-office tablet-based screening and/or remote patient-facing application-based self-completed screening.* |
Population health and EHR integration of screener responses or, at minimum, scores. |
*A workflow for identifying emergent behavioral health risks and a workflow for preserving patient confidentiality should be codified.
FIGURE 27: USE OF TECHNOLOGY FOR PATIENT OUTREACH AND PRE-VISIT PLANNING FOR FOUNDATIONAL KEY ACTIVITIES
This table outlines the use of technology to facilitate specific activities and potential technology solutions that can optimize the uptake and efficiency of in-office visits.
ID |
Technology Focus |
Patient Inreach and Pre-Visit Planning |
Data Acquisition Dependency |
|---|---|---|---|
1 |
Portal-based communication |
|
EHR interface and integration. |
2 |
AI-enabled chatbots |
Identifying issues that need to be addressed before an office visit that can be converted to telehealth visits. |
Population health and EHR incorporation of screening scores and responses. |
3 |
Text messaging |
Appointment reminders. |
EHR interface and integration. |
FIGURE 28: USE OF TECHNOLOGY FOR ENHANCED PATIENT ENGAGEMENT AND VIRTUAL CARE FOR GOING DEEPER ACTIVITIES
The table identifies technology solutions to engage patients asynchronously from office visits for a variety of use cases to enhance care and patient experience.
ID |
Focus Area |
Patient Engagement and Mobile Technology |
Data Acquisition Dependency |
|---|---|---|---|
1 |
AI-enabled Chatbots |
|
HR interface and integration. |
2 |
Remote medical devices |
|
EHR and population health integration. |
FIGURE 29: USE OF TECHNOLOGY FOR INNOVATIONS IN CARE DELIVERY FOR ON THE HORIZON ACTIVITIES
The table describes technology strategies that can enhance care delivery by using artificial intelligence and advanced technology tools.
ID |
Focus Area |
Artificial Intelligence (AI) and Innovation |
Data Acquisition Dependency |
|---|---|---|---|
1 |
Predictive analytics |
|
EHR integration, population health, and patient engagement application integration. |
2 |
Artificial intelligence-enabled diagnostics |
Advanced diagnostic tools that can use imaging, audio files, and EHR data to suggest diagnoses and care management plans. |
EHR integration and population health integration |
RECOMMENDED CITATION AND ACKNOWLEDGEMENTS
Recommended citation: Riley C, Baker L, Glauber J, Deane M, Donald F, Craig C, Rachman F, Esmond W. Children Implementation Guide. In: Coleman K, Mital M, editors. Population Health Management Initiative Populations of Focus Implementation Guide Series. 1st ed. Oakland, CA: Kaiser Permanente; 2024.
Acknowledgments: We gratefully acknowledge the contributions of the many staff and representatives of the Institute for Healthcare Improvement (IHI), AllianceChicago, Center for Care Innovations (CCI), JSI Inc and the Center for Excellence in Primary Care at University of California, San Francisco along with Pyramid Communications and Kaiser Permanente’s Population Health Management Initiative (PHMI) team for crafting this work.
In addition, we are grateful for the partnership of the Department of Health Care Services (DHCS), Community Health Center partners in PHMI, representatives from the California Primary Care Association and the Regional Associations of California (RAC) along with the many other academic, health plan and consulting partners who shared their expertise and insights freely as we collaboratively designed the initiative and created these guides.
Special thanks to the individual reviewers of this first edition of the Populations of Focus Implementation Guide Series who significantly strengthened this work, including: Jeff Norris, David Tian, Karen Mark, Palav Babaria (DHCS); Jennifer Sayles (Pop Health Learning Center); Roger Chaufournier, Christine St. Andre (IHI); Kathleen Figoni, Angela Sherwin (CCI).
