©️ 2024 Kaiser Foundation Health Plan, Inc.
This guide provides step-by-step guidance for improving population-based care for adults living with chronic conditions with the goal of supporting substantive cultural, technological and process changes. In particular, it focuses on increasing the number of patients who have controlled high blood pressure and comprehensive diabetes care.
This guide was designed as part of the Population Health Management Initiative (PHMI), a California collaboration of the Department of Health Care Services (DHCS), Kaiser Permanente and Community Health Centers. Much of the content is relevant and adaptable to primary care practices of all kinds working to improve the health of the populations they serve.
It is estimated that six in 10 U.S. adults are living with a chronic disease, and chronic diseases are the leading cause of death and disability in the United States[1]. The impact of chronic conditions and the rates of complications are higher in historically marginalized populations[2]. One of the most effective ways to manage chronic diseases and reduce health inequities is by applying a systematic, team-based care approach to wellness visits for chronic disease screening and to subsequent scheduled visits for management. Adopting standard procedures to identify and manage chronic conditions allows practices to provide high-quality, person-centered, culturally responsive care to patients, foster efficiency, and reduce clinician and staff burden. Systematic care that incorporates a person-centered approach to managing chronic conditions improves equity in care and patient outcomes by:
- Improving health and well-being among all patient populations.
- Recognizing and reducing potential barriers to care.
- Reducing burnout among clinicians and staff.
The work to ensure that patients have access to high-quality, person-centered diabetes and hypertension care is a continuous effort, and we still have much to learn. This “living” document uses existing evidence, bright spots and examples from the field to offer practical guidance on improving the effectiveness of your diabetes and hypertension management protocols while ensuring patient access to preventive care. While some of the guidance in this document is technical, much of the guide is focused on supporting practices in the substantive cultural, technological and process changes that lead to improved population-based care for adults with diabetes and/or hypertension. Virtually every activity in the guide will require some level of adaptation for your practice’s unique context. The Population Health Management Initiative (PHMI) will update this guide as we learn from and with practices.
We have organized the key activities in this guide into three categories:
- Foundational activities: Activities that all practices should implement as part of the activities to support the two core measures (Comprehensive Diabetes Care and Controlling High Blood Pressure) and the supplemental measure (Adults’ Access to Preventive and Ambulatory Health Services).
- Going deeper activities: More advanced activities that build off the foundational activities and that help ensure your practice can achieve equitable improvement in your patients’ management of chronic diseases, including diabetes and hypertension.
- On the horizon activities: Additional activities, including ideas worthy of testing that include the latest ideas and thinking on management of chronic diseases, including diabetes and hypertension.
Sequencing activities: We recommend that practices consider planning and attempting to implement the activities in the sequence provided in this guide. At the same time, we recognize that different practices may follow a different path toward prioritizing and implementing these activities. Furthermore, there is a lot of overlap between activities; many activities build off, or form the building blocks, of other activities.
Testing and implementing: For each activity, we provide guidance on how to plan, test and implement the activity along with links to other resources, Technology considerations and examples. Consider testing different versions of the action steps and roles on a small scale before fully implementing them at your practice.
Maintaining progress: For many activities, we also provide tips for periodically reviewing and making improvements to key workflows after initially implementing the change. Ongoing review and continual improvement are important for your practice to maintain your progress in population health management and to help you stay nimble in adapting to changing patient demographics, new clinical best practices, new payment policies, workforce changes and other changes at your practice.
If you implement the Foundational Activities in this guide, your practice should be able to achieve the following foundational competencies.
For chronic conditions, your practice will be able to consistently:
- Engage patients served by your practice to validate any of your proposed process improvements and to propose alternative methods to improve quality in your focus area.
- Analyze core quality measures to identify inequities and opportunities for improving A1c control and blood pressure among attributed patients.
- Implement chronic care management activities.
- Create an outreach protocol to reach and engage all attributed patients due for care.
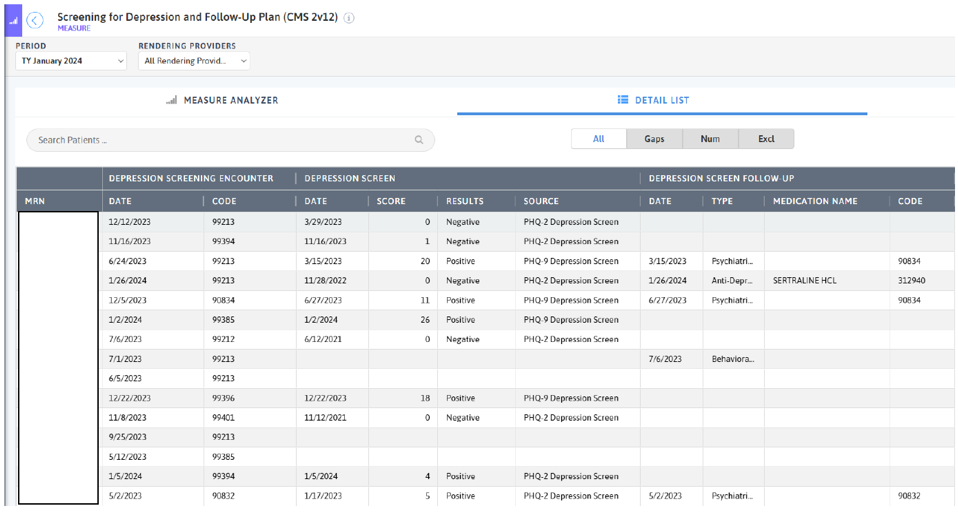
- Integrate behavioral health follow-up services as needed (e.g., for positive depression screens).
- Create a health-related social needs screening process that informs patients’ treatment plans.
- Assess current capabilities and develop a plan for ongoing improvement in data utilization, care team workflows and efficiency that includes sustainable health information technology (HIT) strategies and continuous staff training on technology.
This guide also includes sections on measurement, equity, social health, and behavioral health integration as well as an appendix with helpful tools and resources. We have included information about California Medi-Cal-covered benefits and services that were up-to-date at the time of publishing, but benefits and billing guidance change over time. Nothing in this guide should be considered formal guidance. Anyone using this guide should check with the appropriate authorities on benefits and billing guidance. This document will be refined based on continued learning on this topic; future updates may include additional activities, examples, resources and sections.
Working to improve the health of a population leverages everyone in a practice. Critical roles needed to engage in the work outlined in this guide and support practice change include:
- Quality improvement (QI) leadership, like a QI director, or additional team leads (i.e., clinical, front office, etc.) to support cultural changes.
- Coaches or practice facilitators who are partnered with teams to help identify areas for improvement and support change through change management strategies.
Putting the Key Activities in Context
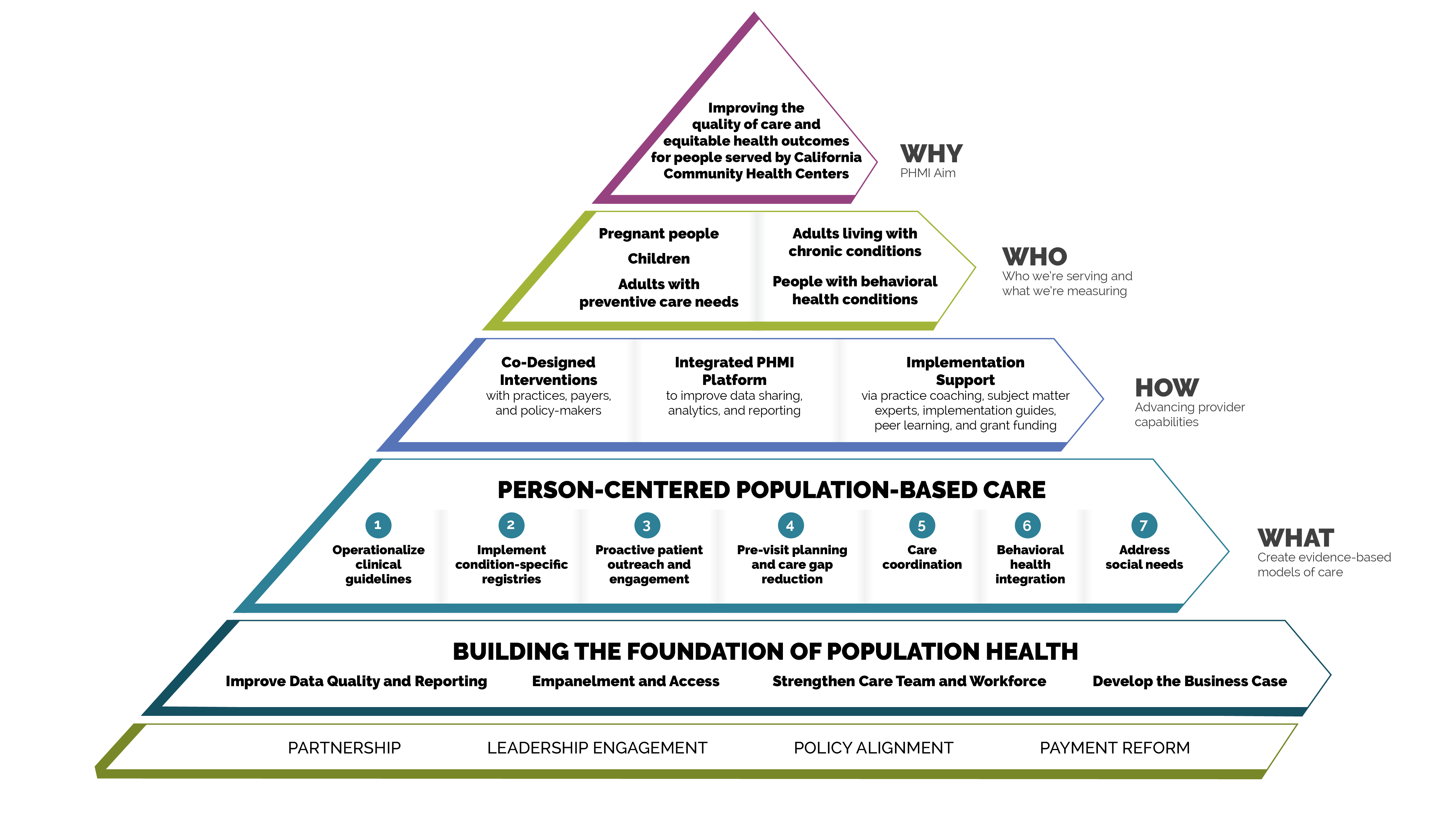
Person-centered population-based care
Each of the key activities advance one or more of the seven person-centered population-based care change concepts:
- Operationalize clinical guidelines.
- Implement condition-specific registries.
- Proactive patient outreach and engagement.
- Pre-visit planning and care gap reduction.
- Care coordination.
- Behavioral health integration.
- Address social needs.
FIGURE 1: PHMI IMPLEMENTATION MODEL
The measures covered in this guide consist of Healthcare Effective Data and Information Set (HEDIS) measures designated as core and supplemental measures by PHMI. These measures can be considered outcome measures because there is ample evidence that improved timely screening rates and follow-up care improves overall population health outcomes for depression. All measures use standard HEDIS definitions and are aligned with California Advancing and Innovating Medi-Ca (CalAIM) and Alternative Payment Methodology (APM 2.0). For information about these measures, reference the PHMI Data Quality and Reporting Guide
PHMI selected two core and one supplemental measures of focus for adult chronic condition management, though practices can track others that feel important and relevant. This guide provides detailed guidance to improve your practice’s results on the measures selected by PHMI.
Core HEDIS Measures for PHMI
|
PHMI Populations of Focus |
Measures |
|---|---|
Adults Living With Chronic Conditions |
Controlling High Blood Pressure
|
|
Comprehensive Diabetes Care
|
Supplemental HEDIS Measures for PHMI
|
PHMI Populations of Focus |
Measures |
|---|---|
All Adults |
Adults’ Access to Preventive and Ambulatory Health Services
|
The core and supplemental measures are part of a larger measurement strategy and learning system, as outlined in Appendix A: Sample Idealized System Diagram: Weaving Your Measurement Strategy and Learning System into Practice Operations. Key Activity 1: Convene a Multidisciplinary Implementation Team for Chronic Care Management outlines how your practice can develop a robust measurement system to support this work. In addition to quality assurance and monitoring, measures are also used during practice operations alongside other data for learning to:
- Guide the actions of the multidisciplinary implementation team as it uses a systematic approach to decreasing inequities and support implementing key activities across the practice.
- Support the care team’s efforts to advance population health and reduce care gaps through daily, weekly and monthly workflows, as well as continuously identify opportunities for improvement.
The PHMI Clinical Guidelines Advisory Group (CGAG) was established to create a standardized approach to review, adopt and promote established clinical guidelines in the PHMI cohort. For people with chronic health conditions, guidance includes controlling hypertension and comprehensive diabetes care. For more information please see the PHMI Clinical Practice Guidelines for Key Medi-Cal Populations of Focus.
FIGURE 2: CLINICAL GUIDELINES: CONTROLLING HIGH BLOOD PRESSURE
Guideline source |
Kaiser Permanente National Guideline Program (October 2021) |
PHMI measure |
Controlling High Blood Pressure |
Guideline language |
Blood pressure (BP) screening: Screen adults 18 years and older for high blood pressure.
Hypertension definition:
Treatment initiation:
Treatment target:
For corresponding SBP/DBP values, corresponding SBP/DBP values, initial pharmacotherapy, and follow up recommendations see the PHMI Clinical Practice Guidelines for Key Medi-Cal Populations of Focus.
|
FIGURE 3: CLINICAL GUIDELINES: COMPREHENSIVE DIABETES CARE
Guideline source |
USPSTF, American Diabetes Association (ADA) and Kaiser Permanente National Guideline Program (July 2023) |
PHMI measure |
Comprehensive Diabetes Care |
Guideline language |
Screening (USPSTF): Asymptomatic adults aged 35 to 70 years who have overweight or obesity. Diagnosis (ADA):
OR
OR
OR
For the full ADA guidelines, see Diabetes Care 2. Classification of Diabetes: Standards of Care in Diabetes - 2023 For glycemic control and treatment targets, and guidelines for self-monitoring, see the PHMI Clinical Practice Guidelines for Key Medi-Cal Populations of Focus.
|
Many key activities in this guide include considerations for utilizing the intervention to improve equitable health outcomes and reduce the effects of racism, bias and discrimination. Key Activity 4: Use a Systematic Approach to Decrease Inequities Within the Population of Focus describes key action steps for how to make an intentional and explicit effort to identify inequities, understand root causes and reduce those inequities.
This guide also offers resources for going deeper into organizational and ecosystem-level work to advance equitable outcomes through strengthening a culture of equity. More information about this approach can be found in the PHMI Equity Framework and Approach and Key Activity 23: Strengthen a Culture of Equity.
Integrated behavioral health supports are important for adults as effective management of chronic conditions is likely to boost health outcomes and enhance patients' quality of life.
One foundational change is to ensure that the care team includes behavioral health staff as core members of the team; this is covered in detail in the PHMI Care Teams and Workforce Guide.
We also offer the resource Pre-Visit Planning: Leveraging the Team to Identify and Address Gaps in Care includes recommended behavioral health screenings.
Throughout the key activities in this guide, we have incorporated considerations for providing trauma-informed care and have included a resource for Trauma-Informed Population Health Management. For additional information, please see the PHMI People with Behavioral Health Conditions Guide. The Agency for Healthcare Research and Quality (AHRQ) also provides resources on integrating health equity and behavioral health.
The Agency for Healthcare Research and Quality (AHRQ) recommends that in order to advance health equity, practices and health systems must consider and address health-related social needs that impact their patients.[3]
For many key activities in this guide, we have highlighted considerations related to social needs at an individual or population level, such as expanding clinic hours and coordinating care. Key Activity 17: Use Social Needs Screening to Inform Patient Treatment Plans assists to develop a process to screen for social needs, which can help practices better understand and support patient- and population-level needs. Practices can help patients make connections to resources in the community to address issues such as nutrition and legal and health education needs. For Medi-Cal patients and families with high levels of social need, such as those experiencing homelessness, referrals to Enhanced Care Management (ECM) and Community Supports programs are available; see Key Activity 21: Provide Care Management for more.
To go deeper in this area, practices can further develop their referral relationships and pathways (Key Activity 22: Continue to Develop Referral Relationships and Pathways Networks) for common social needs and strengthen community partnerships (Key Activity 20: Strengthen Community Partnerships) to build upon the strengths, infrastructure, and resources available in the community. More information about this dual patient- and population-level approach is available in the PHMI Social Health Framework and Approach.
Our theory of change is that if practices implement the activities contained in this guide, it will lead to improved health and well-being outcomes among patients with chronic conditions served by these practices. See Appendix B: Theory of Change for a suggested driver diagram.
Foundational Key Activities
These are the core activities that all practices must implement as part of the activities to support the two core measures (Comprehensive Diabetes Care and Controlling High Blood Pressure) and the supplemental measure (Adults’ Access to Preventive and Ambulatory Health Services).
KEY ACTIVITY #1:
Convene a Multidisciplinary Implementation Team for Chronic Care Management
This key activity involves all seven elements of person-centered population-based care: : operationalize clinical guidelines; implement condition-specific registries; proactive patient outreach and engagement; pre-visit planning and care gap reduction; care coordination; behavioral health integration; address social needs.
Overview
This activity provides guidance for senior leaders to identify the right individuals within your practice who will be responsible for planning and implementing the key activities in this guide and overseeing related quality improvement and equity efforts, as outlined in Appendix A: Sample Idealized System Diagram: Weaving Measurement and Learning Into Practice Operations. This section also provides guidance on how to support and sustain this team to foster success.
The implementation team members are a diverse group of individuals who are champions for advancing this work. Improving your practice’s key outcomes for each population of focus and reducing equity gaps require the aligned efforts of all care teams and nearly all functional areas of the practice, not just those working directly with patients.
This team is responsible for ensuring that all foundational key activities in this guide, including those related to screening for social needs, are implemented. When identifying potential members of this multidisciplinary implementation team, the practice should identify a diverse group of staff who are reflective of various job functions within the practice, the local community and, by extension, the lived experience of patients. In addition to implementing Key Activity 4: Use a Systematic Approach to Decrease Inequities Within the Population of Focus, the team should apply an equity lens to every step outlined in this guide to help ensure that any improvements are equitably spread among the patient population. To achieve optimal functioning and impact, all members of this diverse multidisciplinary team should have their perspectives proactively included.
Relevant HIT capabilities to support this activity include care guidelines, registries, clinical decision support, care dashboards and reports, quality reports, outreach and engagement, and care management/care coordination (see Appendix E: Guidance on Technological Interventions). To enable team coordination, thought must be given to how access to relevant technology and how data capture can be distributed, consistent and integrated into workflows, and how data is accessible across team members. Where possible, it is desirable to avoid duplication of data entry, siloing of information in standalone applications and databases, and the need to work in multiple applications that require separate login.
Action steps and roles
1. Convene a time-limited group of practice leaders.
Suggested team member(s) responsible: chief medical officer (or equivalent), office manager or QI coordinator.
Start with a small group of leaders from your practice (some of whom will be on the implementation team) who can help refine the “charge” or scope of work of the implementation team and both identify and engage the people/roles that will be required to implement the scope of work of the team.
2. Develop a preliminary scope of work or charge outlining the responsibilities of the implementation team.
Suggested team member(s) responsible: time-limited group of practice leaders.
This scope or charge includes but may not be limited to enabling, aligning, leveraging and supporting the planning and implementation of all foundational activities in this implementation guide so that the practice meets the foundational competencies for chronic conditions. This should include a tentative timeline, core activities, and key roles and responsibilities.
However, there may be further foundation-building work needed at your practice in order to succeed at the above key activities. The Population Health Management Capabilities Assessment Tool (PhmCAT) is a multidomain assessment that is used to understand current population health management capabilities of primary care practices. This self-administered tool can help your practice identify opportunities and priorities for improvement.
If your practice does not score highly in the domains of leadership and culture, the business case for population health management, technology and data infrastructure, or empanelment and access, consider implementing the activities listed in the four guides on Building the Foundation before or in parallel to working on key activities related to management of chronic conditions.
3. Identify leadership and key actors for the implementation team.
Suggested team member(s) responsible: time-limited group of practice leaders.
The multidisciplinary implementation team should include those empowered to make changes in workflows, policies and staff assignments. They should be respected influencers in the organization (early adopters), who can also guide the change management process. They should include those with expertise in partnering with patients with diabetes and hypertension management.
- Appoint a “champion” or lead person (e.g., chronic conditions care coordinator or diabetes care coordinator) to oversee the implementation and coordination of the team.
- Identify key staff who will be the core members of the implementation team. These people will likely include one or more panel managers, clinicians, nurses, administrators, data analysts, social workers, community health workers, and other community outreach staff, information technology (IT)/electronic health record (EHR)-related personnel, and human resources personnel.
- For the chronic conditions multidisciplinary team, it is important to include members of the clinical team, patient support team, outreach team, social support team and EHR/data team. This could include a core team and an expanded team. Potential members include:
- Adult/family primary care clinicians (medical doctor, doctor of osteopathic medicine, advanced practice registered nurse, physician assistant).
- Endocrinologist.
- Cardiologist.
- Registered dietician.
- Certified diabetes educator.
- Nurse.
- Medical assistant (MA) or licensed vocational nurse (LVN).
- Social worker.
- Care coordinator.
- Community health worker.
- Pharmacist.
- A member of the IT or EHR team (as part of the expanded team).
- QI lead.
- Billing manager or similar (as part of the expanded team).
- A frontline staff member who interfaces with patients by phone and at check-in.
- Invite identified people to become part of the implementation team and ensure that they have appropriately designated time for participation.
- Teams should engage representation from IT to support the work of pulling data from the EHR and embedding updated data into tracking and evaluation.
4. Launch the implementation team and set it up for success.
Suggested team member(s) responsible: clinical coordinator or chief operating officer or chief medical officer.
This work includes:
- Ensuring that the team understands its charge or scope of work by developing a Multidisciplinary Implementation Team Charter Template, that outlines this work. Groups should work with each other to establish rapport and psychological safety as they develop team norms, which help teams to work together effectively.