Endnotes
- Borksy, A., et al. (2018). Few Americans Receive All High-Priority, Appropriate Clinical Preventive Services. Health Affairs, 37(6). DOI: 10.1377/hlthaff.2017.1248
- Centers for Disease Control and Prevention. (2019). Oral Health Surveillance Report: Trends in Dental Caries and Sealants, Tooth Retention, and Edentulism, United States, 1999–2004 to 2011–2016. Retrieved from https://www.cdc.gov/oralhealth/pdfs_and_other_files/Oral-Health-Surveillance-Report-2019-h.pdfThis link is external to health.gov. [PDF - 5.3 MB]
- Lebrun-Harris LA, Canto MT, Vodicka P. Preventive oral health care use and oral health status among US children. The Journal of the American Dental Association [Internet]. 2019 Apr [cited 2019 Oct 31];150(4):246–58. Available from: https://www.sciencedirect.com/science/article/abs/pii/S0002817718308328
- ABOUT BRIGHT FUTURES [Internet]. Available from: https://downloads.aap.org/AAP/PDF/Bright%20Futures/BF_IntegrateSDoH_Tipsheet.pdf
- Maria Trent, Danielle G. Dooley, Jacqueline Dougé, SECTION ON ADOLESCENT HEALTH, COUNCIL ON COMMUNITY PEDIATRICS, COMMITTEE ON ADOLESCENCE, Robert M. Cavanaugh, Amy E. Lacroix, Jonathon Fanburg, Maria H. Rahmandar, Laurie L. Hornberger, Marcie B. Schneider, Sophia Yen, Lance Alix Chilton, Andrea E. Green, Kimberley Jo Dilley, Juan Raul Gutierrez, James H. Duffee, Virginia A. Keane, Scott Daniel Krugman, Carla Dawn McKelvey, Julie Michelle Linton, Jacqueline Lee Nelson, Gerri Mattson, Cora C. Breuner, Elizabeth M. Alderman, Laura K. Grubb, Janet Lee, Makia E. Powers, Maria H. Rahmandar, Krishna K. Upadhya, Stephenie B. Wallace; The Impact of Racism on Child and Adolescent Health. Pediatrics August 2019; 144 (2): e20191765. 10.1542/peds.2019-1765
- Garg A, Wilkie T, LeBlanc A, Lyu R, Scornavacca T, Fowler J, Rhein L, Alper E. Prioritizing Child Health: Promoting Adherence to Well-Child Visits in an Urban, Safety-Net Health System During the COVID-19 Pandemic. Jt Comm J Qual Patient Saf. 2022 Apr;48(4):189-195. doi: 10.1016/j.jcjq.2022.01.008. Epub 2022 Jan 26. PMID: 35216919; PMCID: PMC8789396.
- Tom JO, Tseng C-W, Davis J, Solomon C, Zhou C, Mangione-Smith R. Missed well-child care visits, low continuity of care, and risk of ambulatory care-sensitive hospitalizations in young children. Arch Pediatr Adolesc Med. 2010;164(11):1052–1058.
- Evans EJ, Arbeit CA. What's the difference? Access to health insurance and care for immigrant children in the US. Int Migr. 2017;55(5):8–30.
- Institute of Medicine. 2003. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: The National Academies Press. https://doi.org/10.17226/10260
- Improving Health Equity: Build Infrastructure to Support Health Equity. Guidance for Health Care Organizations. Boston, Massachusetts: Institute for Healthcare Improvement; 2019. (Available at www.ihi.org)
- Chadha N, Lim B, Kane M, Rowland B. Institute for Healing and Justice in Medicine; 2020. https://belonging.berkeley.edu/race-medicine
- Ahmad K, Kabir E, Keramat SA, Khanam R (2021) Maternal health and health-related behaviours and their associations with child health: Evidence from an Australian birth cohort. PLOS ONE 16(9): e0257188. https://doi.org/10.1371/journal.pone.0257188
- REaL Data Collection Toolbox [Internet]. KHA; 2022 [cited 2023 Dec 18]. Available from: http://www.khaquality.com/Portals/[4]/Resources/HQIC_REaL%20Data_Collection_Toolbox.pdf
- Neal Halfon, Gregory D. Stevens, Kandyce Larson, Lynn M. Olson; Duration of a Well-Child Visit: Association With Content, Family-Centeredness, and Satisfaction. Pediatrics October 2011; 128 (4): 657–664. 10.1542/peds.2011-0586
- Leubner J, Wild S. Developing Standing Orders to Help Your Team Work to the Highest Level. Fam Pract Manag. 2018 May/Jun;25(3):13-16. PMID: 29989776.
- Standing Orders | Center for Excellence in Primary Care [Internet]. cepc.ucsf.edu. Available from: https://cepc.ucsf.edu/standing-orders
- Weitzman C, Wegner L, on behalf of the SECTION ON DEVELOPMENTAL AND BEHAVIORAL PEDIATRICS, COMMITTEE ON PSYCHOSOCIAL ASPECTS OF CHILD AND FAMILY HEALTH, COUNCIL ON EARLY CHILDHOOD, AND SOCIETY FOR DEVELOPMENTAL AND BEHAVIORAL PEDIATRICS. Promoting Optimal Development: Screening for Behavioral and Emotional Problems. PEDIATRICS Volume 135, number 2, February 2015. www.pediatrics.org/cgi/doi/10.1542/peds.2014-3716.
- Assessment of Social Emotional Development and Protective Factors [Internet]. www.aap.org. Available from: https://www.aap.org/en/patient-care/early-childhood/early-relational-health/assessment-of-social-emotional-development-and-protective-factors/
- Cree RA, Bitsko RH, Robinson LR, Holbrook JR, Danielson ML, Smith DS, Kaminski JW, Kenney MK, Peacock G. Health care, family, and community factors associated with mental, behavioral, and developmental disorders and poverty among children aged 2–8 years — United States, 2016. MMWR, 2018;67(5):1377-1383.
- Cree RA, Bitsko RH, Robinson LR, Holbrook JR, Danielson ML, Smith DS, Kaminski JW, Kenney MK, Peacock G. Health care, family, and community factors associated with mental, behavioral, and developmental disorders and poverty among children aged 2–8 years — United States, 2016. MMWR, 2018;67(5):1377-1383.
- phqscreeners [Internet]. www.phqscreeners.com. Available from: http://www.phqscreeners.com/
- Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults. American Journal of Preventive Medicine 1998; 14: 245–58.
- Dube SR, Felitti VJ, Dong M, Giles WH, Anda RF. The impact of adverse childhood experiences on health problems: evidence from four birth cohorts dating back to 1900. Preventive Medicine 2003; 37: 268–77.
- Kaiser Permanente Research Affiliates Evidence-based Practice Center. Screening and Interventions for Social Risk Factors: A Technical Brief to Support the U.S. Preventive Services Task Force [Internet]. 2021. Available from: https://www.uspreventiveservicestaskforce.org/uspstf/sites/default/files/inline-files/Social%20Risk%20Factors%20Tech%20Brief_Assembled%20for%20Web_Sep%202021_1.pdf
- Rojas L, Project S. Accountable Health Communities (AHC) Model Evaluation Second Evaluation Report RTI Point of Contact [Internet]. 2023 [cited 2024 Jan 16]. Available from: https://www.cms.gov/priorities/innovation/data-and-reports/2023/ahc-second-eval-rpt
- Sınger A, Coleman K, Mahmud A, Holden E, Stefanik-Guizlo K. Assessing the Feasibility of an Empathic Inquiry Approach to Social Needs Screening in 10 Federally Qualified Health Centers. The Permanente Journal. 2023 Dec 15;27(4):136–42.
- Byhoff E, Gottlieb LM. When There Is Value in Asking: An Argument for Social Risk Screening in Clinical Practice. Ann Intern Med. 2022;175(8):1181-1182. doi:10.7326/M22-0147
- Alegría, M., NeMoyer, A., Falgàs Bagué, I., Wang, Y., & Alvarez, K. (2018). Social Determinants of Mental Health: Where We Are and Where We Need to Go. Current psychiatry reports, 20(11), 95. https://doi.org/10.1007/s11920-018-0969-9
- Chavez, L. J., Tyson, D. P., Davenport, M. A., Kelleher, K. J., & Chisolm, D. J. (2023). Social Needs as a Risk Factor for Positive Postpartum Depression Screens in Pediatric Primary Care. Academic pediatrics, S1876-2859(23)00095-5. Advance online publication. https://doi.org/10.1016/j.acap.2023.03.007
- Califf, R. M., Wong, C., Doraiswamy, P. M., Hong, D. S., Miller, D. P., Mega, J. L., & Baseline Study Group (2022). Importance of Social Determinants in Screening for Depression. Journal of general internal medicine, 37(11), 2736–2743. https://doi.org/10.1007/s11606-021-06957-5
- National Academies of Sciences, Engineering, and Medicine; National Academy of Medicine; Committee on the Future of Nursing 2020–2030; Flaubert JL, Le Menestrel S, Williams DR, et al., editors. The Future of Nursing 2020-2030: Charting a Path to Achieve Health Equity. Washington (DC): National Academies Press (US); 2021 May 11. 2, Social Determinants of Health and Health Equity. Available from: https://www.ncbi.nlm.nih.gov/books/NBK573923/
- Butler, AB ED, Morgan, MD, MSc, MSHP AU, Kangovi, MD, MS S. Screening for Unmet Social Needs: Patient Engagement or Alienation? NEJM Catalyst [Internet]. 2020 Jul 20; Available from: https://catalyst.nejm.org/doi/full/10.1056/CAT.19.1037
- American College of Physicians. Closing-the-Loop. Baltimore: Transforming Clinical Practice Initiative--CMS; 2015.