- Defining roles and responsibilities, including the anticipated commitment (in hours) on a monthly basis.
- Establishing a meeting structure, file structure and communications structure to support effective, efficient work.
- Dedicating time and effort to forming, storming, norming and performing as a team. The Team Communication and Working Styles Template is one tool that team members can complete and share with other teammates to accelerate this process.
- Understanding baseline data related to outcomes of interest (e.g., hypertension control rates, hemoglobin A1c control rates), along with data related to known and perceived barriers to these outcomes.
- Prioritizing elements within the scope of work, informed by baseline data and identified population needs.
5. Develop a simple yet robust measurement strategy and learning system to guide your improvement efforts.
Suggested team member(s) responsible: implementation team.
A learning system enables a group of people to come together to share and learn about a particular topic, to build knowledge, and to speed up improved outcomes. A measurement strategy and learning system:
- Contains a balanced set of measures looking at outcomes, processes and possibly unintended secondary effects (e.g., increased cycle time and impact on team well-being).
- Incorporates the patient perspective and the perspective of staff (front desk and others), care team members, providers and management.
- Allows the team to determine if the process or system has improved, stayed the same or gotten worse.
- Helps guide improvement efforts and informs practice operations. See Appendix A: Sample Idealized System Diagram: Weaving Measurement and Learning Into Practice Operations for a sample system diagram of how your measurement strategy can be used to support practice operations.
Your practice should track the core and supplemental measures for hypertension control, comprehensive diabetes management and preventive ambulatory care visits. These can be considered outcome measures because there is ample evidence that improved care and management of chronic diseases will improve overall population health outcomes for effective chronic disease management.
In addition to the core and supplemental measures, practices should track process measures and balancing measures. Appendix C: Developing a Robust Measurement Strategy describes and defines the key milestones in the development of a robust measurement strategy, including definitions for each of these terms.
Suggested process measures:
- The percentage of patients 18 to 75 years of age with diabetes (type 1 and type 2) who receive a hemoglobin A1c test during the measurement year (NQF 0057).
- Percentage of patients ages 18 or older who are screened for high blood pressure and, if elevated or hypertensive, have a follow-up plan documented (CMS22v12).
- Percentage of adults who respond to a reminder to get scheduled for their visit.
- Percentage of adults who are due for a preventive/ambulatory visit that the practice reaches out to in order to schedule them if they are not already scheduled.
Suggested balancing measures: - One or more measures related to patient satisfaction.
- One or more measures related to staff satisfaction.
Practices can also look at other metrics to understand the progress of specific improvement initiatives over time. This may include:
- Progress on the Population Health Management Capabilities Assessment Tool (PhmCAT).
- Progress towards foundational competencies listed in this implementation guide. For example: “Yes or no: Did your practice achieve the foundational competency “Screen for Chronic Conditions?”
- Any other care gaps, clinical guidelines or measures your practice feels are important to prioritize.
Applying an equity lens
Your practice is likely achieving better outcomes with some patients than others. To understand these inequities, your practice should stratify your data based on race, ethnicity and language (REAL); sexual orientation and gender identity (SOGI); and other patient characteristics (e.g., social needs, etc.). See more in Key Activity 4: Use a Systematic Approach to Decrease Inequities within the Population of Focus. The ability to segment data in such a manner can lead to profound insights about structural challenges that drive some of the health outcomes. The Advancing Equity Through Data Quality and Reporting section of the PHMI Data Quality and Reporting Guide provides more guidance on this.
Putting it all together
We recommend that your practice record your measurement strategy in one place. This Measurement Strategy Tracker contains all the fields we believe are most useful; it can be customized to meet your practice’s needs.
6. Plan and hold regularly scheduled meetings of the implementation team.
Suggested team member(s) responsible: team lead or clinical coordinator or other individual tasked with coordinating the work of the team.
- Hold time on team members' calendars for standing meetings. Consider biweekly (twice monthly) meetings to start with. The frequency, duration and focus of these meetings may change as you consider additional populations or subpopulations and additional sites or locations, and as the nature of the work changes.
- Having a clinical perspective is an important aspect of this work. Consider models that minimize overall impact to patients’ ability to access care (i.e., having meetings before working hours or during lunch times; having providers attend crucial, rather than all, meetings; scheduling during providers’ administrative time).
- Develop a system to efficiently report on all workstreams and track follow-up items. The Action Plan Template is one tool that can be used to focus your team around the foundational competencies and define responsibility for actions steps to be taken for each project your team has prioritized to work on.
7. Make adjustments based on data from the team’s measurement strategy and feedback loops.
Suggested team member(s) responsible: multidisciplinary team.
- Review data and feedback at least monthly and adapt efforts as needed. Adaptation could include any or all of the following:
- Amending the scope of work.
- Modifying meetings or meeting structures.
- Changing the team composition (adding or removing members).
- Refining activities to better meet the needs of patients and staff, improve outcomes, or reduce inequities.
- Modifying the measurement strategy and/or feedback loops to better understand what is (and is not) happening.
- On an annual basis, the team’s charter and core membership should be reviewed. As the goals of the implementation team are met, the team could disband, meet less frequently (e.g., twice per year) or fold this meeting into a similar standing meeting that occurs separately.
Resources
Health Center Quality Measurement Systems Toolkit
The Health Alliance of Northern California created a summary crosswalk of measurement sets that provides an overview of alignment between measurement systems. It includes in-depth information on each Uniform Data System (UDS) or Quality Incentive Pool (QIP) clinical measure for diabetes care and hypertension, which is contained in a spreadsheet.
The document also shares suggested clinical interventions and community interventions for controlling diabetes and high blood pressure in rural northern California.
Evidence base for this activity
Pandhi N, Kraft S, Berkson S, Davis S, Kamnetz S, Koslov S, Trowbridge E, Caplan W. Developing primary care teams prepared to improve quality: a mixed-methods evaluation and lessons learned from implementing a microsystems approach. BMC Health Serv Res. 2018 Nov 9;18(1):847. doi: 10.1186/s12913-018-3650-4. PMID: 30413205; PMCID: PMC6230270.
KEY ACTIVITY #2:
Update or Implement Clinical Practice Guidelines
This key activity involves all seven elements of person-centered population-based care: operationalize clinical guidelines; pre-visit planning and care gap reduction; behavioral health integration.
Overview
Clinical practice guidelines are established standards of care that provide evidence-based recommendations for the diagnosis, treatment and management of various health conditions. They are established through a systematic review of evidence-based practice from a variety of sources, often from experts in the field. By following these guidelines, healthcare clinicians can ensure that patients receive high-quality care that is supported by current evidence-based practice. Clinical practice guidelines also help standardize care across different healthcare settings, which can improve patient outcomes, reduce healthcare costs and improve health equity.[4] Having guidelines is especially important for hypertension and diabetes management due to the complexity of ongoing management of these conditions.
Clinical practice guideline implementation is important because:
- They ensure that there are minimum standards of care within the practice.
- Care inequities can be reduced by providing universal standards.
- Guidelines allow for the development of other standard processes (i.e., standing orders), which help to reduce clinician burden. See Key Activity 9: Develop and Implement Standing Orders for more information.
- They facilitate a team-based model of care, which can be streamlined with standardized practices.
Clinical practice guidelines help promote equity by providing evidence-based recommendations for effective management of diabetes and hypertension. This ensures that care is standardized across the practice. While implementing clinical practice guidelines does not directly address social needs, enabling supportive care team members other than the primary care clinician to initiate care provides the opportunity to assess and to meet patients’ social needs.
Relevant HIT capabilities to support this activity include care guidelines, registries, clinical decision support, care dashboards and reports, quality reports, outreach and engagement, and care management/care coordination (see Appendix E: Guidance on Technological Interventions). Reports should have the capacity to filter by clinician, location and care team (where applicable).
Access to outside data may be a consideration or requirement (e.g., California Immunization Registry/immunization registry data and data from other practices) as services received outside the health center may be an important part of screening and follow-up. Ideally, this is accomplished by real-time data exchange, but where not possible, it may require manual entry. This may need to include not only the EHR but care coordination/population health management applications or freestanding referral registries. While claims data may be helpful in this regard, lag time may impact its usefulness. Patient-facing applications should be strongly considered to promote patient activation by helping ensure that patients are informed and appreciative of the nature and importance of recommended care. See Key Activity 24: Develop System to Provide Remote Monitoring for additional information.
Action steps and roles
1. Review the current, most up-to-date clinical guidelines and update appropriately.
Suggested team member(s) responsible: medical director (or equivalent) and quality improvement lead.
See the section titled Clinical Practice Guidelines earlier in this guide. Ensure your practice is using the latest guidelines.
In addition to those guidelines, you can review the following resources:
- ADA diabetes care recommendations (2023 standards).
- 2017 American College of Cardiology (ACC)/American Heart Association (AHA)/American Academy of Physician Assistants/Association of Black Cardiologists/American College of Preventive Medicine/American Geriatrics Society/American Pharmacists Association/American Society of Hypertension/American Society for Preventive Cardiology/National Medical Association/Preventive Cardiovascular Nurses Association Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults.
PHMI Clinical Practice Guidelines.
- Kaiser Permanente Adult Blood Pressure Clinical Practice Guidelines.
- Kaiser Permanente Type 2 Diabetes Screening and Treatment Guideline.
2. Develop standard methods of updating clinic staff on changes within key guidelines.
Suggested team member(s) responsible: medical director (or equivalent) and quality improvement lead.
These updates could be provided during a set meeting time, via email communication, via video update, etc.
3. Ensure access to evidence-based clinical decision support systems.
Suggested team member(s) responsible: administration and medical director (or equivalent).
Clinical decision support provides staff with information that is relevant to the care situation at appropriate times to enhance health and healthcare.[5] This provides easy access to support such as clinical practice guidelines and medication alerts. These are sometimes integrated into the Electronic Health Record (EHR).
4. Regularly evaluate and support the infrastructure of patient care teams to ensure adequate redundancy and staffing.
Suggested team member(s) responsible: administration, medical director (or equivalent) and nursing director (or equivalent).
Part of developing the infrastructure for care teams to properly integrate clinical guidelines is providing adequate equipment for staff. This includes providing validated, automated monitors and adequate supplies of all blood pressure cuff sizes to each care team. Point-of-care A1c tests are another aspect of infrastructure that can be considered. Staff should also be trained upon hire, and annually thereafter, on proper blood pressure measurement procedures. This ensures that all staff are trained and available to utilize equipment. Staff should also be trained on other aspects of workflows, such as rooming, pre-visit planning (PVP), huddles, etc., in order to ensure that care does not suffer if a crucial staff member is unavailable on a certain day.
Additionally, practices should regularly evaluate clinic workflows and clinician panels to ensure that the number of staff that are allocated to each area is adequate. See the PHMI Empanelment Guide and Care Teams & Workforce Guide for more information.
5. Develop guidelines that reflect a spectrum of treatment needs.
Suggested team member(s) responsible: administration, medical director (or equivalent) and nursing director (or equivalent).
Guidelines should provide evidence-based recommendations for intensification of treatment, which emphasizes performance feedback. This can be for initiatives such as following up on lab results or utilizing guidelines for medication measures. Additionally, clinicians should be educated regarding how to best address common side effects and lab abnormalities.
Implementation tips
Facilitate opportunities to share/collaborate with behavioral health colleagues about the clinical practice guidelines for chronic diseases management. Much of chronic disease management requires patients to engage in behavior change. Behavioral health colleagues bring skills and strategies that best support patients in making and sustaining the changes necessary to initiate and maintain behavior change
Resources
KEY ACTIVITY #3:
Use Care Gap Reports or Registries to Identify All Patients Eligible and Due for Care
This key activity involves all seven elements of person-centered population-based care: ooperationalize clinical guidelines; implement condition-specific registries; address social needs.
Overview
This foundational activity provides detailed guidance on how to reliably and efficiently develop and use a regularly updated list of patients eligible for recommended or standard screenings or interventions (e.g., blood pressure, lab work, etc.) through a care gap report or registry. Please note that this activity focuses on diabetes and hypertension; many other preventive and maintenance services are needed to provide comprehensive preventive care (see the Pre-Visit Planning: Leveraging the Team to Identify and Address Gaps in Care resource for a more complete list).
Care gaps are gaps between the recommended care that a patient should receive according to clinical guidelines and the care a patient actually receives.
Most EHRs already have a module that identifies what services are due for each patient (see examples below).
FIGURE 4: EXAMPLE OF A CARE GAP REPORT FOR AN INDIVIDUAL PATIENT (BLOOD PRESSURE)
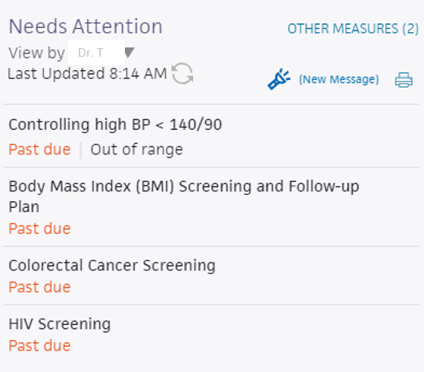
FIGURE 5: EXAMPLE OF A CARE GAP REPORT FOR AN INDIVIDUAL PATIENT (HEMOGLOBIN A1C)
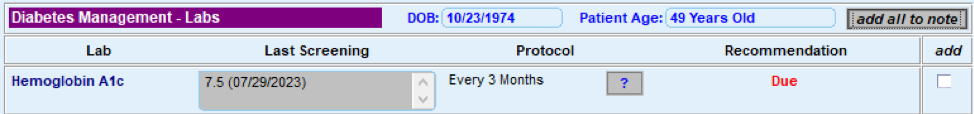
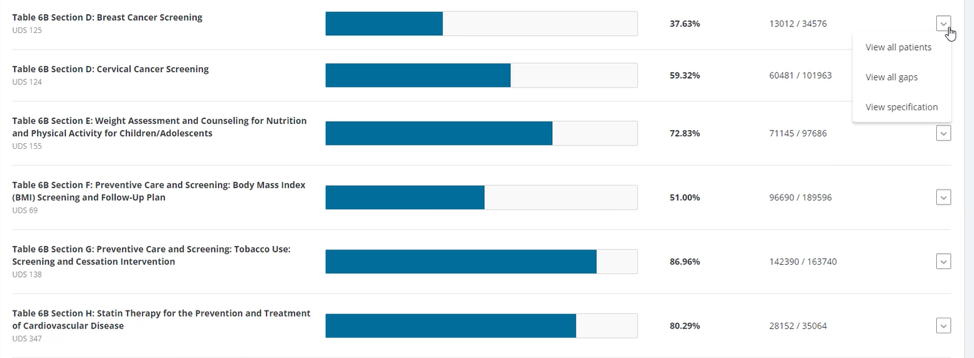
FIGURE 6: EXAMPLE OF A CARE GAP REPORT SUMMARY AT A POPULATION LEVEL
A registry is a list of patients with a specific characteristic that can be used for tracking aspects of screening, treatment or outcomes. At minimum, a registry should include:
- Medical record number. (MRN)
- Patient name.
- Date of birth.
- Contact information.
- Race, ethnicity, and preferred Language (REAL).
- SOGI data.
- Clinical data points that are being checked for care gaps.
An example chronic care registry report from the American Medical Association highlights clinical data points that may be important to consider when building a chronic care registry.
Care gap reports are reports embedded in EHRs that use the registry concept to identify patients assigned to your care team or in some other cohort, who have a specified care gap.
Rather than put the responsibility on an individual care team member for searching through charts or remembering which patients need further preventive care or follow-up, this key activity provides guidance on how the practice can efficiently leverage EHRs to identify patient care gaps.
Care gap reports are essential for practices to understand and continually improve consistency and reliability for meeting guidelines for preventive care and chronic disease management. At the care team level, care gap reports focus on gaps for patients assigned to your care team and help your team understand which patients you are responsible for. They can be used to:
- Support improvements to the pre-visit planning (PVP) process, standing orders and other routine clinical workflows designed to systematically identify and address gaps in recommended care.
- Prioritize patients to whom care teams should provide proactive outreach and reminders for engaging in care.
- Support quality improvement efforts with an equity lens.
- Improve your performance on key measures by ensuring you are able to do follow-up assessments/screenings for patients overdue for services (such as labs, ophthalmology checks for people with diabetes, foot screening for neuropathy, etc.).
Actively identifying and acting on care gaps ensures all eligible patients assigned to your practice receive timely screenings for chronic disease and other preventive services. This reduces the burden on the healthcare system by preventing more severe health issues in the future. Furthermore, this reduces missed or delayed diagnoses. For adults with chronic conditions, care gap reports can identify patients who are due for regular or infrequent required screenings in accordance with clinical care guidelines, including guidelines that may be established by specific payors. They also can identify opportunities for screening and improvement for controlling said chronic conditions.
Many practice patients experience barriers to accessing care due to structural and historical racism, homophobia, xenophobia and other biases that have historically disadvantaged individuals and groups from receiving equitable services. Defining clear criteria and gaps for patients due for specific screenings or preventive services helps to illuminate groups that have not had equitable access. It also combats biases by standardizing expectations for who is due for what care, providing a starting point for ensuring reliable and equitable access.
Staff can identify potential barriers and challenges for patients accessing and engaging in care by using enhanced care gap reports to filter and display the data alongside demographic information, social needs, behavioral health needs and communication preferences. This information can be used to promote a person-centered approach when designing the care plan, promoting self-care and conducting other patient engagement activities, such as conducting outreach in the patients’ preferred language.
Furthermore, care gap reports that segment the data into cohorts based on demographic and other personal information may help the team identify inequities in care, access and outcomes, which can inform improvement efforts. For example, therapeutic intensity requirements may differ by population. It is also important to gain input from the patient to ensure that their needs are being met.
Care gap reports can be used during pre-visit planning (PVP) to identify people for whom social needs screening has not yet been completed. This creates an opportunity to identify unmet social health needs and to connect patients with resources that address their social needs. See Key Activity 10: Develop or Refine and Implement a Pre-Visit Planning Process for more information.
Many EHRs already have a module that identifies what services are due for each patient whereas others do not. Where this functionality is available, it may not be configurable to align with the health center’s specific protocol or be able to incorporate outside data. Other options for developing registries include supplemental applications, population health platforms and freestanding customized databases that draw data from the EHR and other sources.
Care gap reports may be embedded in EHRs or made available through other technology channels (See Appendix E: Guidance on Technological Interventions.)
They are useful both at the individual patient level and aggregated to identify groups of patients to facilitate population-level management through registries.
A registry can be thought of as simply a list of patients sharing specific characteristics that can be used for tracking and management. Both care gap reports and registries should have the capacity to segment patients by age, gender, race/ethnicity and language.
Other relevant HIT capabilities to support/relate to this activity include care guidelines, care dashboards and reports, quality reports, outreach and engagement, and care management/care coordination.
(See Appendix E: Guidance on Technological Interventions.)
Access to outside data (e.g., California Immunization Registry/immunization data and data from other practices) may be a consideration or requirement as services received outside the practice may be part of compliance. While claims data may be helpful in this regard, lag time may impact its usefulness. Patient-facing applications should be strongly considered to ensure patients are informed and appreciative of the nature and importance of recommended care. In California, many healthcare organizations are required or have chosen to participate in the California Data Exchange Framework (DxF), which can facilitate data sharing between clinics, managed care plans (MCPs) and other partners.
Action steps and roles
1. Plan the care gap report.
Suggested team member(s) responsible: panel manager or data analyst. If it is not clear how the report can be produced, this step may involve one or more people from the practice who work on the EHR and possibly the EHR vendor.
As a team, decide what screenings or treatment guidelines are appropriate for your population of focus and prioritize the most important care gaps to run reports on. Start with the core and supplemental measures and any process measures your practice is tracking, then consider if there are any other gaps, clinical guidelines or measures your practice feels important to prioritize.
Identify the inclusion criteria for each report, such as age, any exclusion criteria and factors that make someone high risk.
Care gap reports should at minimum include monitoring for control of the following:
Among persons 18 to 75 years old with diabetes:
- No hemoglobin A1c test within the past six months.
- A1c >9% without a follow-up.
- Missing a urine albumin-to-creatinine ratio test in the past 12 months.
- Missing diabetic eye exam in the past 12 months.
- Missing diabetic foot exam in the past 12 months.
Among persons 18 to 85 years old with hypertension:
- No documentation of blood pressure in the past 12 months (or ever).
- If the last blood pressure was uncontrolled.
- If there was no documented follow-up if the blood pressure was elevated.
Care gap reports should also be developed to flag persons not meeting HEDIS measure thresholds who require follow-up because of positive screening results or lab values outside recommended limits. Many such reports may already be part of your clinic’s EHR.
2. Build the report.
Suggested team member(s) responsible: data analyst.
Determine whether the EHR has an existing report or one that can be modified to fit the inclusion criteria. You should talk to staff who are familiar with the electronic record; in some cases, it may be necessary to consult with the EHR vendor to confirm this information and how to run the report.
The care gap format should include:
- Criteria for inclusion in the report.
- The overall compliance rate for the care gap being measured.
- All patients eligible for the screening or intervention and their addresses and phone numbers.
- The last date the test was performed, if known or if applicable; the previous results; and the type of test used.
- Preferred method of communication (e.g., phone, email, text).
Reports should be able to display and/or disaggregate the data based on:
- Race, ethnicity, and language (REAL) as well as sexual orientation and gender identity (SOGI).
- Any known social or behavioral needs.
- Communication preferences or other preferences that would inform the screening modalities offered or treatment preferences, such as documented declination of prior screenings or medications.
- Data on any other characteristic, including insurance data, that could pose a barrier to completing screening or influence treatment choices.
Report developers should also work to allow for evaluation of data on a clinician panel, clinic unit, whole clinic and health system level.
3. Standardize the data format.
Suggested team member(s) responsible: panel manager or data analyst.
Standardizing the data format and where it is entered is critical to ensuring accuracy in the resultant report. Once you know that a report can be produced, understand the specific data elements that are needed to produce the reports.