- Black MM, Oberlander SE. Psychological Impact and Treatment of Neglect of Children. Child Abuse and Neglect. 2011;490–500.
- McLean SM, Booth A, Gee M, Salway S, Cobb M, Bhanbhro S, Nancarrow SA. Appointment reminder systems are effective but not optimal: results of a systematic review and evidence synthesis employing realist principles. Patient Prefer Adherence. 2016 Apr 4;10:479-99. doi: 10.2147/PPA.S93046. PMID: 27110102; PMCID: PMC4831598.
- Perron NJ, Dao MD, Kossovsky MP, Miserez V, Chuard C, Calmy A, Gaspoz JM. Reduction of missed appointments at an urban primary care clinic: a randomised controlled study. BMC Fam Pract. 2010 Oct 25;11:79. doi: 10.1186/1471-2296-11-79. PMID: 20973950; PMCID: PMC2984453.
- Viswanath, K., Bekalu, M., Dhawan, D. et al. Individual and social determinants of COVID-19 vaccine uptake. BMC Public Health 21, 818 (2021). https://doi.org/10.1186/s12889-021-10862-1
- Menschner C, Maul A. Key ingredients for successful trauma-informed care implementation [Internet]. 2016 Apr. Available from: https://www.samhsa.gov/sites/default/files/programs_campaigns/childrens_mental_health/atc-whitepaper-040616.pdf
- Trauma-Informed Care Implementation Resource Center. What Is Trauma? [Internet]. Trauma-Informed Care Implementation Resource Center. 2018. [accessed 2023 Aug 27]. Available from: https://www.traumainformedcare.chcs.org/what-is-trauma/
- Trauma-Informed Care [Internet]. [accessed 2023 Aug 17]. www.aap.org. Available from: https://www.aap.org/en/patient-care/trauma-informed-care/
- Centre for Health Care Strategies. What is Trauma-Informed Care? [Internet]. ]. Trauma-Informed Care Implementation Resource Center. 2021. [accessed 2023 Aug 17]. Available from: https://www.traumainformedcare.chcs.org/what-is-trauma-informed-care/3
- Trauma-Informed Care [Internet]. ]. [accessed 2023 Aug 17]. www.aap.org. Available from: https://www.aap.org/en/patient-care/trauma-informed-care/.
- Centre for Health Care Strategies. What is Trauma-Informed Care? [Internet]. Trauma-Informed Care Implementation Resource Center. 2021. Available from: https://www.traumainformedcare.chcs.org/what-is-trauma-informed-care/
- Survey on Racism, Discrimination and Health [Internet]. KFF. 2023. Available from: https://www.kff.org/racial-equity-and-health-policy/poll-finding/survey-on-racism-discrimination-and-health/
- Tong JKC, Akpek E, Naik A, Sharma M, Boateng D, Andy A, et al. Reporting of Discrimination by Health Care Consumers Through Online Consumer Reviews. JAMA Network Open. 2022 Feb 28;5(2):e220715.
- Trauma-Informed Care Implementation Resource Center. What Is Trauma? [Internet]. Trauma-Informed Care Implementation Resource Center. 2018. Available from: https://www.traumainformedcare.chcs.org/what-is-trauma/
- Takeshita J, Wang S, Loren AW, Mitra N, Shults J, Shin DB, et al. Association of Racial/Ethnic and Gender Concordance Between Patients and Physicians With Patient Experience Ratings. JAMA Network Open. 2020 Nov 9;3(11):e2024583.