Document how each data element must be entered into the EHR in order to populate the fields needed for reporting. In some cases, data on completion of screening must be entered by hand (e.g., when the test is performed by a lab that does not communicate with the legacy EHR). Doing this will require a decision on the part of the practice as a whole and may require staff training and reinforcement on an ongoing basis. Where issues or apparent confusion is identified, regular discussion at team huddles or staff meetings will help in maintaining a standard approach.
Tip: Assign responsibility for the initial review of the reports to confirm data integrity.
4. Develop workflows to improve patient screening and preventive care completion rates.
Suggested team member(s) responsible: panel manager, care team and EHR specialist (or equivalent).
At the patient level, ensure that the care gap report can be used for or linked with reminders or alerts for clinicians, as well as for reminders to patients who need to come in to the clinic for screening or follow-up. As an example, a care gap report could alert the care team that a diabetic patient is in need of a foot check in accordance with the guidelines. For example, a standing order could trigger the MA who is trained in foot screening to do the foot check at the time of rooming. The workflow in Figure 7 applies to both chronic and preventive screening.
FIGURE 7: SCHEDULED PREVENTIVE CARE VISIT WORKFLOW
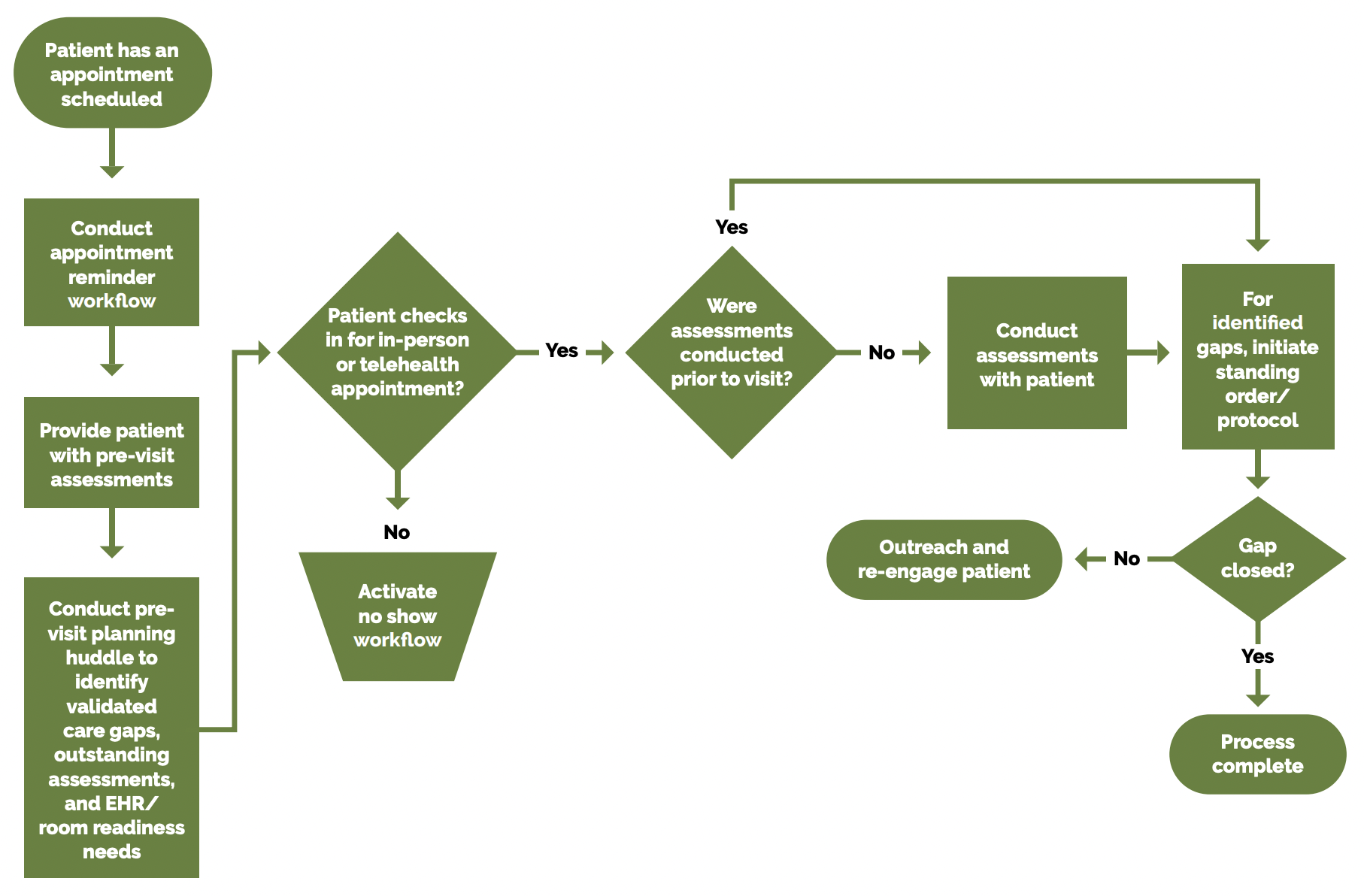
See the PHMI Care Teams and Workforce Guide Resource 6: Workflow Examples for more information.
Depending on communication preferences that have been expressed by patients, the patient care gap report may be exported to an automated reminder system that can trigger reminders by phone, text, email or postal mail.
In addition, as part of the practices’ PVP process, patient care gaps should be reviewed and flagged as part of the daily huddle. See Key Activity 10: Develop or Refine a Pre-Visit Planning Process for more details.
An example of this is the Axis Community Health project implemented through participation in the Population Health Learning Network. Axis Community Health wanted to improve its behavioral health data infrastructure to better track patient outcomes, adjust treatment and provide quality care. This case study describes the registry they created, key changes and outcomes.
5. Develop a process for reviewing gaps at the population level.
Suggested team member(s) responsible: panel manager.
Set a report frequency to review care gap reports at regular care team meetings or huddles in order to develop a plan for improvement at the population level. This may include an outreach campaign to build community awareness of the value of screenings and the availability of easily accessed screening services. Reports should be able to be drilled down to the clinician level for accountability and used by the care team to improve performance.
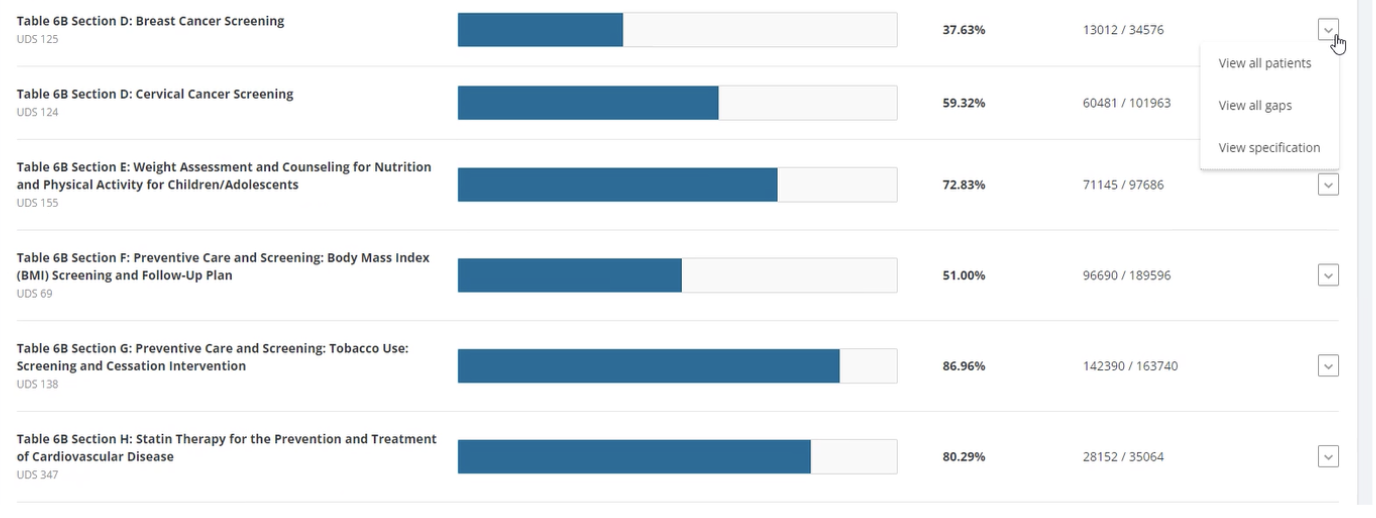
FIGURE 8: EXAMPLE OF A POPULATION CARE GAP REPORT DASHBOARD
Implementation tips
- Consider using other practice staff to help close gaps in care. For example, front office staff can assist with scheduling a follow-up nonacute visit to address gaps in care if a patient comes in for a sick visit.
- Consider incorporating chronic disease management into sick visits to further expand patients’ opportunity to receive care.
- Treatment intensity required for a patient can be benchmarked between providers in a practice. This can be accomplished by comparing treatment intensity rates over a period of time (i.e., three months), which can then be compared to the clinical effectiveness of interventions (i.e., diabetes control or hypertension control).
Resources
Evidence base for this activity
Conderino S, Bendik S, Richards TB, Pulgarin C, Chan PY, Townsend J, et al. The use of electronic health records to inform cancer surveillance efforts: a scoping review and test of indicators for public health surveillance of cancer prevention and control. BMC Medical Informatics and Decision Making. 2022 Apr 6;22(1).Sequist TD, Zaslavsky AM, Marshall R, Fletcher RH, Ayanian JZ. Patient and Physician Reminders to Promote Colorectal Cancer Screening. Archives of Internal Medicine. 2009 Feb 23;169(4):364.
KEY ACTIVITY #4:
Use a Systematic Approach to Decrease Inequities Within the Population of Focus
This key activity involves all seven elements of person-centered population-based care: operationalize clinical guidelines; implement condition-specific registries; proactive patient outreach and engagement; pre-visit planning and care gap reduction; care coordination; behavioral health integration; address social needs.
Overview
This activity provides guidance for a systematic evidence-based approach for identifying and then reducing inequities for children. It focuses on the first primary driver in PHMI’s equity approach: Reduce inequities for populations of focus.
FIGURE 9: PHMI EQUITY DRIVER DIAGRAM
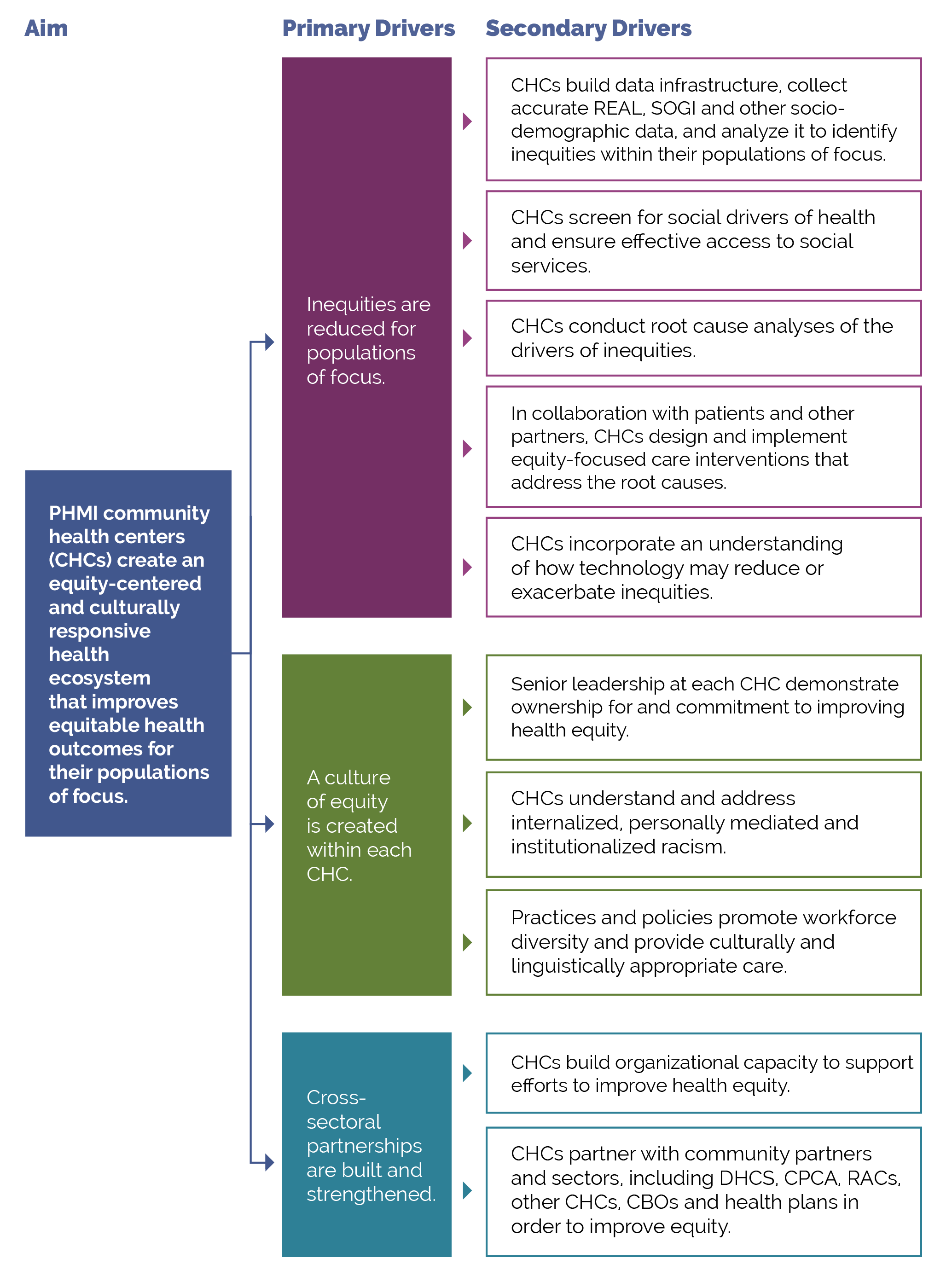
Your practice is likely achieving better outcomes with certain populations or subpopulations and worse outcomes with others. Inequitable outcomes are often the result of social and cultural factors that serve as barriers to accessing care. They are generally most acute among persons of color, immigrants, persons speaking a primary language other than English and other populations who have been marginalized. As we work to reduce and, over time, eliminate inequitable health outcomes, we need to understand both what contributes to these different outcomes as well as factors that do not contribute to them
This includes recognizing that race is a social construct determined by society’s perception. While some conditions are more common among people of certain heritage, inequities in conditions such as cancer, diabetes and adverse maternal outcomes have no genetic basis. While genetics do not play a role in these inequitable outcomes, the extent to which inequities in the quality of care received by people of color contribute to inequitable health outcomes has been extensively documented.[6] These inequities are often a direct result of racism, particularly institutionalized racism – that is, the differential access to the goods, services and opportunities of a society by race.[7] Racial health inequities are evidence that the social categories of race and ethnicity have biological consequences due to the impact of racism and social inequality on people’s health.[8] It is also critical to recognize that we have policies, systems and procedures that unintentionally cause inequitable outcomes for racial, ethnic, language and other minorities, in spite of our genuine intentions to provide equitable care and produce equitable health outcomes.
Improving your practice’s key outcomes for each population of focus requires a systematic approach to identifying equity gaps (e.g., who your practice is not yet achieving equitable outcomes for) and then using quality improvement (QI), collaborative design, systems thinking and related methods to reduce these equity gaps.
Identifying and meeting patients’ social needs are key drivers of reducing inequitable health outcomes. We provide additional guidance in this key activity on how to both reduce inequities and meet patients’ social health needs.
Access to the data required to identify and monitor inequities, as outlined in the key actions below, is fundamental to this activity.
Relevant HIT capabilities to support this activity include care guidelines, registries, clinical decision support (modifications required to consider disparate groups), care dashboards and reports, quality reports, outreach and engagement, and care management/care coordination (see Appendix E: Guidance on Technological Interventions).
EHRs have the ability to capture basic underlying socioeconomic, sexual orientation and gender identity (SOGI) and social needs-related data but may in some cases lack granularity or nuances that may be important for subpopulations. Mismatches between how the UDS captures REAL data versus how EHRs capture or MCPs report data can also create challenges. This may require using workarounds to capture these details. It is also important to ensure that other applications in use that may have separate patient registration processes are aligned. Furthermore, tracking inequities in accessing services not provided by the health center may also require attention to data sources or applications outside the EHR.
Health centers should also be alert to the potential for technology as a contributor to inequities. For example, patient access to telehealth services from your practice may be limited by the inequitable distribution of broadband networks and patient financial resources (e.g., for phones, tablets and cellular data plans). The Techquity framework can be a useful way to structure an approach to ensure that technology promotes rather than exacerbates inequity.
Language, literacy levels, technology access and technology literacy should also be considered and assessed against the populations served at the health center.
Action steps and roles
1. Build the data infrastructure needed to accurately collect REAL, SOGI, social needs and other demographic data.
Suggested team member(s) responsible: data analyst.
- Race, ethnicity and language (REAL)
- Sexual orientation and gender identity (SOGI)
The PHMI Data Quality and Reporting Guide provides guidance and several resources for collecting this information. According to this guide, the initial step in addressing inequities is to collect high-quality data that fosters a holistic view of patient characteristics and needs. This entails incorporating REAL data, demographic data (age, SOGI, geography) and social needs data. By collecting and monitoring this information, healthcare practices can gain valuable insights into inequities in access, continuity and health outcomes. Steps 2 to 4 below provide more information on this process.
Collecting REAL information allows practices to identify and measure inequities in care while also ensuring that practices are able to interact successfully with patients. This is done by understanding patients’ unique culture and language preferences.[9] KHAQuality.com has a toolbox that assists with REAL data collection.
The Uniform Data System Health Center Data Reporting Guidance (2023 Manual) provides detailed guidance on REAL and SOGI. Note: While UDS does not currently require that practices report on the specific primary language of each patient, practices should make an effort to identify and record each patient’s primary preferred language since UDS reporting still requires languages other than English to be reported.
Accurate data collection requires appropriate fields and options in the EHR and other employed technologies, as well as appropriate human workflows in collecting the data. Staff responsible for data collection should be continuously trained and assessed for best practices in data collection, including promotion of patient self-report.
In addition, practices should work to ensure that patients understand the importance and use of this information to help them feel comfortable with supporting its collection. High rates of “undetermined” or “declined” responses in these fields may be indicative of the need to train staff in how to ask these questions and to communicate the importance of the information and how it will be used to improve the healthcare the patient receives. An example of how this was incorporated into a practice was Lyon-Martin Community Health Services partnering with its EHR provider in order to build trust with disclosing this type of data.
Collecting this data is important, especially to obtain a complete picture of health for patients who identify as transgender. There are certain risks and condition indicators that are gender specific, which impact how clinicians provide care to a patient. The World Professional Association for Transgender Health has provided further guidance regarding standards of care related to gender diversity.
2. Use the practice’s EHR and/or population health management tool to understand inequitable health outcomes at your practice by stratifying your data.
Suggested team member(s) responsible: data analyst.
This includes reviewing your care gap report/care registry and being able to stratify all of the following:
- Core measures for the population of focus.
- Supplemental measures for the population of focus.
- Process measures for the population of focus.
Stratify this data by:
- REAL.
- SOGI.
- Other factors that can help identify subpopulations in need of focused intervention to reduce an equity gap (e.g., immigrants, people experiencing homelessness, etc.).
This is not a one-time event, but rather a continuous process (see step 13 below). It should be done in tandem with step 3 below.
Each practice should define the frequency of review and use of its registry to stratify data. In early use, the stratified data will support the identification of areas of inequity and allow for interventions to be prioritized.
3. Screen patients for social needs.
Suggested team member(s) responsible: care team.
Key Activity 17: Use Social Needs Screening to Inform Patient Treatment Plans provides guidance on screening patients for health-related social needs and how the information can begin to be used to inform patient treatment plans, including referral to community-based services. This is not a one-time event, but rather a continuous process. It should be done in tandem with step 2 above.
4. Analyze the stratified data from steps 2 and 3 to identify patterns in inequitable outcomes within the population of focus.
Suggested team member(s) responsible: data analyst, QI leads and care team.
Analyze the stratified data from steps two and three to identify patterns in inequitable outcomes.
This includes:
- Utilizing tools to examine, visualize and understand disparities across different populations or subpopulations.
- Data over time (using run charts).
- Exploring trends, patterns and significant differences to understand which demographic groups will require a focused effort to close equity gaps.
Update your practice’s measurement strategy so your practice’s improvement efforts remain centered around advancing equitable outcomes. Some examples include creating specific, measurable, achievable, relevant, time-bound, inclusive and equitable (SMARTIE) goals and updating your process and outcome measures so you can understand differences by REAL or SOGI indicators. See Appendix C: Developing a Robust Measurement Strategy for more.
This is not a one-time event but rather a continuous process (see step 13 below). Periodic review of stratified data allows for recognition of gap closures and emergence of new disparities.
5. Conduct a root cause analysis for each subpopulation that the practice does not yet have equitable outcomes for.
Suggested team member(s) responsible: multidisciplinary team.
Select root cause analysis approaches that work best for the equity gap you are closing include:
- Engagement with and gathering of information from patients affected by the health outcome in your root cause analysis (see step 6).
- Brainstorming.
- Systems thinking (understanding how interconnected social, economic, cultural and healthcare access factors may be impacting the health outcome).
- Tools that rank root causes by their impact and the feasibility of addressing them (e.g., a prioritization matrix and/or an impact effort matrix).
- Visual mapping of root causes and effects (e.g., fishbone diagram).
- Focused investigations into selected root causes to gather qualitative data through interviews, surveys or focus groups with the subpopulation of focus.
Present the findings to a broader group of stakeholders to validate the identified root causes and gain additional insights. Incorporate the stakeholders’ feedback and refine the analysis, as needed.
6. Partner with patients to develop insights that will help you develop successful strategies.
Suggested team member(s) responsible: care team and people with lived experience (patients who are members of the population[s] of focus).
Using one or more human-centered design methods, such as focus groups, 7 - Stories, Journey mapping, etc. (see links to these methods below), work with members of each population of focus to better understand:
- Their assets, needs and preferences.
- Cultural beliefs, including traditional healing practices.
- Beliefs and level of trust in healthcare generally and in the topic of focus specifically (e.g., cancer screening, immunizations, behavioral health, etc.).
- Barriers to accessing care.
- Barriers to remaining engaged in care.
- Trusted sources of information or communication mechanisms for this population.
- Their ideas for improving health outcomes.
The patients you partner with for this and other steps in this key activity may be part of a formal or informal patient group and/or identified and engaged specifically for this equity work.
7. Identify key activities that address or partially address the root causes of the identified equity gaps.
Suggested team member(s) responsible: care team and people with lived experience.
Based upon the insights your practice has developed for a population of focus and your root cause analysis, determine which of the key activities in this implementation guide could address or partially address the equity gap. This could also include making physical adjustments to the environment in order to make the practice more welcoming or culturally responsive.
Most of the key activities in this guide either explicitly address an equity challenge or can be adapted to better address an equity challenge. Examples of key activities that can be adapted to reduce identified equity gaps include (but are not limited to):
- Key Activity 20: Strengthen Community Partnerships.
- Key Activity 11: Screen for Chronic Conditions.
- Key Activity 8: Proactively Reach Out to Patients Due for Care.
- Key Activity 17: Use Social Needs Screening to Inform Patient Treatment Plans, such as providing a referral for one of the CalAIM Community Supports.
- Key Activity 18: Coordinate Care.
- Key Activity 22: Continue to Develop Referral Relationships and Pathways.
- Key Activity 23: Strengthen a Culture of Equity.
8. Develop new strategies/ideas to address the identified equity gaps.
Suggested team member(s) responsible: care team and people with lived experience.
If one or more of your root causes cannot be addressed fully through key activities in this guide, use one or more human-centered design methods (see resources below) to develop ideas to improve health outcomes and reduce inequities among people with chronic conditions.
Developing these ideas is best done with representatives who are diagnosed with a chronic condition (as they have expertise and experience that may be missing from the practice’s care team). Compensating these patients and community members for time spent on improvement activities is a best practice. During this brainstorm, you are developing ideas without immediate judgment of the ideas in an effort to generate dozens of potentially viable strategies.
Selected resources on human-centered design and collaborative design
- Center for Care Innovations (CCI) Human Centered Design Curriculum via CCI Academy.
- IDEO’s The Field Guide to Human-Centered Design.
- IDEO’s Design Kit: Methods.
9. Determine which strategies to test first.
Suggested team member(s) responsible: care team and people with lived experience.
Steps 7 and 8 above help your practice identify existing key activities and generate new ideas.
There are many ways to prioritize ideas. The Institute for Healthcare Improvement often recommends a priority matrix.
If you have organized your key activities and new ideas into themes or categories, you may choose to work on one category or select one to two ideas per category to work on.
The number of key activities and/or new ideas that you prioritize for testing first should be based on the team’s bandwidth to engage in testing. Therefore, it is critical to determine the bandwidth for the team(s) that will be doing the testing so that you can determine how many ideas to test first.
10. Use quality improvement (QI) methods to begin testing your prioritized key activities and new ideas.
Suggested team member(s) responsible: care team and people with lived experience.
Nearly all the key activities and all of your new ideas will require some degree of adaptation to use them within your practice and to be culturally relevant and appropriate to your patients.
Use plan-do-study-act (PDSA) cycles, generally starting as small as feasible (think in ones — e.g., one clinician, one hour, one patient, etc.) and becoming larger as your degree of confidence in the intervention grows.
Whenever testing a key activity or new idea, we recommend that the practice:
- Use PDSA cycles to test your ideas and bring them to scale. See more information on PDSAs below in the Appendix C: Developing A Robust Measurement Strategy.
- Generally, start with smaller-scale tests (e.g., test with one patient, for one afternoon, in a mailing to 10 patients, etc.). Use the chart titled How Big Should My Test Be? in the Implementation Tips section below to help you decide what test size is most appropriate.
Develop or refine your learning and measurement system for the ideas you are testing. A simple yet robust learning and measurement system will help you understand improvements, unintended secondary effects and how implementation is going.
By working out the inevitable challenges in the idea you are testing using a smaller-scale PDSA cycle, ultimately, the improvement activity will work better for patients and be less frustrating to the care team. Testing and refining also can eliminate inefficient workarounds that occur when a new process or approach is imposed onto an existing system or workflow.
Select resources on Quality Improvement (QI)
Institute for Healthcare Improvement’s Quality Improvement Essentials Toolkit, which includes:
- Cause and effect diagrams.
- Driver diagrams.
- Failure modes and effects analysis.
- Flowcharts.
- Histograms.
- Pareto charts.
- PDSA worksheet.
- Project planning form.
- Run charts.
- Scatter diagram.
IHI’s Videos on the Model for Improvement (Part one and Part two).
11. Implement (bring to full scale and sustain) those practices that have proven effective.
Suggested team member(s) responsible: care team.
Once an idea has been well tested and shown to be effective on a small scale, it is time for your practice to “hardwire” the idea, approach or practice into your daily work. Consider using the MOCHA implementation planning worksheet to think through:
- Measurement.
- Ownership.
- Communication (including training).
- Hardwiring the practice.
- Assessment of workload.
Sometimes implementation may require that you update your protocol and/or policies and procedures for the populations of focus.
12. Once you have tested, refined and scaled up the initially prioritized ideas, begin testing other ideas.
Suggested team member(s) responsible: care team and people with lived experience.
This might include going back to ideas that were elicited previously but were not initially prioritized for implementation. You might also move through the testing steps above to generate and prioritize new ideas or adapt ideas to better serve additional subpopulations of focus.
13. Establish formal and informal feedback loops with patients and the care team.
Suggested team member(s) responsible: care team.
To help ensure that your practice’s ideas are meeting the needs of patients (and their families), helping to reduce identified equity gaps, and are feasible/sustainable for your practices, it is important to have both formal and informal feedback loops.
For patients (and their families), feedback loops might include:
- Sharing ideas with the population of focus to gather feedback and ensure accuracy before testing.
- Getting feedback from patients directly after testing new ideas with them (and incorporating their feedback into your next test).
- Patient satisfaction surveys (or similar).
- Follow-up calls with a subset of patients to understand what works well and what could be improved.
- Patient focus groups.
- Having the practice’s patient advisory board or similar provide feedback.
- For the care team, feedback loops might include:
- Existing or new staff satisfaction/feedback mechanisms.
- Regularly scheduled meetings/calls to get staff feedback on processes, methods and tools.
14. Continually analyze your data to determine if your efforts are closing equity gaps.
Suggested team member(s) responsible: care team.
This includes regular (at least monthly) review of the stratified measures for all of the following:
- Core measures for the population of focus.
- Supplemental measures for the population of focus.
- Process measures for the population of focus.
- Social needs data.
- Any additional measures collected as part of your testing and refinement effort.
Share the data with patients to both show your work to decrease known equity gaps and to solicit ideas for closing them.
Implementation tips
- When testing a change idea (either a key activity or new idea) for your practice to address a known equity gap, the size of your test scope or group is critical.
- We recommend starting with a very small test (e.g., with one patient or with one clinician) or a small test (e.g., with all patients seen during a three-hour period by one clinician) unless you are certain that the change idea (key activity or test) will lead to improvement (with little or no adaptation for your practice), the cost of a failed test is extremely low, and staff are excited to test the change idea.
- As you learn from each test what is (and is not working), you can conduct larger-scale tests and tests under a variety of conditions. While at first glance this would appear to slow down the implementation effort, starting small and “working out the kinks” as you progressively work to full scale actually save time and resources and are much less frustrating for your patients and care team. The visualization below provides guidance on how big your test should be.
FIGURE 10: HOW BIG SHOULD MY TEST BE?
Resources
KEY ACTIVITY #5:
Expand Clinic Hours Outside of a Typical Work Day
This key activity involves all seven elements of person-centered population-based care: address social needs.
Overview
Clinics may take many approaches to provide person-centered access to care. A potentially transformative approach is to offer appointment times outside the typical workday. For example, you may choose to offer appointments at early morning hours or evening hours at your clinic a couple of days a week, as needed.
Telehealth technology may also be used to supplement and provide flexible hours, since staff may be more able or willing to work early or late hours from their homes.
Patients need accessible healthcare to ensure that they have access to care that meets their needs. Many health center patients work one or more jobs and often have limited time to attend medical visits during what are considered typical business hours. Flexible clinic hours can expand patients’ access to care and could be a good match for staff preferences as they balance work and life responsibilities.
Beyond flexibility, practices should try to be compliant with the California Department of Managed Health Care’s timely access standards for appointment availability. All licensed California managed care plans (MCPs) are accountable for providing this level of access to their members; they annually monitor their contracted primary and specialty providers on these standards. Moreover, Federally Qualified Health Centers (FQHCs) also need to be in compliance with the Health Resources and Services Administration’s requirements for hours of operation, which generally means providing extended hours.
Incorporating patient preferences for expanded clinic hours is a strategy to foster equitable health outcomes through expanded access to care. Patients and families with low income or shift work may have very little flexibility with their working hours and multiple competing priorities for their time. Consider providing increased late afternoon and evening access on weekdays to accommodate higher numbers of visits during after-school and after-work hours. Additionally, consider providing weekend hours, such as limited Saturday morning to early afternoon hours.
This population also may face multiple other obstacles to participating in regularly scheduled preventive care visits that are important to learn about, including a need for medical interpreter services for non-English-speaking patients. Of note, the California Department of Managed Health Care and DHCS mandate that medical interpreter services be available when needed during all appointments.
See Appendix E: Guidance on Technological Interventions for further information.
Action steps and roles
1. Review current clinic operating hours and available data on missed appointments.
Suggested team member(s) responsible: director or QI lead.
The practices’ data manager or QI lead should stratify the data on hypertension and diabetes management to identify groups of patients who are not meeting goals. The data should be filtered by patient demographics to identify subpopulations who are having difficulties keeping appointments in the current schedule.
2. Learn patient preferences about clinic hours.
Suggested team member(s) responsible: staff member.
Practice leadership should identify a staff member or peer leader to reach out to patients and learn the challenges patients have in keeping their appointments. This person should ask open-ended questions about patient preferences for accessing care. Consider asking specific questions about times that would be most convenient for the patient.
3. Query staff to learn their preferences about working hours.
Suggested team member(s) responsible: human resources or clinic leadership.
Clinic leadership or human resources staff may query the staff team along similar lines, asking their preferences about working hours and if current hours may be causing barriers to patients who are attempting to access care.
4. Test flexible clinic hours.
Suggested team member(s) responsible: director.
Review what you learned and run a small-scale test, scheduling patients to fill slots in one or two shifts of the preferred flexible clinic hours. Continue testing different time slots until the team is satisfied that you have learned as much as you need to designate an expanded clinic schedule. Be aware that this step may need to be repeated at intervals to gauge emerging preferences of patients and staff.
5. Designate an expanded clinic schedule and track the results.
Suggested team member(s) responsible: director, human resources and QI lead.
Practices should implement a clinic schedule that incorporates the most-attended appointment windows. Schedule staff time based on staff preferences, and partner with staff to foster a healthy work-life balance. The QI lead should review the rate of kept appointments during the extended hours and compare them to the rate of kept appointments during usual business hours.
For additional interventions to improve appointment access, consider open access scheduling and/or same-day appointments using a similar careful testing and implementation approach.
Resources
KEY ACTIVITY #6:
Incorporate Chronic Disease Management Into Sick Visits
This key activity involves all seven elements of person-centered population-based care: all visits; operationalize clinical guidelines; behavioral health integration; address social needs.
Overview
Ensuring that activities needed to manage chronic conditions are incorporated into sick visit appointments expands access to care and facilitates a “whole-person care” approach. This creates opportunities to build interventions that are responsive to patients’ needs and preferences for engaging in the health system. It also provides opportunities to see if patients are up-to-date on condition-monitoring lab work and if nonacute visits should be scheduled.
Incorporating well-care visits into sick visits meets the patient where they are and maximizes the value of their time in the clinic. Many patients will only seek care when they require a sick visit. Therefore, it is highly valuable to incorporate routine care into sick visits.
Patients and families with lower socioeconomic status are likely to benefit from the ability to access preventive care when they are able to visit the clinic. For example, patients who balance competing demands may struggle to keep scheduled appointments. They would benefit from having the opportunity to engage in wellness care during a sick visit. Due to financial constraints, patients may prioritize urgent care over routine or preventive care.
Clinical decision support to prompt the care team to attend to preventive care during all visits is an effective strategy. Ideally, this would be positioned to be available to the extended care team and not restricted to the medical clinician. Prompting strategies can be reinforced through the availability of care guideline-driven order sets and standing orders available in the EHR. See Key Activity 9: Develop and Implement Standing Orders for more information.
Care quality and care gap reports that are analyzed against visit history can be utilized to track progress by clinician and care team in leveraging sick visit opportunities to meet guidelines.
Action steps and roles
Below is a sequence of steps that practices can use to leverage visit activities.
1. When scheduling an appointment, consider providing longer appointment times for sick visits that will incorporate wellness activities.
Suggested team member(s) responsible: Clinic administration, QI lead
The office staff who schedule sick visits can be helpful in assisting clinical staff to identify patients who are overdue for wellness care. Additionally, office staff can use patient messages, medication refill requests and phone calls as touchpoints to screen for preventive care needs/opportunities.
2. Use pre-visit planning (PVP).
Suggested team member(s) responsible: QI lead, care team lead and frontline staff.
Use a PVP process that includes a pre-visit checklist, data from registries/care gap reports and a staff huddle to identify which patients with scheduled sick visits would benefit from the inclusion of chronic care management activities. The team should determine priority chronic care management activities to include for each sick visit. See Key Activity 10: Develop or Refine and Implement a Pre-Visit Planning Process for more information.
3. Empower rooming staff to engage patients in the decision to do the care activity.
Suggested team member(s) responsible: director or care team lead.
Staff may be required to make a real-time decision about whether to go ahead with addressing wellness needs – keeping in mind that a visit may be lengthened and/or raise topics that patients may not be prepared to tackle when feeling unwell. Care team leaders can empower rooming staff to offer opportunities for patients to engage in wellness care and express the importance of patients’ own priorities.
4. Test new and adapted practices and processes to develop improved workflows and standard protocols for implementing management of chronic conditions during sick visits, focusing first on prioritized areas for improvement.
Suggested team member(s) responsible: QI lead with frontline staff, patients and their families.
Implementation tips
- Consider how your existing technology can be leveraged to automate or partially automate the steps in this key activity (e.g., EHR, automated survey mailers/email platforms).
- Gain input from care teams while implementing this measure. Work with clinical staff to implement this activity in a way that optimizes workflows and supports best patient care.
KEY ACTIVITY #7:
Create and Use Clinician Reminders
This key activity involves all seven elements of person-centered population-based care: operationalize clinical guidelines; implement condition-specific registries; proactive patient outreach and engagement; pre-visit planning and care gap reduction; care coordination; behavioral health integration; address social needs.
Overview
This activity provides guidance on how to develop, configure and use reminders in the Electronic Health Record (EHR) so that clinicians are aware of which patients are eligible for and due for wellness care measures regarding diabetes and hypertension. This activity calls for clinician reminders that flag patients at higher risk as well as patients with likely barriers to accessing care (e.g., mobility issues, speaking a language other than English, etc.).
Clinician reminders are one of several tools that clinicians, Medical Assistants (MAs) and other members of the care team can use to help ensure they are aware of their patients’ need for the various diagnostics required to effectively manage diabetes and hypertension. These reminders reduce the amount of time a clinician spends identifying the preventive services recommended for the patient. They also prompt the clinician to inform and educate the patient.
Focus on equity by using data to identify which populations, subpopulations or groups the current outreach and education efforts do not reach. See the PHMI Data Quality and Reporting Guide for more information.
Collaboratively designing outreach strategies with community partners and current patients promotes cultural humility and sensitivity. Tailored outreach with personalized reminders addresses diverse needs and reduces inequities in access to care for chronic conditions.
This activity relies on similar capabilities as care gap management, utilizing population views and registries to create patient-specific reminders within each patient’s chart. For EHRs that have the capacity to display care gaps, that information can be leveraged to create clinician reminders for patients who might have an upcoming appointment. When that technology is not well developed, information from registries/care gap reports can be utilized to generate lists that enable care team members or other clinical staff to create those reminders. Many EHRs are capable of storing next appointment data that can also be used to differentiate patients who need a clinical reminder versus those who would benefit from outreach.
Other relevant HIT capabilities to support this activity include care guidelines; clinical decision support, including patient-facing clinical decision support; and care dashboards and reports.
Action steps and roles
1. Create a flag or alert in the patient record.
Suggested team member(s) responsible: panel manager or data analyst and practice staff responsible for the EHR.
At the patient level, ensure that the practice’s EHR or population health management tool creates a flag or alert to notify the care team of gaps in necessary care for effective diabetes and hypertension management using the latest USPSTF recommendations in accordance with your practice’s clinical practice guidelines. These alerts enable the care team to maximize the identification of necessary chronic disease management services related to patient visits.
This step may involve people from the practice who work on the EHR if it is not clear if or how the EHR can produce the care gap reports.
An example of what a patient-level care gap alert may look like is included in Figure 11.
FIGURE 11: EXAMPLE OF A PATIENT-LEVEL CARE GAP ALERT
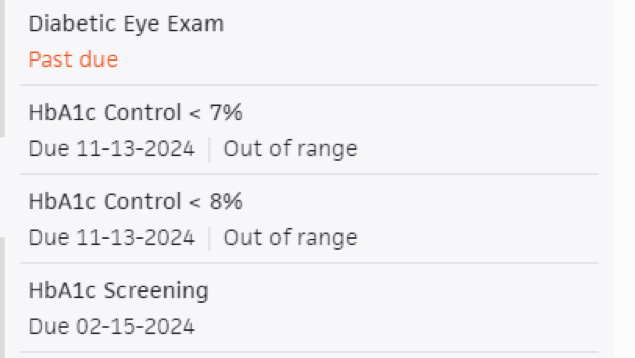
2. Configure the EHR alerts.
Suggested team member(s) responsible: practice staff responsible for the EHR.
Collaborate with the person/team responsible for your EHR to set up automated alerts within the EHR system for patients due for chronic disease management care needs.
Determine the timing and frequency of reminders (e.g., annually, biennially) based on clinical guidelines and patient risk factors.
Work with the care team and the person/team responsible for your EHR to help ensure that the automated alerts are not overlooked when there is an overabundance of alerts. The alerts should be provided at the appropriate time and in a format that is intuitive to the care team.
If possible, the alert should flag those at greater risk (see the USPSTF guidelines).
3. Make clinician reminders a part of the pre-visit planning (PVP) process.
Suggested team member(s) responsible: panel manager.
Work with the clinician and care team to develop ways to ensure these reminders are part of the PVP process (see Key Activity 10: Develop or Refine and Implement a Pre-Visit Planning Process).
4. Ensure reminders are updated continuously.
Suggested team member(s) responsible: panel manager, QI lead, and/or their designee.
Practices should have a process for updating EHR records so that the clinician reminders remain accurate (e.g., do not show a patient needing a lab work that they just had). At a minimum, this process should include:
- The person(s) responsible for doing this.
- Whether the needed exams/lab work was discussed with the patient (yes/no).
- If an exam/lab work was discussed, the patient’s response (yes/maybe/no/not at this time).
- The follow-up based on this conversation, including the results of any exams/lab work and the follow-up needed. Utilize EHR technology to facilitate the follow-up process.
5. Provide ongoing training on creating and using clinician reminders.
Suggested team member(s) responsible: panel manager and practice staff responsible for the EHR
Ensure that all members of the care team receive ongoing training on each of the four steps above. This training can be incorporated into huddles and should be part of the orientation for new staff. At a minimum, it should include ensuring that care team members:
- Know of the reminders and what they mean.
- Understand where, how and when they will receive the reminders. This should include showing each clinician where to locate the reminders and ensuring that the flag or alert is turned on. Any visual reminders should be easily accessible to clinicians.
- Understand the process for updating the EHR to ensure that the reminders are accurate.
6. Monitor clinician reminders for accuracy and completeness.
Suggested team member(s) responsible: panel manager, QI lead, and/or their designee.
It is critical to have a feedback loop with the practice’s care team about any real or potential errors in clinician reminders. Some examples of errors that may occur are:
- Patients who are eligible for and due for screening for whom a reminder or flag does not appear.
- Patients who have recently been screened for whom the reminder or flag continues to appear.
The reminders process should be modified as needed whenever errors are discovered.
FIGURE 12: EXAMPLE OF A CLINICIAN REMINDER
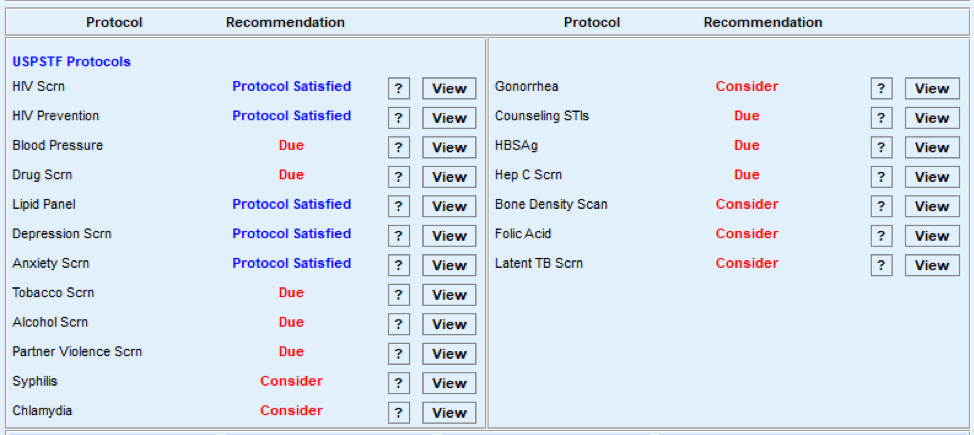
Implementation tips
- If the practice has successfully implemented clinician reminders in other clinical areas, this can be used as the basis for clinician reminders for chronic conditions.