- Jetty A, Jabbarpour Y, Pollack J, Huerto R, Woo S, Petterson S. Patient-Physician Racial Concordance Associated with Improved Healthcare Use and Lower Healthcare Expenditures in Minority Populations. Journal of Racial and Ethnic Health Disparities. 2021 Jan 5;
- Frakes MD, Gruber J. Racial Concordance and the Quality of Medical Care: Evidence from the Military [Internet]. National Bureau of Economic Research. 2022 [cited 2023 Oct 13]. Available from: https://www.nber.org/papers/w30767
- Trauma-Informed Care Implementation Resource Center. What Is Trauma? [Internet]. Trauma-Informed Care Implementation Resource Center. 2018. Available from: https://www.traumainformedcare.chcs.org/what-is-trauma/
- Schulman M, Menschner C. Laying the Groundwork for Trauma-Informed Care [Internet]. 2018. Available from: https://www.traumainformedcare.chcs.org/wp-content/uploads/Brief-Laying-the-Groundwork-for-TIC_11.10.20.pdf
- Patel, M.P., Schettini, P., O’Leary, C.P. et al. Closing the Referral Loop: an Analysis of Primary Care Referrals to Specialists in a Large Health System. J GEN INTERN MED 33, 715–721 (2018). https://doi.org/10.1007/s11606-018-4392-z
- American College of Physicians. Transforming Clinical Practice Initiative SAN Power Packs: Closing the Loop. Centers for Medicare & Medicaid Services; 2019. Available from: https://www.cms.gov/priorities/innovation/files/x/tcpi-san-pp-loop.pdf
- Reducing Care Fragmentation: A Toolkit for Coordinating Care [Internet]. The Center for Accelerating Care Transformation. The Commonwealth Fund; 2010. Available from: https://www.act-center.org/application/files/7016/3112/2157/Toolkit_Reducing_Care_Fragmentation.pdf
- James H. Duffee, Alan L. Mendelsohn, Alice A. Kuo, Lori A. Legano, Marian F. Earls, COUNCIL ON COMMUNITY PEDIATRICS, COUNCIL ON EARLY CHILDHOOD, COMMITTEE ON CHILD ABUSE AND NEGLECT, Lance A. Chilton, Patricia J. Flanagan, Kimberley J. Dilley, Andrea E. Green, J. Raul Gutierrez, Virginia A. Keane, Scott D. Krugman, Julie M. Linton, Carla D. McKelvey, Jacqueline L. Nelson, Emalee G. Flaherty, Amy R. Gavril, Sheila M. Idzerda, Antoinette “Toni” Laskey, John M. Leventhal, Jill M. Sells, Elaine Donoghue, Andrew Hashikawa, Terri McFadden, Georgina Peacock, Seth Scholer, Jennifer Takagishi, Douglas Vanderbilt, Patricia G. Williams; Early Childhood Home Visiting. Pediatrics September 2017; 140 (3): e20172150. 10.1542/peds.2017-2150
- Reviewing Evidence of Effectiveness [Internet]. 2020. Available from: https://www.acf.hhs.gov/sites/default/files/documents/opre/homvee_executive_summary_brief_2020%20%28certified%20for%20posting%29.pdf
- Casillas KL, Fauchier A, Derkash BT, Garrido EF. Implementation of evidence-based home visiting programs aimed at reducing child maltreatment: A meta-analytic review. Child Abuse & Neglect. 2016 Mar;53:64–80.