KEY ACTIVITY #8:
Proactively Reach Out to Patients Due for Care
This key activity involves all seven elements of person-centered population-based care: proactive patient outreach and engagement; pre-visit planning and care gap reduction.
Overview
Conducting proactive outreach can ensure patients follow through on recommended care.
As part of PVP and other clinical workflows, your practice should be conducting some level of outreach to provide patients with information they may need to prepare for upcoming visits or engage in follow-up care. In addition, most EHRs can be integrated with an automated reminder system for upcoming appointments and apparent gaps in care, such as a patient being due for an A1c lab or a diabetic foot exam. Patient outreach also occurs as a part of care coordination, especially around supporting patients to engage in external referrals and in follow-up to a hospital admission or discharge (see Key Activity 18: Coordinate Care).
Proactive outreach to patients due for care focuses on identifying subpopulations among the patients assigned to a care team who may benefit from additional outreach and implementing more personalized reminders and “touches” to encourage them to engage in care.
Outreach to people who are not yet actively engaged in care goes beyond this foundational activity. See Key Activity 20: Strengthen Community Partnerships for more about identifying trusted messengers in your community.
Proactive outreach ensures that patients remain engaged in care. It also provides an opportunity for their health needs to be identified and addressed in a timely manner. Untreated health needs can lead to worse outcomes; proactive outreach may improve health outcomes and help ensure that the patient feels that their overall well-being is valued by the practice.
Timely engagement and development of an environment that is conducive to effective chronic condition management can lead to better health outcomes and reduce long-term healthcare costs by preventing the exacerbation of an untreated condition. Patients who have a chronic disease and feel asymptomatic may become disengaged with care if not regularly engaged by their care team.
Focus on equity by using data to identify which populations, subpopulations or groups the current outreach and education efforts do not reach. See the PHMI Data Quality and Reporting Guide for more information.
Unmet health-related social needs (e.g., income security, transportation and health literacy) can result in no-shows and deterioration of patient health status. Proactive outreach, combined with awareness of health-related social needs, ensures that practices can connect patients to community resources while establishing trust in the care team. See Key Activity 17: Use Social Needs Screening to Inform Patient Treatment Plans and Key Activity 20: Strengthen Community Partnerships for more information.
Collaboratively designing outreach strategies with community partners and current patients promotes cultural humility and sensitivity. Tailored outreach with personalized reminders addresses diverse needs, reducing inequities in access to care.
This activity relies on similar capabilities as care gap management, utilizing population views and registries to track gaps in adult preventive healthcare against screening guidelines. These registries can be utilized to generate outreach lists for appointment schedulers and/or care managers and other care team members who might be tasked with contacting patients due for services. Many EHRs are capable of storing next appointment data that can also be used to generate lists and may link to automated appointment outreach workflows. Patient-facing outreach and engagement technologies can be utilized for delivering appointment reminders and for patient self-scheduling. Care managers might use care management applications to track and prompt adult preventive health needs, as well as wellness visits.
Other relevant HIT capabilities to support this activity include care guidelines; clinical decision support, including patient-facing clinical decision support; care dashboards; and reports. Some health centers may focus extra resources on adult patients identified as high risk through risk-stratification algorithms.
Action steps and roles
1. Identify subpopulations among your patients who may benefit from outreach.
Suggested team member(s) responsible: panel manager or data analyst with care teams.
Some methods for identifying subpopulations to reach out to may include:
- Start with frequent no-show patients. Seek to understand their reasoning behind the no-shows, which may be related to social health-related needs or health literacy issues.
- Ask your care teams to identify patients they consider high-risk patients who have been lost to care.
- This may also include reaching out to patients who have not been seen in the last 12 months.
- Conduct outreach to patients whose last blood pressure was not controlled but who did not have a follow-up.
- Use care gap reports to identify patients who are behind on screening or who have missed a follow-up visit.
- Review all patients who are due for a follow-up review of their care plan or who have not had an updated blood pressure or glucose laboratory test; prioritize those patients for outreach.
See Key Activity 3: Use Care Gap Reports or Registries to Identify All Patients Eligible and Due for Care for more information.
2. Establish the outreach model for your practice.
Suggested team member(s) responsible: practice leadership.
One commonly used outreach model is to hire dedicated staff as population health specialists who are responsible for using care gap reports to conduct proactive outreach and to schedule follow-ups. See more about this in the PHMI Care Teams and Workforce Guide Resource 2: Care Team Duties and Recommended Education and Licensure resource.
Different teams may adjust this role to fit their needs. This model ensures that each care team includes staff with knowledge of the local environment.
Train all outreach staff in cultural humility, motivational interviewing skills and the use of trauma-informed care. See more in the resource: Trauma-Informed Population Health Management.
3. Supplement your reminder system for contacting various subpopulations.
Suggested team member(s) responsible: population health specialist, with guidance from implementation team and IT staff.
Reminders should be sent to all persons with an upcoming scheduled appointment. The clinic scheduling system will likely have a function for generating automated reminders with an option for patients to cancel or reschedule if they cannot keep the appointment. Reminders should also be sent to all patients who appear to have gaps in care and missed appointments. See more about updating your care gaps reports to enable setting up automated reminders in Key Activity 3: Use Care Gap Reports or Registries to Identify All Patients Eligible and Due for Care. The reminders could include a request to bring medications and any home-monitoring readings, such as home glucose and blood pressure readings. These are valuable resources for clinicians as they allow the clinicians to complete an accurate medication reconciliation and review the readings during the patient’s appointment.
Automated reminder systems support efficiency and reliability. However, more intensive reminders where the patient receives a personalized telephone call from their care team may help patients who are at higher risks of nonattendance or being lost to care.[10]
FIGURE 13: PROACTIVE OUTREACH AND ENGAGEMENT
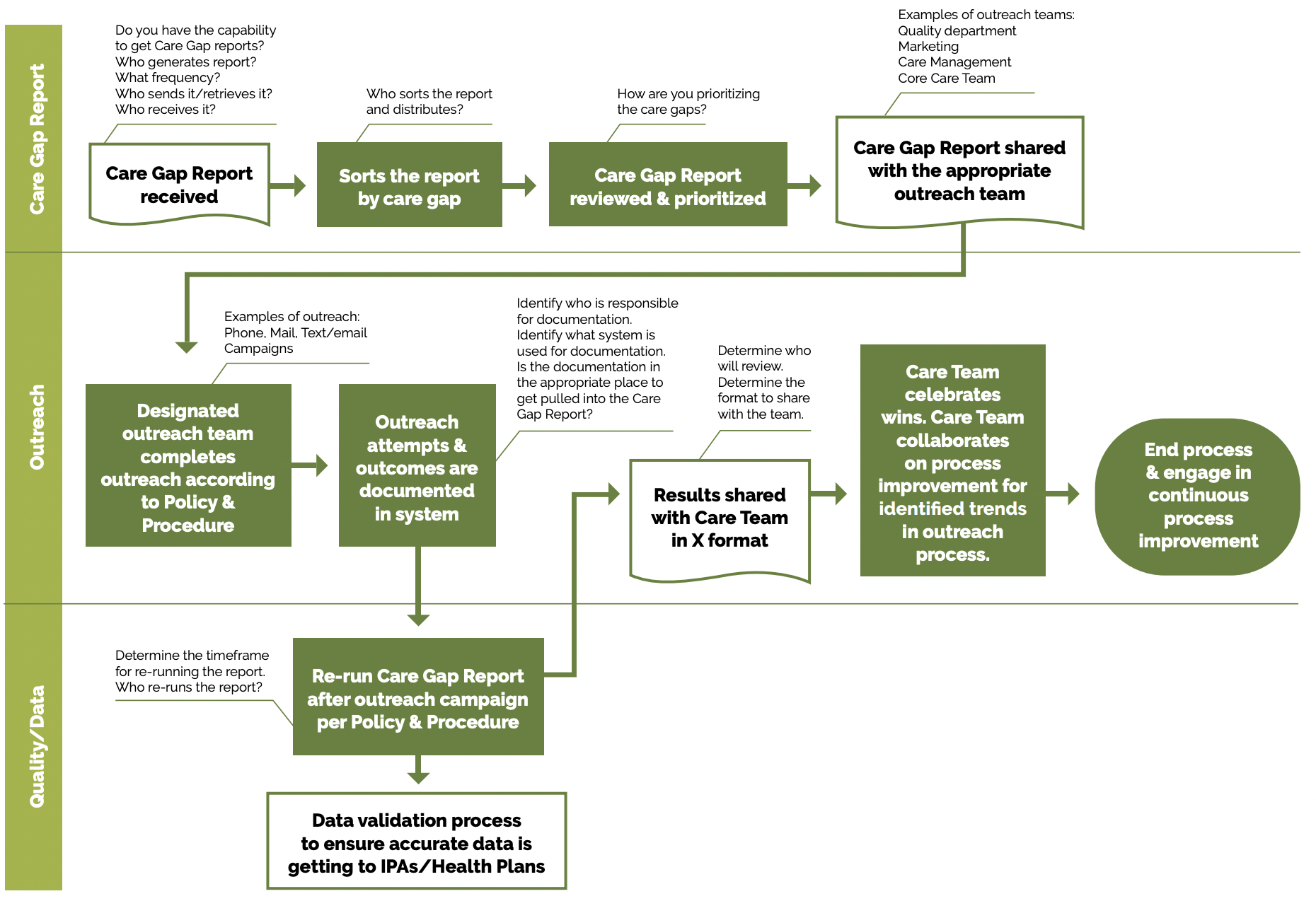
See the PHMI Care Teams and Workforce Guide Resource 6: Workflow Examples for more information.
Utilize multiple pathways to reach and engage patients. For example, a Swiss clinic used sequential appointment reminders consisting first of a phone call and second a text if patients did not answer the phone after three attempts. If the patient had no phone number listed, they received a postal reminder two days prior to their appointment. The reminder system significantly reduced the rate of missed appointments and allowed the clinic to reallocate 28% of the canceled appointments.[11]
Reminders should accommodate language requirements, as well as stated patient communication preferences (text, email, mail or phone). Reminders that include standard information (appointment date, time, clinic location), as well as information about what to expect and additional clinical information, may be more effective.[12]
4. Use “touches” that provide alternatives to the traditional office visit.
Suggested team member(s) responsible: extended care team, including community health workers and population health specialist, with guidance from implementation team.
Assess what types of interactions/care can be provided outside of a typical office setting. Collaborate with patients as part of their care planning to understand their preferences for communication and care team interactions. Examples of alternative interactions include, but are not limited to:
- Nursing staff visits (virtual).
- Pharmacy visits.
- Digital communication through emails, texts and patient portals.
- Newsletters focused on a specific condition.
- Social media that includes discussion groups related to the management of conditions of focus.
- Home visits for high-risk, underserved, or mobility-challenged patients.
- Other technological solutions, such as apps focused on patient conditions that provide a vehicle for ongoing engagement.
For patients with diabetes, group visits often can result in peer support systems that contribute to health literacy and assist with addressing health-related social needs. See Key Activity 19: Provide Group Visits for Chronic Care Management for more information.
Foster patient’s ability to self-monitor their diabetes and/or hypertension at home: For patients with hypertension and/or diabetes, empowering patients to self-measure their blood pressure can influence their health literacy and lifestyle choices. See Key Activity 24: Develop System to Provide Remote Patient Monitoring for more information.
5. Establish a process for engaging patients assigned to your practice by their managed care team who have not yet been seen by the practice.
Suggested team member(s) responsible: multidisciplinary implementation team.
Depending on your agreement with the health plans, it is important for practices to make a proactive plan to build capacity to accommodate assigned-but-not-yet-seen health plan patients in the clinic. Practices should develop strategies for outreach and engagement with these populations in order to shift them from not yet seen to fully engaged in primary care.
6. Continuously reassess outreach approaches with a goal of improvement.
Suggested team member(s) responsible: population health specialist.
Test your outreach approaches and measure their effectiveness. Outreach can be measured by reviewing data from missed appointments, numbers lost to follow-up, etc.
Survey patients to obtain retrospective and prospective feedback on outreach efforts.
Regularly update outreach strategies based on community feedback and changing demographics.
Implementation tips
Providing more intensive outreach: For high-risk patients or patients with complex health and social needs, consider care management as a more intensive approach for facilitating ongoing communication and coordination (See Key Activity 21: Provide Care Management and Key Activity 18: Coordinate Care).
Exploring one-time outreach efforts: If there is a backlog of patient care gaps, consider a campaign where you focus on closing gaps for specific screenings, labs or vaccines.
Going deeper with community partners: Consider strengthening community partnerships to provide greater infrastructure for closing gaps in care (see Key Activity 20: Strengthen Community Partnerships). Community partners can support outreach and health literacy efforts, participate in collaborative design by providing insight around a particular patient population, and provide resources and supports for patients. For example, education and programs on chronic conditions can be made broadly available through community partners (such as schools, community gathering places, churches, senior centers, etc.), which allows for community health improvement beyond the typical reach of the practice. Consider nontraditional community partners that allow practices to reach patients where they are.
- A more intensive approach to outreach involves the more real-time information flow between the clinician and the patient enabled by RPM programs. See Key Activity 24: Develop System to Provide Remote Monitoring for more information.
- The Sonoma County Indian Health Project used a script to talk to patients about joining its program that focuses on preventing heart attacks and strokes in patients with high blood pressure, high cholesterol and high glucose levels.
- This patient brochure from San Francisco Health Network educates patients on strategies to identify risk factors for heart disease and improve blood pressure.
Evidence base for This activity
Biola H, Deyo J, Hayes T, Small L, Chaplin J, Pak-Harvey E, et al. Reaching the Hard-to-Reach: Outcomes of the Severe Hypertension Outreach Intervention. American Journal of Preventive Medicine [Internet]. 2020 Nov 1;59(5):725–32. Available from: https://www.ajpmonline.org/article/S0749-3797(20)30291-9/fulltextDenberg TD, Myers BA, Eckel RH, McDermott MT, W. Perry Dickinson, Lin CT. A patient outreach program between visits improves diabetes care: a pilot study. International Journal for Quality in Health Care. 2009 Apr 1;21(2):130–6.
KEY ACTIVITY #9:
Develop and Implement Standing Orders
This key activity involves all seven elements of person-centered population-based care: operationalize clinical guidelines; pre-visit planning and care gap reduction.
Overview
A standing order is a preapproved order to perform a specific intervention for any patient who meets the criteria for the order. Standing orders describe the action to be taken and identify who on the care team is authorized to execute the order. They are designed to enable care team members other than the primary care clinician to initiate specific clinical actions to provide timely screening and care, provided that specific criteria are met. Common standing orders include measures such as lab work, immunizations or cancer screenings, which are initiated ahead of the clinician’s time with the patient. An important characteristic of a standing order is that all the patients who meet the criteria for the order receive the same treatment, thereby embedding equity into the clinical approach.
To limit the potential for errors and ensure patient safety, standing orders should be carefully designed, regularly reviewed and revised as necessary. They should be based on evidence-based recommendations and best practices, and they should have broad support from the medical director, practice manager, physicians and other staff. In addition, they should outline the criteria for initiating, modifying or discontinuing a particular course of action or treatment for a patient.[13]
Standing orders allow care team members to work to the full scope of their license and provide infrastructure to support care team members as they work toward greater autonomy. They promote practice workflow efficiency and effectiveness by standardizing care while freeing up time for the prescribing clinician.
Standing orders help promote equity by ensuring that every patient who meets the criteria for an intervention under the standing order is provided with appropriate services, thereby limiting variation that could occur in interpersonal encounters. Standing orders are particularly useful for preventive care and screening for chronic diseases and conditions – such as diabetes, hypertension, cardiovascular disease and cancer – that historically have disproportionately affected certain groups.
Most EHRs have the ability to enable creation of order sets that can be utilized to create standing orders. Order sets are particularly effective for managing a group of standard adult screening orders for a population. (See Appendix E: Guidance on Technological Interventions for more details on implementing order sets in a commercial EHR.) Depending upon the health center’s workflows, these order sets can be placed on the chart by providers or can be drawn down by responsible designated staff according to protocols.
Relevant HIT capabilities to support this activity include electronic access to care guidelines, registries, care gap reports and clinical decision support.
Effectiveness of standing orders can be tracked through registries and care quality reports.
Action steps and roles
The steps below outline the actions and steps required to create standing orders. These steps are adapted from the University of California, San Francisco’s Center for Excellence in Primary Care.[14]
1. Review and understand the latest clinical guidelines for the required standing order and your practice’s already established protocols.
Suggested team member(s) responsible: Quality improvement lead and panel manager or data analyst or medical director (or equivalent).
For guidelines from the United States Preventive Services Task Force (USPSTF), the USPSTF site should be reviewed at least annually and/or upon notification of changes to ensure that the latest recommendations are being used by the practice.
The University of California, San Francisco’s Center for Excellence in Primary Care provides guidance on developing standing orders along with examples of standing orders for several clinical conditions.
Regardless of the specific guidelines being used by the practice, the care team should monitor the website containing these guidelines at least annually and/or upon notification of changes to ensure that the latest recommendations are being used by the practice.
Resources
- USPSTF’s Prediabetes and Type 2 Diabetes Screening Guidelines.
- ADA’s Comprehensive Medical Evaluation and Assessment of Comorbidities: Standards of Care in Diabetes—2023.
2. Translate the appropriate clinical guidelines into a standing order.
Suggested team member(s) responsible: panel manager or data analyst.
The standing order will follow the relevant clinical guidelines (and be updated whenever clinical guidelines are updated).
They should allow registered nurses (RNs), Licensed Vocational Nurses (LVNs), and/or Medical Assistants (MAs) with proper training to initiate the agreed upon standing order process if the patient does not have any clinical history that may require a clinician to address the concern themselves. Actions that may be initiated during a standing order include an order, a referral or a clinician notification of the need for a screening/test.
Some examples of standing orders to review are from the Great Plains Quality Innovation Network, University of California, San Francisco, San Francisco Health Plan and Idaho Health West. Chapa-De Indian Health also developed a diabetes protocol for medication refills, which provides examples of what could be checked prior to refilling a medication as part of a standing order.
Redwood Community Health Coalition (now Aliados Health) provided this policy and procedure template for their patient health centers. It includes standing orders for treatment intensification by registered nurses. The American Academy of Family Physicians developed a plan to assist practices in utilizing standing orders to help teams work to their highest level.
In addition to the written standing order, the practice should develop a standard workflow (or similar tool) outlining how the standing order is to be implemented and how it fits into the practice’s existing workflow (with or without changes to the practice’s existing workflow).
3. Obtain approval for standing orders from clinical leadership.
Suggested team member(s) responsible: panel manager or data analyst and medical director (or equivalent).
For the standing order to be valid and in effect, it must:
- Be approved by clinical leadership at the practice.
- Be signed and dated by a designated valid signatory (i.e., medical director or other physician).
- Include the effective date for the standing order.
Practices should consider including an expiration date to help ensure that the standing order is reviewed and updated regularly. If possible, a notification should be put in place to ensure that the order is reviewed regularly. As the clinical guidelines change or other components of the standing order are updated, the standing order should be signed and dated again by the appropriate party with an effective date for the revision.
4. Train practice staff on how to use standing orders.
Suggested team member(s) responsible: medical director or equivalent.
It is critical that practice staff, both those directly named in the standing order and other members of the care team, receive training on the use of the standing order. Training should include a thorough review of the written standing order, the associated workflow and any additional materials related to the workflow, such as patient education or instructional materials. Documents, such as a checklist, may be utilized to provide resources for clinic staff. This standing orders checklist for diabetic patient visits guides a team-based care approach and ensures that patients get the care they need at each visit.
Training should be provided on each standing order at least annually. Updated training should be provided before the effective date on any revisions. Training should also be part of the orientation for all new members of the practice care team. Based on feedback from the staff, the standing order can be refined to make the instructions clearer (e.g., several staff members who are confused by a specific instruction during training indicates that the instruction needs to be revised).
5. Regularly review the standing order to ensure it is effective.
Suggested team member(s) responsible: clinical director or equivalent (or their designee).
It is likely that one or more aspects of the standing order will not work as planned. For example, the practice’s workflow may not fully support the standing order, the wording may be confusing or the standing order’s protocol may not be followed correctly (i.e., staff are using workarounds). The practice should routinely check for these and other common challenges and revise/update the standing order as needed to ensure that it works for the practice and meets all applicable regulations and guidelines.
Implementation tips
- A basic workflow for other standing orders that your practice already has in place can be used as a starting point when developing a new standing order. Before beginning work on a new standing order, determine whether your practice has existing standing orders that you can learn from as you develop this one.
- Verify if carrying out standing orders is within the legal scope of practice for the staff member intended to carry them out.
- The first two to four weeks after implementing a standing order should be used to test and refine it. We recommend that practices start with smaller-scale tests (e.g., test for one day or one area), study the successes and challenges (including errors), and refine the standing order and/or respective training as needed. Then the practice can test again, increasing the scale of the test as fewer challenges or errors arise.
- Common pitfalls of standing orders:
- Standing orders that are not updated when screening guidelines are revised and that reflect an outdated practice: Practices should assign the task of updating the protocols to a member of the team who is responsible for maintaining the order.
- New staff do not know clinical protocols: If new staff are not instructed on the clinical protocols, a review of standing orders as a core element of orientation for all roles named in the standing order should be implemented.
- Standing orders include the signature of a clinician who is no longer with the practice: Standing orders should be reviewed at least annually and any time a clinician responsible for setting the order changes roles.
- To further integrate behavioral health into primary care, consider what protocols may be appropriate for behavioral health activities, such as screening for depression, anxiety or unhealthy substance use. Screening for depression, substance use, anxiety and health-related social needs does not require a physician order and is often integrated into clinic workflows and pre-visit planning without utilizing standing orders. However, in practice, the distinction between a standing order and a protocol can mean different things to different teams, so there are instances where practices find it useful to create standing orders for behavioral health screenings as a way to support the care team to provide evidence-based practice. See the PHMI People with Behavioral Health Conditions Guide for more information.
Evidence base for This activity
- Alberti LR, Garcia DPC, Coelho DL, Lima DCAD, Petroianu A. How to improve colon cancer screening rates. World Journal of Gastrointestinal Oncology [Internet]. 2015 [cited 2019 Dec 10];7(12):484. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4678395/Ishida K, Weiss E, Kee SA, Yingling CT. Increasing colorectal cancer screening orders using unlicensed assistive personnel. BMJ Open Quality. 2019 Jun;8(2):e000545.
- Percefull J, Butler J. Improving mammography through effective screening, brief intervention, and referral to treatment at a rural health center. Journal of the American Association of Nurse Practitioners. 2020 Jan 16; Publish Ahead of Print.
Resources
KEY ACTIVITY #10:
Develop or Refine and Implement a Pre-Visit Planning Process
This key activity involves all seven elements of person-centered population-based care: operationalize clinical guidelines; pre-visit planning and care gap reduction.
Overview
This key activity provides guidance for how the care team can effectively and efficiently embed preventive care measures into the practice’s pre-visit planning (PVP) process. PVP is typically driven by the medical assistant with help from other care team members. It includes steps taken:
- At the end of the current visit to ensure the patient understands any actions they need to take and to schedule for any follow-up.
- Prior to a scheduled appointment to “scrub” the chart and identify any pre-visit tasks per the pre-visit checklist.
- The day of an appointment, during the daily huddle and before the patient sees the primary care provider (PCP).
- Related resource: Care Team and Workforce Resource 4: Daily Huddles Overview and Process.
The average medical visit at California practices lasts just 15 to 20 minutes, and many patients come to these visits with multiple needs. Pre-visit planning works towards optimizing a team-based approach outside of these short primary care visits so that patients receive comprehensive care in alignment with the latest clinical guidelines and their own preferences.
Pre-visit planning allows for better coordination of care. This can be particularly beneficial for patients with complex health needs, ensuring they receive comprehensive and equitable care. As your practice works to reduce any identified equity gaps, PVP is often a powerful activity for ensuring culturally relevant care as the care team partners with the patient to discuss follow-up actions.
The PVP should incorporate your practice’s process for screening and responding to social needs, including checking whether social needs screening is due. When social needs are identified, the team should be clear on the pathways, both during and after visits, to address and follow up on those needs.
PVP draws upon similar technical enablers as care gap reporting. Likewise, it can be facilitated at the level of the individual patient and at the level of groups of patients coming for a specific team’s care in an appointment schedule block. The format in which planning is done needs to consider the workflow and staffing model.
Relevant HIT capabilities to support this activity include care guidelines, registries, clinical decision support, care dashboards and reports, outreach and engagement, and care management/care coordination (see Appendix E: Guidance on Technological Interventions).
Individual patient-level PVP would optimally be enabled within the EHR, provided the EHR is able to store relevant information, such as assessments, plans, orders and notes outside of a visit note. PVP might also include use of patient-facing applications, such as portals reminders, questionnaires and self-completed screenings/assessments, which ideally would be available to the clinician and care team in the EHR.
Engagement of the expanded care team in PVP requires access by all relevant members of the care team to contribute to and view relevant information. This may require coordination with technology additional to the EHR, such as care coordination and population management applications where relevant information might be stored.
Huddle reports, in which individual patient information can be visualized in summary views across all patients within a session, can require use of technology outside the EHR. However, huddle reports might also be supported by developing reports populated by data from the EHR. Ideally, internal practice/EHR data should be supplemented with external data where such information completes the patient’s current status. If such electronic access is not possible, workflow should include manual reconciliation by history from the patient.
Action steps and roles
1. Assess the current state of the PVP process across your practice.
Suggested team member(s) responsible: implementation team or QI team.
Understand how the process currently works for all visit types (e.g., scheduled, same day, virtual) in light of your practice’s performance on core and supplemental measures.
Compile existing paperwork and process documentation into one place and talk to MAs and other members of the care team to understand their questions and challenges around the PVP process.
Consider making current-state process maps that communicate the major steps in the PVP process and acknowledge pain points or challenges in the process. Pain points are places where the process is not working well for patients, staff or specific subpopulations or demographic groups for whom your data analysis has revealed equity gaps. In addition, pay attention to places where staff are creating workarounds to the process. The presence of workarounds indicates that the process might need further clarification or refinement to support the care team to reliably implement it.
Your team may find it helpful to compile process maps both for the high-level PVP as detailed in Figure 14 and for more detailed documentation for specific clinical workflows.
FIGURE 14: EXAMPLE OF A HIGH-LEVEL PVP WORKFLOW
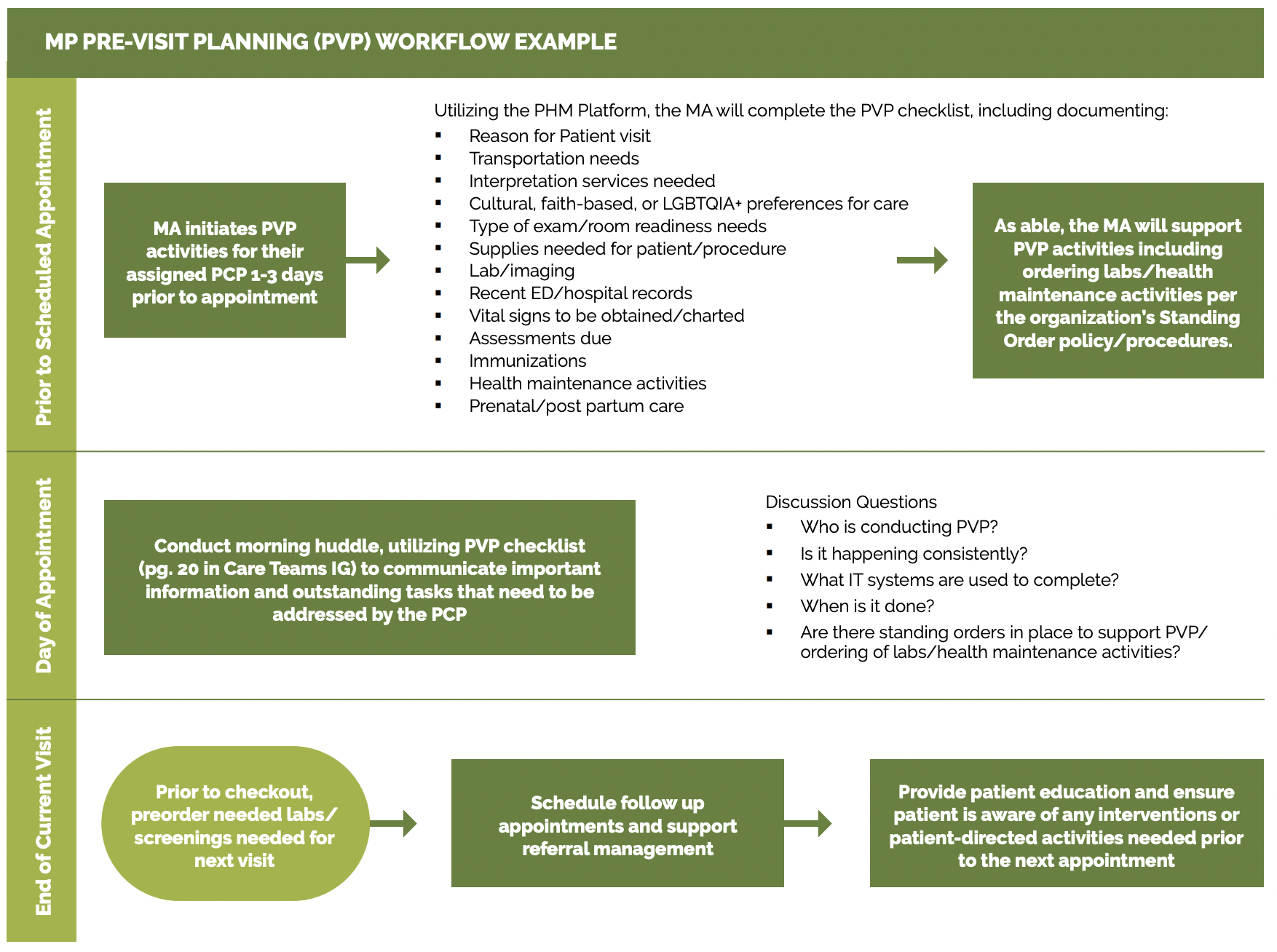
See the PHMI Care Teams and Workforce Guide Resource 6: Workflow Examples for more information.
2. Identify where to update the PVP process to more consistently and reliably address care gaps.
Suggested team member(s) responsible: implementation team or QI team – may include the data manager to assist with identifying patients through EHRs.
Examine where you can further incorporate or streamline your practice’s clinical protocols and standing orders into PVP, including via the PVP checklist, daily huddles and other key clinical workflows.
This may include the following discussion points:
- Who will initiate the discussion with the patient based on the needs (e.g., primary language) and preferences of the patient. It may be beneficial to have communications coaching or training for staff on how to ask or address difficult questions or conversations.
- How and when they will plan to have the discussion during the visit.
- How they will be prepared to address any barriers.
- What educational materials will be available for use that are relevant to the patient.
Examples and considerations for updating the PVP process are included below.
Clinical guidelines and care gaps: Consider which preventive and maintenance services could be addressed more reliably using PVP, including those in your EHR’s care gap module. The Pre-Visit Planning: Leveraging the Team to Identify and Address Gaps in Care resource provides a more complete list of preventive services for adults and children. Figure 15 provides an example of how your EHR might be able to support flagging any patient overdue for common maintenance services (A1c, LDL, nephropathy, eye exams, and foot exams).
FIGURE 15: PVP REPORT DETAILING OVERDUE PREVENTIVE AND MAINTENANCE SERVICES
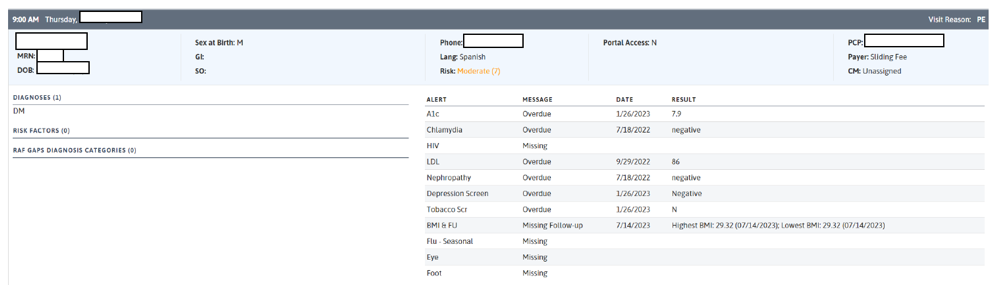
PVP checklist: A generic PVP checklist to be completed by the MA or LVN at least one to three days before the appointment is provided in Figure 16. Most EHRs will have a health maintenance module that identifies what preventive care is due, but a printed or digital checklist provides a starting point for ensuring key steps are not missed.
FIGURE 16: PVP PLANNING CHECKLIST
|
Checklist Domain |
Checklist Item |
|---|---|
General |
|
Room readiness |
|
Medical record review |
|
Screenings are completed by the patient, results are documented, and follow-up is completed. |
For a more complete list of preventive screenings, see the resource Pre-Visit Planning: Leveraging the Team to Identify and Address Gaps in Care. |
|
Scrub chart for care gaps, preclinic labs and missing information: This is not an all-encompassing list of what should be included for PVP; instead, it serves as a starting point to address core HEDIS measures. |
An example chart scrub process led by the MA or LVN as part of PVP for completing open orders is detailed in Figure 17. |
FIGURE 17: EXAMPLE CHART SCRUB PROCESS FOR OPEN ORDERS
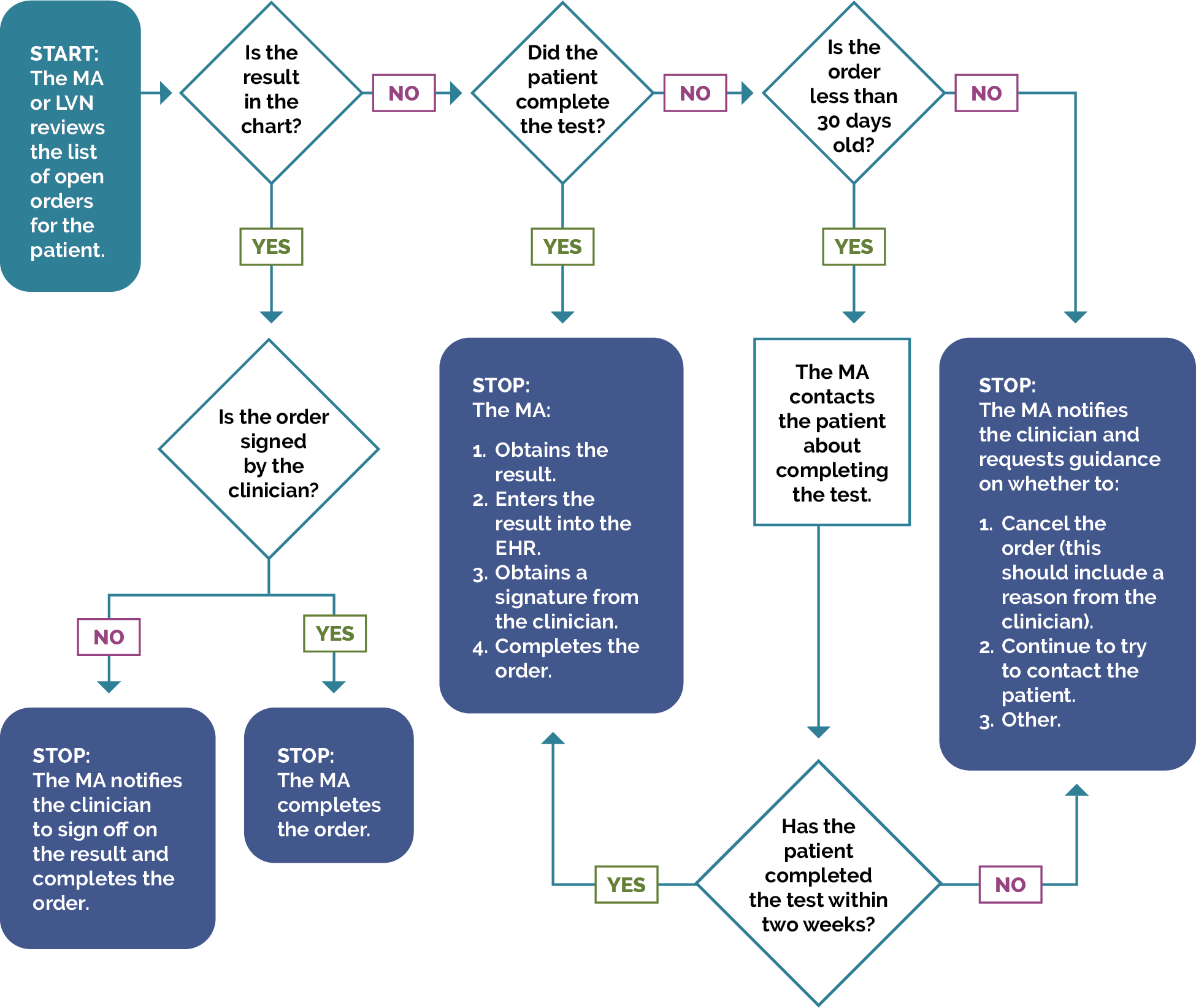
Daily huddles: Design or redesign the team’s daily huddle so the care team can review prioritized action items for the list of patients scheduled to come and any further follow-up for patients seen in the previous days. Work to incorporate it as part of the regular clinic schedule. For more information, see the PHMI Care Teams and Workforce Guide Resource 4: Daily Huddles Overview and Process.
The Center for Excellence in Primary Care resource on Healthy Huddles includes tools, a video and examples of how pre-visit planning (PVP) flows into the daily huddle process, including a healthy huddle warm-up, which can help MAs prepare for huddles.
Patients requiring special considerations: Ensure that the PVP includes a process to flag for the care team:
- Patients requiring special attention, such as those with complex needs or recent hospitalizations.
- Patients who need extended time or additional services during their visit (e.g., translation services, mobility assistance, screenings).
Specific consideration for patients with diabetes: The patient should be contacted one to four days prior to their appointment to ask them to bring in their glucometer and/or readings so that the clinician can review them. Additional steps may be required to prepare for a diabetes management appointment, such as reviewing if the patient has an adequate amount of diabetes management supplies (such as glucose meters, lancets, glucose test strips, etc.) and downloading/uploading the glucometer data if a patient is part of an RPM program. See Key Activity 24: Develop System to Provide Remote Monitoring for more information.
Detailed clinical workflows: Clinical workflows should be updated to describe at which step in PVP or the patient visit a care team member will address a specific gap in care with the patient.
Planning for care after the visit: Effective PVP includes scheduling pre-visit labs and other diagnostics at the end of the current visit, as well as coordinating care and referrals for services not available at the practice. Confirm the patient understands the purpose of any follow-up care. See Key Activity 18: Coordinate Care for more information.
The American Medical Association has an online guide for implementing PVP, which includes forms, templates and other resources.
3. Test planned changes to the PVP workflows and support care teams in implementing the workflow.
Suggested team member(s) responsible: implementation team or QI team.
Test and refine important changes to the PVP process with one or two care teams before considering rolling out the change more broadly at the practice.
Implementing the change includes updating documentation and creating a staff training schedule or training refresher for staff to sustain workflow changes. For example, train MAs every six months on the PVP. If they have difficulty, have them retake training with a different highly effective MA and monitor closely until competency in the task is reached. Infrastructure should be evaluated to ensure that there is adequate training and staff time to effectively complete this process.
Customizing the EHR: For further streamlining of the process, practices can customize their EHR template to align with PVP workflows. Be sure to account for potential costs associated with the creation of new templates, staff training and IT.
An example of this is Golden Valley Health Centers, which outlined workflows for their staff in relation to medication results based upon patient blood pressure results taken while in the clinic.
4. Establish a process to review and update PVP workflow.
Suggested team member(s) responsible: care team with quality improvement manager.
Identify staff responsible for reviewing and updating the PVP process at least annually to incorporate the latest clinical guidelines and check for any workarounds that have developed.
Resources
KEY ACTIVITY #11:
Screen for Chronic Conditions
This key activity involves all seven elements of person-centered population-based care: operationalize clinical guidelines; pre-visit planning and care gap reduction; address social needs.
Overview
Standard screening for chronic conditions reduces morbidity and mortality by detecting disease at an earlier stage, which in turn ensures that clinical management can begin closer to onset. If a patient is diagnosed as prediabetic or has elevated blood pressure, interventions in the form of lifestyle changes can be implemented to help reverse the diagnosis. This activity provides guidance on how to incorporate standardized blood pressure screening protocols and diabetes management protocols into your clinical workflows.
Screening for diabetes and hypertension is important because:
- Early detection and treatment can prevent or delay the onset of serious complications from diabetes and hypertension.
- Effective management of diabetes and hypertension has the potential to reduce the likelihood of adverse outcomes in the future.
Implementing a universal screening process reduces barriers to care by facilitating a process in which people are screened in a manner that promotes equity. Risks related to diabetes and hypertension differ by population. Therefore, having a standard process is crucial to fitting the needs of various populations. It is recommended that for the purposes of hypertension, a blood pressure screening occurs at every visit.
Diabetes and hypertension are conditions that are more difficult to manage and are affected by the social needs of patients. Therefore, systematically assessing social needs and other factors that influence patients’ ability to achieve diabetes and hypertension control (e.g., access to a refrigerator, access to safe places to exercise, access to healthy foods, etc.) is important. By acknowledging and working within the social needs of patients, clinicians can work collaboratively with the patient to make lifestyle and medication adjustments that are tailored to their needs.
Relevant HIT capabilities to support this activity include care guidelines with a specific focus on recommended screenings, clinical decision support and PVP tools.
(See Appendix E: Guidance on Technological Interventions.)
By leveraging PVP strategies, available embedded clinical decision support and screening guidelines, care teams can plan for chronic disease screening. Use of standing orders can support these efforts.
Action steps and roles
1. Utilize appropriate recommendations for screening.
Suggested team member(s) responsible: medical director (or equivalent) and QI officer.
See the ADA recommendations for diabetes screening.
For hypertension, accurate blood pressure measurement should be completed at every visit. Each care team should be provided adequate equipment for screening, including validated, automated monitors and an adequate supply of all blood pressure cuff sizes. The AHA also has resources available that outline protocols for correct blood pressure measurement.
Resources:
- AHA toolkit – poster on steps for accurate blood pressure measurement.
- PHMI Clinical Practice Guidelines.
- USPSTF website.
- ADA Practice Guidelines Resources.
- Centers for Disease Control and Prevention/Million Hearts’ Hypertension Control Change Package.
2. Utilize clinic data to identify any patients who have not been officially identified in their respective registries.
Suggested team member(s) responsible: EHR specialist (or equivalent), QI officer and medical director (or equivalent).
Systems should establish mechanisms for identifying hypertensive and diabetic patients who meet criteria for a respective diagnosis but have not yet been officially identified in their chart documents or have never had their blood pressure taken. This might occur when blood pressure is not tracked over time or when blood pressure is taken incorrectly. More information is provided in the National Association of Community Health Centers’ Hiding in Plain Sight Change Package.
3. Integrate screening criteria into clinical workflows.
Suggested team member(s) responsible: QI officer, nursing officer (or equivalent), and nursing or MA staff.
These workflows may include, but are not limited to, the pre-visit planning process and standing orders. A blood pressure measurement protocol should be established. It is recommended that blood pressure is taken at every visit. See Key Activity 10: Develop or Refine and Implement a Pre-Visit Planning Process and Key Activity 9: Develop and Implement Standing Orders for more information.