- AAP Updates Early Childhood Home Visiting Recommendations [Internet]. HealthyChildren.org. [cited 2024 Jan 16]. Available from: https://healthychildren.org/English/news/Pages/AAP-Updates-Early-Childhood-Home-Visiting-Recommendations.aspx
- AAP Updates Early Childhood Home Visiting Recommendations [Internet]. HealthyChildren.org. [cited 2024 Jan 16]. Available from: https://healthychildren.org/English/news/Pages/AAP-Updates-Early-Childhood-Home-Visiting-Recommendations.aspx
- James H. Duffee, Alan L. Mendelsohn, Alice A. Kuo, Lori A. Legano, Marian F. Earls, COUNCIL ON COMMUNITY PEDIATRICS, COUNCIL ON EARLY CHILDHOOD, COMMITTEE ON CHILD ABUSE AND NEGLECT, Lance A. Chilton, Patricia J. Flanagan, Kimberley J. Dilley, Andrea E. Green, J. Raul Gutierrez, Virginia A. Keane, Scott D. Krugman, Julie M. Linton, Carla D. McKelvey, Jacqueline L. Nelson, Emalee G. Flaherty, Amy R. Gavril, Sheila M. Idzerda, Antoinette “Toni” Laskey, John M. Leventhal, Jill M. Sells, Elaine Donoghue, Andrew Hashikawa, Terri McFadden, Georgina Peacock, Seth Scholer, Jennifer Takagishi, Douglas Vanderbilt, Patricia G. Williams; Early Childhood Home Visiting. Pediatrics September 2017; 140 (3): e20172150. 10.1542/peds.2017-2150
- Villas-Boas SB, Kaplan S, White JS, Hsia RY. Adolescent Total and Mental Health–Related Emergency Department Visits During the COVID-19 Pandemic. JAMA Netw Open. 2023;6(10):e2336463. doi:10.1001/jamanetworkopen.2023.36463
- Solmi, M., Radua, J., Olivola, M. et al. Age at onset of mental disorders worldwide: large-scale meta-analysis of 192 epidemiological studies. Mol Psychiatry 27, 281–295 (2022). https://doi.org/10.1038/s41380-021-01161-7
- Bergen, C., Bortolotti, L., Tallent, K., Broome, M., Larkin, M., Temple, R., Fadashe, C., Lee, C., Lim, M. C., & McCabe, R. (2022). Communication in youth mental health clinical encounters: Introducing the agential stance. Theory & Psychology, 32(5), 667-690. https://doi.org/10.1177/09593543221095079
- Fischer, J. A., Kelly, C. M., Kitchener, B. A., & Jorm, A. F. (2013). Development of Guidelines for Adults on How to Communicate With Adolescents About Mental Health Problems and Other Sensitive Topics: A Delphi Study. SAGE Open, 3(4). https://doi.org/10.1177/2158244013516769
- Sullivan, K, George, S. & Horowitz, K. (2021) Addressing National Workforce Shortages by Funding Child Psychiatry Access Programs. Pediatrics January 2021; 147 (1). https://e20194012. 10.1542/peds.2019-4012
- Pharmacy FAQs [Internet]. www.cdph.ca.gov. Available from: https://www.cdph.ca.gov/Programs/CID/DCDC/CAIR/Pages/CAIR-join-pharmacy-FAQs.aspx
- Intro [Internet]. Center for Advancing Dyadic Care in Pediatrics. Available from: https://dyadiccare.ucsf.edu/intro
- Racovites N. HealthySteps Evidence Summary [Internet]. HealthySteps. 2021. Available from: https://www.healthysteps.org/resource/healthysteps-outcomes-summary/
- Research [Internet]. Child-Parent Psychotherapy. Available from: https://childparentpsychotherapy.com/about/research/
- Weiner M, Perkins AJ, Callahan CM. Errors in completion of referrals among older urban adults in ambulatory care. J Eval Clin Pract. 2010;16(1):76-81. doi:10.1111/j.1365-2753.2008.01117.x
- Mehrotra A, Forrest CB, Lin CY. Dropping the baton: specialty referrals in the United States. Milbank Q. 2011;89(1):39–68. doi: 10.1111/j.1468-0009.2011.00619.x.
- Mehrotra A, Forrest CB, Lin CY. Dropping the baton: specialty referrals in the United States. Milbank Q. 2011;89(1):39–68. doi: 10.1111/j.1468-0009.2011.00619.x.
- National Committee for Quality Assurance. Patient-Centered Medical Home (PCMH) - NCQA [Internet]. NCQA. 2011. Available from: https://www.ncqa.org/programs/health-care-providers-practices/patient-centered-medical-home-pcmh/
- Cai C, Gaffney A, McGregor A, Woolhandler S, Himmelstein DU, McCormick D, et al. Racial and ethnic disparities in outpatient visit rates across 29 specialties. JAMA Internal Medicine. 2021 Nov 1;181(11):1525. doi:10.1001/jamainternmed.2021.3771