4. Evaluate patients further as needed, with appropriate lab work.
Suggested team member(s) responsible: clinicians and medical support team.
Lab work may be appropriate for hypertension after a diagnosis is confirmed to further evaluate secondary causes. For diabetes management, another A1c or fasting blood sugar test might help confirm the diagnosis. Urine microalbumin can help assess for complications.
Chapa-De Indian Health’s diabetes protocols, which address retinal screening, provide an example of the need for further evaluation. The vast majority of patients who develop diabetic retinopathy have no symptoms until the very late stages (by which time it may be too late for effective treatment); this emphasizes the importance of regular evaluation. Additionally, this resource from Alexander Valley Healthcare provides information on workflows and promising practices in diabetic retinal eye exam screening.
The following guidelines should be utilized for the evaluation and treatment of hypertension:
- Establish new diagnosis of hypertension per guideline (two office-based readings >140/90) with confirmation by home readings (>135/85).
- Order baseline tests for new diagnoses of hypertension, including but not limited to the following:
- Complete blood count.
- Electrolytes.
- Creatinine with eGFR.
- Lipids.
- Thyroid stimulating hormone (TSH).
- A1c.
- Urine albumin-to-creatinine ratio.
- Urinalysis.
- EKG.
- Follow established hypertension guideline for blood pressure goals, including home readings (HEDIS, ACC/AHA, Kaiser Permanente).
- Follow preferred medication protocol using fixed-dose combination (FDC) for initiation and titration.
- Utilize team-based care for titration. The team may include a pharmacist, a nurse practitioner/physician assistant, or a nurse.
5. Consider referrals to specialists to assist with further tailoring care plans.
Suggested team member(s) responsible: clinicians and medical support team.
Examples of potential resources to refer patients to include but are not limited to:
- A health coach or behavioral health specialist: They can work with patients to further evaluate any behavioral health screening concerns. Another asset of behavioral health interventions is assisting the patient with developing a plan for manageable lifestyle changes, which can help them best manage the disease. An overview of how this can be accomplished is from Cherokee Health Systems, which uses an integrated behavioral health approach to address a variety of behavioral health concerns.
- A clinical pharmacist or other care team members (if appropriate) who can assist with titration for antihypertensives/hypoglycemics.
Implementation tips
- Consider ongoing quality improvement projects that are linked to correct measurement of blood pressure This may include an unobserved or observed audit, or other process measures, such as repeating a blood pressure when necessary.
- Antidepressant use has been linked to the development of new onset diabetes, particularly with long-term use or higher dosages. It is especially important to screen people with behavioral health conditions for chronic disease.
Resources
National Association of Community Health Centers’ Hiding in Plain Sight Change Package
This change package is a deliverable of the National Association of Community Health Centers’ Million Hearts Hiding in Plain Sight project. It was produced by reviewing the details of the change ideas each health center team employed and any associated tools and resources. This document is a compilation of items thought to be most valuable and to most clearly capture the best that emerged from this work. The change package structure and organization align with the clinical decision support/QI worksheets used to map and identify enhancements to workflows around identifying potential undiagnosed hypertension, engaging patients in care and diagnosing hypertension in a timely and accurate manner. These three steps are critical precursors to managing hypertension successfully and achieving blood pressure control. This change package also aligns with the Centers for Disease Control and Prevention/Million Hearts’ Hypertension Control Change Package.
KEY ACTIVITY #12:
Manage Medication Therapies
This key activity involves all seven elements of person-centered population-based care: operationalize clinical guidelines; care coordination; address social needs.
Overview
Managing diabetes and hypertension with medication therapies requires a comprehensive approach to care, which should be tailored to the needs of each patient. Practices should work to:
- Implement a fixed-dose combination of medications for hypertension.
- Continually assess the need for medications to manage type 2 diabetes and hypertension as some patients can come off antihypertensives with lifestyle change and weight loss (less common).
- Assess and explore patients’ experience regarding unwanted side effects of medication.
- Use preferred medication protocols as per guidelines. Practices should make sure that the guidelines clearly specify which provider types are authorized to make those changes.
Managing medication therapy is important because it helps patients to have better clinical outcomes. It also allows for the use of medications to be streamlined and have a level of regular clinical monitoring, which allows for adjustments to be made on a regular basis in order to best serve patients. Revisiting medication therapy avoids clinical inertia (i.e., when clinicians do not up-titrate medications despite persistence of high blood pressure. The Bellows study (2023) found that treatment intensification is likely the most important driver of blood pressure control.[15]
Clinicians should work to prescribe medications in a manner that is within their best judgment and that promotes equitable access to medications. The chosen plan of treatment should also take into account the patient’s available resources. Clinicians should also work with their care teams to reduce barriers to medication access.
An aspect of effective medication management is to involve patients and families in their care. When deciding upon a medication for treatment, clinicians should involve the patient in deciding upon the type of treatment that best fits their lifestyle. This can include addressing patients’ social needs, as unmet social needs can contribute to difficulties in medication and diet adherence, or more broadly, difficulties in adhering to medication and recommended lifestyle changes.
If a family member or caregiver is involved, they should be included in the conversation so that they understand how to best assist the patient. Care management may also be used to further assist in effective usage of medications.
Relevant health information technology (HIT) capabilities to support this activity include care guidelines, EHR medication lists and alerts, clinical decision support, and medication adherence assessments. Additional tools include condition-specific resources for optimizing medical therapy. When available, clinical pharmacists are an excellent resource for compliance and prescribing recommendations. guidance.
Action steps and roles
1. Consult clinical practice guidelines for how to best manage the condition.
Suggested team member(s) responsible: clinician.
Practices should work to update/implement clinical practice guidelines to ensure they are up-to-date and effective for managing diabetes and hypertension. See Key Activity 2: Update or Implement Clinical Practice Guidelines for more information.
Please also review the following resources:
- PHMI Clinical Practice Guidelines.
- ADA’s diabetes care recommendations.
- AHA/ACC’s 2017 BLOOD PRESSURE guideline.
- Kaiser Permanente’s 2023 diabetes management clinical practice guidelines.
- CCI’s Hypertension Control Change Package.
- American College of Cardiology (ACC).
2. Decide upon a set course of treatment with the patient. If available, a clinical pharmacist may also be consulted.
Suggested team member(s) responsible: clinician or patient or clinical pharmacist (if available).
Clinicians should work to develop a treatment in conjunction with the patient’s wishes. Chronic disease management is significantly related to lifestyle choices. Therefore, it is crucial that a plan is developed to work with the patient’s lifestyle, rather than not taking the patient’s current status into account.
3. Screen patients for assistance programs.
Suggested team member(s) responsible: medication assistance enrollment personnel.
Screen patient for Medi-Cal and Covered California eligibility through the enrollment personnel and then to Medication Assistance Programs if there is a gap or need in their care. Assist the patient (if needed) to enroll them in assistance programs to make medications more affordable, such as Medication Assistance Programs, vouchers or 340B.
4. Decide upon a shared frequency of management with the patient (i.e., every three months, six months, etc.)
Suggested team member(s) responsible: clinician and patient.
Part of the patient’s follow-up should include discussing whether their current medications are still meeting their needs. The patient’s adherence to the medication regime should also be evaluated.
Specific consideration for patients with hypertension
Patients who have uncontrolled hypertension should be followed up at least on a monthly basis until considered controlled. Patients who have controlled hypertension should be seen every three to six months or potentially more frequently based on their comorbidities. This can be done in person or virtually.
For the purposes of regular monitoring, practices should establish a biweekly follow-up for elevated blood pressures. This can occur with an MA/LVN. This follow-up should include looking at home blood pressure readings. See Activity 14: Foster Patients’ Ability to Self-Monitor Their Blood Pressure and/or A1c at Home and Activity 24: Develop System to Provide Remote Monitoring for further information.
Specific consideration for patients with diabetes
The patient should be contacted one to four days prior to their appointment to ask them to bring in their glucometer and/or readings so that the clinician can review them. To determine if the medication is still adequate, the clinician should also take into account the patient’s latest A1c and home glucose readings.
5. Monitor patient for medication adherence.
Suggested team member(s) responsible: clinician, pharmacist and nurse or MA.
Medication adherence should be assessed at every visit or clinical encounter using a question that normalizes missing medications (i.e., “On an average week, how many doses do you miss?”). Ideally, responses should align with pharmacy refill data. Clinicians may be able to obtain pharmacy data to assist with medication adherence monitoring. Suboptimal adherence (typically defined as <80%) should be addressed using standard tools and open-ended questions (i.e., motivational interviewing). Consider leveraging the use of your EHR or patient management platform to obtain this data.
Clinicians should utilize the Medication Refill Adherence Rate (MRAR) and Days of Supply Remaining (DSR):
MRAR:
Like Portion of Days Covered (PDC) but with a few key differences:
- MRAR is more specific to drug class.
- PDC is used for chronic conditions.
Timeline:
- MRAR: rolling 12 months
- PDC: calendar year.
Both systems require that there is a patient count for the denominator.
- MRAR removes inactive prescriptions (the goal is greater than 80%).
- PDC outcomes may be lower than MRAR because the PDC system may still include medications that become inactive in the denominator.
DSR:
Calculates how many days remain of the patient’s current supply. The last prescribed medication for the class should be utilized.
- One challenge of this system is that there may be fewer days remaining if a patient is finishing a prescription when switching to a different medication in the same class.
- For example: When switching from simvastatin to atorvastatin, the DSR system assumes a switch to atorvastatin immediately.
A negative number represents that the patient is overdue for a refill if the medication is taken as prescribed.
- For example, if a patient’s DSR number is −10, they have been out of medication for 10 days.
- A negative DSR may serve as an earlier indicator before the MRAR system that a patient is nonadherent.
6. Manage multiple medications.
Suggested team member(s) responsible: clinician, patient, and clinical pharmacist (if available).
If the patient is taking multiple medications or has difficulties taking or managing their medication, personnel who have enhanced expertise in complex medication management, such as a clinical pharmacist, should be consulted. This is to assist with streamlining the patient’s medication regimen or with making alterations to medication administration (such as bubble packaging) to center adherence towards the patient. Practices should check with the patient’s pharmacy to determine if they can do bubble packaging if appropriate for patient care.
7. Clinicians should be trained to manage common side effects or lab abnormalities of commonly prescribed medications.
Suggested team member(s) responsible: medical director (or equivalent) and Quality improvement lead (or equivalent).
For specific medications, a standard system for follow-up should be established in order to facilitate best patient care. This helps to ensure that side effects are monitored properly. Clinicians should be aware of which medications should be titrated when being stopped, which medication side effects are dose dependent, and how to best manage a side effect that occurs as a result of a medication.
8. If appropriate, utilize care managers to assist the patient with managing their medications.
Suggested team member(s) responsible: patient and care manager.
Patients may be identified for care management based on qualifying criteria as part of risk stratification. Some EHRs may already have this feature available. The American Academy of Family Physicians also provides guidance on risk stratification. See Key Activity 18: Coordinate Care and Key Activity 21: Provide Care Management for more information.
9. Patients who have not been in for their regularly scheduled appointments should be contacted directly if they have not been seen in one year.
Suggested team member(s) responsible: EHR specialist (or equivalent), patient services representative and MAs.
See Key Activity: 8: Proactively Reach out to Patients Due for Care for more information.
10. Reevaluate current medication regime.
Suggested team member(s) responsible: clinician, pharmacist and patient.
If a medication regime is not currently working for a patient, it should be adjusted to achieve their goals per established clinical guidelines. An example of this is from the Sonoma County Indian Health Project, which utilized a pharmacist-led clinic to facilitate switching to glucagon-like peptide-1 (GLP-1) agonists and incorporating lifestyle changes to assist diabetic patients.
Consider updating diabetes treatment regimens to include medications that lower cardiovascular morbidity. This should be based upon the patient’s other health risks, other chronic diseases, etc. Practices should consult the ADA’s latest Standards of Care in Diabetes for further information. For certain populations (such as those at high risk for atherosclerotic cardiovascular disease, etc.), SGLT2 and GLP-1 agents are recommended within the following guidelines:
- For inpatients with established, or high risk for, atherosclerotic disease, heart failure and chronic kidney disease, the treatment regimen should include agents that reduce cardiorenal risk. The ADA recommends using a cardiovascular disease risk calculator to assess risk, such as the calculator on the ACC website.
- A person-centered approach should guide the choice of pharmacologic agents, including (but not limited to) cost and access.
- In adults with type 2 diabetes, a GLP-1 receptor agonist is preferred to insulin when possible.
Before making substantial changes to a patient’s medication regime, practices should determine with the patient if the medications are affordable, therefore making it possible for them to continue adherence. Programs such as 340B or medication assistance should also be leveraged to assist patients in their ability to continue to afford medications.
Example workflow
Chapa-De Indian Health developed a registered nurse case manager workflow and a respective protocol, which encourage medication adherence by allowing diabetes nurse case managers to order refills for diabetes-related medications. This ensures timely refills and promotes patient adherence.
Implementation tips
- If available, integrating pharmacists into the primary care team to provide comprehensive medication management can be greatly beneficial. The University of Southern California School of Pharmacy collaborated with AltaMed Health Services to provide comprehensive medication management for patients with poor chronic disease control, which has been shown to improve care as a whole.
- An effective strategy to effectively monitor adherence is to ask patients to bring in their medications and home blood pressure/glucose meter readings. This is a valuable tool for clinicians when making clinical decisions. Consider utilizing nursing staff to assist with reconciliation.
KEY ACTIVITY #13:
Manage Treatment of Comorbid Hypertension and Diabetes
This key activity involves all seven elements of person-centered population-based care: operationalize clinical guidelines; pre-visit planning and care gap reduction; care coordination; address social needs.
Overview
It is not uncommon that a patient may struggle with comorbid hypertension and diabetes. Hypertension is twice as common in patients who are diabetic compared to those who are not.[16] Therefore, it is fairly likely that clinicians who are treating diabetes will also be treating hypertension. Both of these diagnoses are commonly treated through pharmacological interventions combined with lifestyle change recommendations. Due to the close relationship between the two chronic diseases, it is essential to coordinate and streamline treatments in order to provide high-quality care to patients while also optimizing treatment.
Treating hypertension and diabetes as a group of diagnoses rather than individually is important for the overall health of patients. Having an optimized rather than a separate approach to care reduces the patient’s burden of maintaining complicated care regimes. Due to the nature of these diseases as lifelong illnesses, the treatment plans for these types of care need to be in concordance with, and manageable for, patients to incorporate into their everyday lives. The more a care plan is tailored to a patient’s existing lifestyle and needs, the more likely they will be able to follow it.
To improve social health and equity in relation to diabetes and hypertension management, accounting for social needs and working to minimize the effects of unmet needs will assist in reducing inequities in related health outcomes.
A family unit approach to care, which provides the patient with more support, is a significant asset for achieving effective management of diabetes and hypertension. Involvement from family and caregivers is a crucial aspect of successful management, and it can make interventions more effective. When clinicians develop care plans with patients, caregiver involvement should be considered to ensure that the medication regimen and lifestyle changes are sustainable to the patient.
Relevant health information technology (HIT capabilities to support this activity include care guidelines, EHR medication lists and alerts, clinical decision support and medication adherence assessments. Additional tools include condition-specific resources for optimizing medical therapy. When available, clinical pharmacists are an excellent resource for compliance and prescribing recommendations. guidance.
Action steps and roles
1. Streamline medication regime to ensure that the patient has the most effective treatment with the least amount of medication possible.
Suggested team member(s) responsible: clinician, pharmacist and patient.
Fixed-dose combination medications should be considered to achieve more effective hypertension management.[17] Fixed-dose combination medications help to improve patient adherence, condition control and time to control. Many fixed-dose combination medications are covered by Medi-Cal (on formulary). This may also include employing use of interventions such as bubble packaging, medication delivery and others in order to reduce barriers to care.
2. Determine, in consultation with the patient, which healthy lifestyle changes are acceptable to them that they feel they can reasonably implement.
Suggested team member(s) responsible: clinician, patient and behavioral health consultant (if available).
Examples may include, but are not limited to:
- Increasing exercise.
- Switching to healthier food options (e.g., from white rice to brown rice, from cereal to oatmeal made with rolled oats, etc.).
- Incorporating more fruits and vegetables into the patient’s regular diet.
- Switching to fruits that have lower levels of natural sugar (e.g., switching from oranges to berries).
3. Consult, or refer the patient to, a behavioral health clinician who can assist with change management.
Suggested team member(s) responsible: clinician, patient and behavioral health consultant (if available).
The Shasta Community Health Center Quality Improvement Storyboard provides an example of integrating behavioral healthcare into diabetes care.
4. Refer the patient to other education or intervention options, as appropriate, for further assistance, such as case management, diabetes education or medically tailored meals.
Suggested team member(s) responsible: clinician, patient, and care coordination staff (or equivalent).
Resources
Evidence base for this activity
Petrie JR, Guzik TJ, Touyz RM. Diabetes, Hypertension, and Cardiovascular Disease: Clinical Insights and Vascular Mechanisms. The Canadian journal of cardiology. 2018 May;34(5):575–84.
KEY ACTIVITY #14:
Foster Patients’ Ability to Self-Monitor Their Blood Pressure and/or Blood Glucose at Home
This key activity involves all seven elements of person-centered population-based care: operationalize clinical guidelines; proactive patient outreach and engagement; pre-visit planning and care gap reduction; care coordination.
Overview
This key activity coincides with Key Activity 24: Develop System to Provide Remote Monitoring. Developing a system in conjunction with patients increases partnership between the clinician and the patient. It also assists patients with learning how to best monitor their condition and understand how different actions impact their health as a whole. This is especially important for diabetic patients, who would be able to see that their changing A1c is a direct result of regular self-monitoring. Encouraging self-monitoring allows for a greater degree of specificity and knowledge for clinicians. It also helps patients communicate their questions and concerns more effectively with their clinician.
Patient self-monitoring is important because it helps patients to better understand their condition and how lifestyle choices affect their overall health. For diabetic patients, it helps when adjusting their medication doses (depending on the type of medication that is being utilized). It also allows patients to communicate a more thorough picture of their condition with their clinician during regular visits. Self-monitoring may also be a source of motivation for patients when they can see direct correlative changes in relation to their actions.
Regular home patient monitoring promotes equitable outcomes by putting the patient at the center of their care structure. Regular diagnostic monitoring ensures that an accurate picture is obtained in regards to how effective a treatment plan is within the context of the patient’s everyday life. Independent of the unconscious biases and stressors that exist in a clinical setting, patients can instead be monitored in a safe and comfortable location.
Regular home monitoring may address some barriers to obtaining healthcare, such as lack of transportation. Regular monitoring provides regular updates, which also can encourage clinician teams to intervene skillfully and connect the patient to additional resources that could address any social or other care gaps.
Relevant health information technology (HIT) capabilities to support this activity include RPM technologies (including telehealth), care guidelines, registries, clinical decision support, care dashboards and reports, quality reports, outreach and engagement, and care management/care coordination.
(See Appendix E: Guidance on Technological Interventions.)
Registry data can support the identification of patients who are not meeting clinical goals. With focused outreach, care management resources can be leveraged to engage those patients in a conversation regarding their interest and ability to engage in remote monitoring technologies/telehealth as well as other modalities, as warranted by their condition. Asynchronous communication tools, such as patient portals and texting modalities, can also support these efforts.
Action steps and roles
1. Determine an agreed upon method and frequency with the patient for monitoring their blood pressure and/or glucose.
Suggested team member(s) responsible: medical staff and patient.
This may include, but is not limited to, RPM, journaling, etc. The method and frequency of monitoring should be evaluated regularly with the patient during their appointments. See Key Activity 24: Develop System to Provide Remote Monitoring for more information.
2. Work with the patient to ensure that they know how to properly utilize their blood pressure cuff and/or glucometer.
Suggested team member(s) responsible: medical staff and patient.
If possible, ask the patient to bring in their home blood pressure cuff to calibrate it with the clinic’s sphygmomanometer. One-on-one instruction during a nurse visit is a great opportunity to teach proper use. Training on proper blood pressure measurement technique and/or blood glucose measurement while in the clinic helps the patient to feel confidence while also correcting any improper techniques being utilized.
An example of this is Livingston Community Health, which utilized education to help patients feel adequately equipped to monitor their blood pressure at home.
3. Assist the patient to develop a network of support to help self-manage their chronic condition.
Suggested team member(s) responsible: medical staff, patient and caregiver.
A caregiver, family member or group (e.g., diabetes education or walking group, etc.) Groups are particularly beneficial due to their ability to generate relationships around a shared goal.
4. Assist the patient with understanding certain threshold diagnostics that they should be mindful of, which may warrant medical intervention (e.g., too high blood pressure, glucose value, etc.).
Suggested team member(s) responsible: medical staff.
Patients should be assisted with understanding when to reach out to their clinician with concerns and how to access care after hours for significantly abnormal diagnostics.
Example workflow
La Clinica de la Raza outlined in this case study how they implemented processes for patient self-monitoring of blood pressure.
Open Door Family Medical Centers chose to implement a blood pressure cuff loaner program in order to support a blood pressure patient self-monitoring program.
Implementation tips
- The San Francisco Health Network developed a hypertension toolkit, which provides resources for staff (around self-measured blood pressure monitoring, including coaching for blood pressure cuffs, patient education materials, tools and frequently asked questions) and patients (including resources for home blood pressure cuff instructions for self-measuring blood pressure, logs, worksheets, action plans, healthy food information and more in English, Spanish and Chinese).
- It may be beneficial to consider continuous glucose monitoring for patients. The Sonoma Valley Community Health Center utilized this method for patients who were not routinely checking their glucose levels while using traditional glucose meters.
KEY ACTIVITY #15:
Implement Behavioral Health Screening
This key activity involves all seven elements of person-centered population-based care: operationalize clinical guidelines; pre-visit planning and care gap reduction; behavioral health integration. operationalize clinical guidelines; pre-visit planning and care gap reduction; behavioral health integration.
Overview
This key activity provides guidance on behavioral health screening. The Substance Abuse and Mental Health Services Administration (SAMHSA) defines depression as a disorder of the brain. It causes intense, long-lasting feelings of anxiety, sadness and fatigue, making it difficult for parents to care for themselves, as well as handle daily responsibilities. Universal screening should be implemented in order to ensure that patients are receiving the adequate resources that they need.
Depression plays a significant role in a patient’s ability to manage chronic conditions, especially patients who are diagnosed with diabetes. Behavioral health needs should be addressed in concordance with physical health in order to ensure a wholistic approach to care.
Comprehensive screening in physical, behavioral and social health domains is necessary to identify patients’ needs and wants across a whole-person spectrum of health. It also ensures that patients are able to receive care in a manner that promotes equal access. Treatment for depression in concordance with their chronic conditions involves multiple modalities, including counseling, group therapy and medication; these can be tailored to the patient’s individual needs.
Technology can support screening for behavioral health conditions by delivering structured guidelines, protocols and clinical decision support to care team members responsible for carrying out assessments. It can also help by incorporating standardized screening tools into EHRs and care management/care coordination applications. These screening tools can also be made available directly to patients through patient outreach and screening technologies.
Understanding the prevalence of behavioral health conditions assists in program and resource development to track impact on health outcomes and to incorporate into risk stratification. Health information technologies used to track referrals are also important in care management.
Action steps and roles
Below is a sequence of steps that practices could use to implement screening for behavioral health conditions.
1. Understand current recommendations for regular behavioral health screening.
Suggested team member(s) responsible: QI lead and frontline staff.
Guidance from “the USPSTF recommends that adults be screened for depression, alcohol abuse, and drug abuse, and that primary care physicians ensure there is appropriate diagnostic follow-up available from behavioral health clinicians.”[18] Additional information can be found in the PHMI People with Behavioral Health Conditions Guide.
Please see the USPSTF website for more information:
- USPSTF’s recommendations for depression and suicidality in adults.
- USPSTF’s recommendations for anxiety screening for adults.
- USPSTF’s recommendations for unhealthy alcohol use in adolescents and adults.
- Guidelines are currently proposed for this documentation. Practices should check back periodically to ensure that the most up-to-date recommendations are being utilized.
- USPSTF’s recommendations for unhealthy drug use.
2. Create a care gap report.
Suggested team member(s) responsible: QI lead and frontline staff.
Establish a baseline by assessing the percentage of patients for, or visits at, which behavioral health screening occurred.
See Key Activity 3: Use Care Gap Reports or Registries to Identify All Patients Eligible and Due for Care for more information.
3. Practices should flag all eligible patients for behavioral health screening and administer screening.
Suggested team member(s) responsible: Pre-visit planning staff.
There are many validated tools available. Practices should use tools that are:
- Validated or accepted for use in adults.
- Routinely used.
- Free.
- Easy to administer and score.
- Available in numerous languages.
This should be programmed as an alert in the EHR so staff are aware. These tools can also be used for discussion and planning for the day, such as during morning huddles or during the pre-visit planning process.
To screen for depression, consider:
- Patient Health Questionnaire-2 (PHQ-2)/Patient Health Questionnaire-9 (PHQ-9) (PHQ-2 in Spanish/PHQ-9 in Spanish).
To screen for anxiety, consider:
- Generalized Anxiety Disorder 7-Item Scale, which has seven questions.
To screen for post-traumatic stress disorder (PTSD), consider:
To screen for bipolar disorder, consider:
- Mood Disorder Questionnaire, which has 17 questions.
4. Create a protocol to screen for behavioral health conditions.
Suggested team member(s) responsible: Behavioral health clinicians, medical care clinicians, nursing staff.
Ensure standardized clinical workflows are in place for routine screening for adults. In many practices, MAs or other clinical support staff administer the mental health screenings in advance of the clinician visit. Clinic support staff alerts the clinician to a positive screen, who then reviews the results and, if appropriate, offers relevant treatments or referrals.
To maximize completion of behavioral health screenings, the workflow should be executed at any visit where the patient is new, has not been into the clinic in over a year, or requires regular follow-up. Practices should establish reoccurrence thresholds to ensure that patients are screened routinely as appropriate.
5. Develop workflows for integrating behavioral health during regular patient care, including provision of pharmacotherapy when indicated.
Suggested team member(s) responsible: Behavioral health clinicians, medical care clinicians, nursing staff.
- Identify mental health screening tools to be integrated universally in every clinical setting where patients may present.
- Establish an evidence-based, person-centered response protocol based on what is feasible for each area of practice and local mental health resources. Ideally, responses are tailored to condition severity and are strength based, culturally relevant and responsive to patients’ values and needs.
- Ensure staff can activate an immediate suicide risk assessment and response protocol as needed for patients with identified suicidal ideation, significant risk of harm to self and/or others, or psychosis.
6. Educate clinicians, frontline staff, administrative staff, patients and patients’ designated support networks on optimal care for patients, including detection, assessment, treatment, monitoring and follow-up best practices.
Suggested team member(s) responsible: Behavioral health clinicians, medical care clinicians, quality improvement staff.
- Facilitate trauma-informed training and education to address healthcare team member biases and stigma related to mental health conditions, including anti-racism considerations.
- Incorporate mental health into multidisciplinary rounding to establish a nonjudgmental culture of safety.
- Provide staff and provider training on common modalities to treat depression.
7. Develop and maintain a set of referral resources and communication pathways between the patient’s providers, community-based organizations, and state and public health agencies to address patient needs, including social drivers of mental and physical health.
Suggested team member(s) responsible: Care coordinators, behavioral health staff, quality improvement staff, clinic administration.
Establish care pathways that facilitate coordination and follow-up among multiple providers.
- Identity local resources for mental health conditions that necessitate immediate treatment (i.e., psychosis, suicidality).
Ensure a clear protocol for communication between primary care providers and the patient’s behavioral health providers.
8. Screen and provide linkage to resources for structural and social drivers of health that may impact clinical recommendations for treatment plans.
Suggested team member(s) responsible: Behavioral health clinicians, medical care clinicians, nursing staff.
- Transportation, childcare and housing, among other factors, may impact a patient’s ability to adhere to their mental health treatment plan.
Resources
PHQ-2
Depression screening tools.
PHQ-9
Depression screening tools.
KEY ACTIVITY #16:
Support Patient Self-Care
This key activity involves all seven elements of person-centered population-based care: proactive patient outreach and engagement; care coordination; behavioral health integration.
Overview
The term “self-care” refers to patients’ engagement in the activities and decisions that improve their health and well-being. Supporting self-care involves activities that enhance the capacity of individuals to engage in their care.
To address the healthcare needs of communities, patients and families must have skills and knowledge to make healthy lifestyle choices. This is a daunting task, but primary care practices can help by taking opportunities to enhance patients’ ability to self-manage through provision of resources tailored to patient needs and of coaching in self-care practices.
Evidence suggests that supporting self-care can improve patient outcomes and quality of life.[19] In addition, a focus on the capacity of individuals in underserved segments of the population to engage in their care is foundational to ensuring equitable care delivery.
Underserved populations experience lower rates of health literacy and less access to resources and training for self-care. Health centers can help bridge these inequities by empowering patients through training and coaching support on self-care. Those patients who are more self-activated are better able to navigate their healthcare and social needs.
Relevant health information technology (HIT) capabilities to support this activity include care guidelines, registries, clinical decision support, care dashboards and reports, quality reports, outreach and engagement, and care management/care coordination.
(See Appendix E: Guidance on Technological Interventions.)
Given the challenges with equitable access to technology, a multimodal approach to supporting patients is important. The range of opportunities to provide patient support and education include face-to-face sessions, telephone sessions, asynchronous communication tools (e.g., patient portals and texting modalities) as well as telehealth visits.
Action steps and roles
1. Improve information resources to patients.
Suggested team member(s) responsible: clinic staff; if a patient and family advisory council is in place, ask them to develop and/or refine patient information materials.
- Update patient information materials and have them available in the languages most prevalent in the community. Gaining input from patients is also valuable during this process.
- Support patient use of a patient portal that allows for easy access to the electronic health information.
- Utilize health literacy universal precautions when creating widely circulating resources. The use of universal precautions is an approach to providing health information and services, which assumes that all patients may have difficulty comprehending health information or accessing services.[20] On an individual patient level, being aware of a patient’s level of health literacy helps staff members convey information effectively.
- Discuss a patient’s interest in information about health topics during clinic visits. Rather than assuming that a patient needs and wants certain information, use tips from the field on motivational interviewing to ask open-ended questions.
Tip: Consider holding “onboarding” group visits for new patients, which orient the patients to the clinic, its workflows and resources, and opportunities for self-care support.
2. Identify opportunities to enhance patient knowledge and confidence.
Suggested team member(s) responsible: clinic staff, including social workers, diabetes educators, nurses and clinicians.
Provide patients with tools, such as mobile apps or wearable devices, to monitor their vital signs, physical activity and medication adherence. Regular monitoring enhances self-awareness and accountability.
Offer workshops and classes on nutrition, physical activity, stress management and/or sleep hygiene. Encourage patients to adopt healthier lifestyles through practical tips and motivational support.
3. Implement shared care plans with patients.
Suggested team member(s) responsible: care team; patients; and family members, if appropriate.
Implementing shared care plans (see AHRQ's Develop a Shared Care Plan) involves decisions of:
- How the patient-clinician discussion will fit into the clinic visit workflow.
- Training in facilitating collaborative conversations with patients.
- How the shared care plan will be shared with the patient (e.g., paper, patient portal).
- How the shared care plan will be documented.
4. Address health-related social needs that impact self-care.
Suggested team member(s) responsible: care team.
Implement universal social needs screening and use the results to identify health-related social needs of patients. See Key Activity 17: Use Social Needs Screening to Inform Patient Treatment Plans for more information.
Update a directory of community-based resources (see Key Activity 20: Strengthen Community Partnerships) and routinely refer patients to appropriate resources through the care coordination process already in place. Follow up with patients who have been referred to community-based resources to learn if the referral was helpful.
5. Implement self-management support.
Suggested team member(s) responsible: care team.
Self-Management Support is a technique that enables patients to play an active role in their healthcare. Self-Management Support uses the ask-tell-ask approach, patient-directed goal setting and follow-up to support individuals in making decisions that benefit their health and well-being. Training for staff and clinicians will be necessary to implement Self-Management Support.
Implementation tips
Begin self-care coaching in the exam room. Consider opportunities to leverage the extended members of the care team who often are representative of the populations you are serving. The self-management coaching can be before a patient is seen by a clinician (while waiting for the clinician) and after the patient has seen the clinician. The key is to ensure the self-management coaching is well coordinated by the integrated care team.
Self-care coaching can begin with new patients. Consider holding onboarding group visits for new patients, which orients the patients to the clinic, its workflows and resources, and opportunities for self-care support.
Resources
KEY ACTIVITY #17:
Use Social Needs Screening to Inform Patient Treatment Plans
This key activity involves all seven elements of person-centered population-based care: chronic disease management; behavioral health integration; address social needs.
Overview
This activity provides guidance on screening patients for health-related social needs and how the information can begin to be used to inform patient treatment plans, including referral to community-based services. Social needs are defined as individual material resources and psychosocial circumstances required for long-term physical and mental health well-being, such as housing, food, water, air, sanitation and social support. For individuals with chronic diseases, addressing social health needs can contribute to better management and control of their conditions.[21]
Evidence continues to accumulate that demonstrates not only the ways in which social needs impact physical and mental health outcomes,[22][23][24] but also how worsening physical and mental health conditions can impact social stability.[25][26]
Food and income insecurities are contributing factors to many chronic conditions.[27] Assisting patients with good food choices and sources can contribute to their well-being.
Screening for social needs provides an opportunity to ensure healthcare is provided in the context of life circumstances in which patients and their families are living. This is part of providing holistic, person-centered care.
Health equity is advanced by addressing the underlying issues that prevent people from being healthy. At the population level, this means addressing community-wide health-related social needs and structural determinants. At the individual level, this means acknowledging and beginning to address health-related social needs.[28]
Social needs screening often asks questions about private and potentially stigmatized aspects of a patient’s life (e.g., poverty, interpartner violence).[29] See below in the action steps about screening for and responding to social needs in a trauma-informed way. Be aware that staff may also experience trauma when screening for social needs (e.g., if a staff person has a history of food insecurity or has experienced homelessness in the past). Have a plan to support staff needs.
Note there is not yet consensus or uniform endorsement regarding screening for social needs, due at least in part to a lack of high-quality evidence on the risks, benefits and best practices of screening and response.[30] For example, findings from the recent Centers for Medicare & Medicaid Services’ (CMS’) Accountable Health Communities Model indicate that social needs screening and navigation services reduced emergency department utilization and may have reduced expenditures; however, they did not appear to increase patients’ connection to community services or resolve patients’ social needs.[31] Other possible ways social needs screening can support attending to social needs include strengthening the patient/provider relationship,[32] destigmatizing social services, tailoring care and, at a population level, increasing social investment.[33]
Technology-enabled screening can be utilized to screen patients for social needs through various channels: directly in the EHR, in applications used by care coordinators, and directly to patients via patient-facing outreach and engagement technologies. Practices will need to determine a process to ensure that externally generated screening information is incorporated into the patient record and used for care delivery, risk assessment and management, and management of relevant referrals. Social health information exchanges exist in some communities to identify where patients are getting social services and to help identify higher-risk patients; these will develop over time.
Action steps and roles
1. Pick a validated standardized screening instrument and establish how to document results.
Suggested team member(s) responsible: clinical leadership.
Pick a standardized screening tool that fits your organizational environment and the context of your patient population. Kaiser Permanente, in partnership with the Social Interventions Research and Evaluation Network, conducted a review of social needs screening tools and provides a comparison tool and search tool for different tools for adults and children. Currently available standardized tools you might consider include:
- Protocol for Responding to and Assessing Patients’ Assets, Risks and Experiences (PRAPARE) (developed by the National Association of Community Health Centers Association of Asian Pacific Health Organizations (AAPCHO) and Oregon Primary Care Association (OPCA).
- The CMS’ Accountable Health Communities Health-Related Social Needs Screening Tool.
- The American Academy of Family Physicians’ Social Needs Screening Tool.
Work with your clinical informatics team to determine how staff will document screening results in your EHR. Some EHR systems have screening tools already embedded, and many are moving quickly to incorporate screening. Some EHRs may be able to auto-populate Z codes based on screening results. Your MCPs may offer additional guidance or support and can be a resource to connect your practice to other organizations that have experience with screening instruments and technology tools. By using the same screening tools and/or IT platforms, the consistency and quality of care delivery can be enhanced.
For the patient’s problem list, DHCS provides a list of 25 Priority Social Determinants of Health Codes to focus on. This shorter list of codes is intended to capture areas where the health system may have the greatest impact on identifying and addressing social needs.
2. Understand resources and community referrals for positive screens.
Suggested team member(s) responsible: referral manager and community health workers.
Through CalAIM, the DHCS has taken steps to ensure that Medi-Cal patients have access to social support that can impact health outcomes. Connect with your MCPs and regional area consortia to understand what services and resources they have in place to support patient access to community-based social services. Many MCPs are developing relationships with social services clinicians to meet the needs of their patients. For Medi-Cal patients with the highest level of social needs, MCPs offer ECM (see Key Activity 21: Provide Care Management) and some or all of 14 Community Supports. These Community Supports provide resources to address social needs, such as housing navigation, recuperative care posthospitalization and medically tailored meals. Some MCPs use the new CalAssist tool for Medi-Cal patients to self-identify whether they are eligible for any of the 14 CalAIM Community Supports and generate a referral to the applicable community support provider.
Many patients will screen positive for social needs and will benefit from connection to alternative resources that are not part of Community Supports. Contact your MCP to see if they have established relationships with clinicians who connect individuals to social services. Health plans may contract with an online clinician or with a social services network lead entity that can connect you with existing community-based organizations and public agencies in the area. These contracted services will often include a process for making closed loop referrals, where the referring clinician is notified if the patient has successfully accessed the referral. Closed loop referrals are a best practice in care coordination; they lead to higher levels of patient and provider satisfaction.[34]
Key services to catalog include nutrition assistance, employment readiness, childcare support, postpartum paid family leave, rent/utility assistance and resources for transportation. Other places to look to build sources for local community referrals include:
- Your current social work staff and/or community health workers, who may have many go-to resources already identified.
- Free online aggregators for local community services in California, such as findhelp.org.
- 211, a free telephone number providing access to local community services for housing, utility, food and employment assistance.
- Resource networks maintained by a local hospital or larger health system in your area.
Technologies that facilitate community referrals – such as findhelp.org (Aunt Bertha), Purple Binder’s Transforming How People find Community Services and Unite Us’ cross-sector collaboration software – can also help to facilitate community referrals.
For going deeper in this area, practices can consider prioritizing quality improvement activities that establish new or previously underutilized community resources to address specific social needs as part of your application of Key Activity 4: Use a Systematic Approach to Decrease Inequities Within your Population of Focus. Case studies provided in the resources linked below provide examples of improvement initiatives.
3. Establish a workflow for screening and referrals.
Suggested team member(s) responsible: QI Lead, multidisciplinary workgroup.
Consider screening before the patient meets with the PCP and have a workflow in place for following up a positive screen (e.g., meet with care coordinator or care management staff who will facilitate referral). Take steps to flag the positive screen so the PCP is aware and can address any positive screen during the visits.
Train staff in the new workflows and how to provide trauma-informed screening. Staff often initially resist screening if they feel they do not have the tools to help address positive screens.
Following screening, ask patients for their prioritized need and whether they would like assistance before making a referral.
Provide staff a written script and accompanying signage to build confidence in dealing with the challenging circumstances many patients experience.
4. Provide person-centered care that acknowledges social needs.
Suggested team member(s) responsible: PCPs and the expanded care team.
Information about a patient’s social needs can be used to provide tailored, person-centered care and treatment plans that patients are more likely to follow. For example, if a patient screens positive for food insecurity, that could influence details around dietary advice given for conditions like heart disease or weight management. Use trauma-informed ways of engaging patients in their own care, including developing shared goals, providing self-management support and using communication techniques such as motivational interviewing. See more about Trauma-Informed Population Health Management.
The desires and goals of the patient will inform how and when to move ahead in addressing social needs. It is important to support patients through motivational interviewing and trauma-informed practices to create a person-centered care plan. Having processes in place to support ongoing person-centered care planning (such as a warm handoff to a care coordinator or a documented plan to follow up at the next visit on issues discussed) will help to build trust and support connection to community referrals when the patient is ready.
Examples of how this activity has been implemented
Rogue Community Health in Medford, Oregon, recognized the need to implement screening for health-related social needs. It also recognized that the lack of interoperability in their health information flow was a barrier to collaboration in their community. As a result, it served as a convener and backbone partner, pulling together a group of community-based organizations and public health entities into a “no wrong door model” for screening of social needs. The partnership was called the Rogue Challenge. It resulted in a shared community database where patients could be screened at multiple data entry points and where the life cycle of a positive screen and referral could be tracked to ensure that people with positive screens were connected to community resources and completed their referrals. Together, the collaborating partners selected an appropriate validated social needs screening tool and adapted it to their context. Next, the team tested screening workflows, including the ability to access information and provide additional screens. This approach expanded the capacity of community-based organizations to administer social health screening, which provided the health center with information in advance of a clinic visit. In their value-based care environment, it had the added benefit of identifying new patients not connected to primary care and connecting them to the health center, thus growing their population of capitation patients.[35]
Implementation tips
Start by identifying the most common social needs (e.g., food, housing, secure income) and for each need work to map out an end-to-end process from identification to resolution.
Practice coaches can be resources in this process of mapping, which can include:
- Selection of a screening tool.
- Capture of data within the tool (e.g., Z codes for health-related social needs for future tracking and reporting).
- Development of a referral pathway (including individuals responsible, agencies).
- Definition of success and resolution.
- Ongoing periodic follow-up.
- Seek input from patients, families, clinic staff and referral entities as you develop your process.
Resources
Examples from CCI
Case studies of how practices implemented screening tools and undertook innovative quality improvement activities to address food and transportation insecurity:
Evidence base for this activity
- Califf RM, Wong C, Doraiswamy PM, Hong DS, Miller DP, Mega JL. Importance of Social Determinants in Screening for Depression. Journal of General Internal Medicine. 2021 Aug 17;
- Chavez LJ, Tyson DP, Davenport MA, Kelleher KJ, Chisolm DJ. Social Needs as a Risk Factor for Positive Postpartum Depression Screens in Pediatric Primary Care. Academic Pediatrics. 2023 Sep 1;23(7):1411–6.
KEY ACTIVITY #18:
Coordinate Care
This key activity involves all seven elements of person-centered population-based care: proactive patient outreach and engagement; pre-visit planning and care gap reduction; care coordination; behavioral health integration; address social needs.
Overview
This activity will help you provide care that is person centered and coordinated across all internal and external providers involved with the patient.
Care coordination involves deliberately organizing patient care activities and sharing information among all participants concerned with a patient’s care to achieve safer processes and more effective outcomes.
Care coordination is an integral part of providing high-quality population-based care in an ambulatory care clinic. In your practice, care coordination happens daily as part of standard work and includes activities such as assisting patients with referrals, managing patient messages and receiving incoming information from outside care partners, including pharmacies, specialists, hospitals and community partners (e.g., schools, employers, community-based organizations).
Managing care across multiple settings is often a source of frustration and dissatisfaction for both patients and providers. Lack of coordinated care can result in both duplication of services and lack of completion of needed services. When care is not coordinated, decisions can be made without a complete picture of the patient’s needs and goals. Practices that have effective care coordination processes often employ closed loop referrals as a best practice.[36][37] In a closed loop referral, a referring provider can track the status of the referral (completed or pending) as well as the outcome of the referral, including whether additional follow-up is needed. When closed loop referrals are implemented, both provider and patient satisfaction are enhanced.
There are four fundamental concepts when thinking about care coordination activities within your practice:[38]
- Accountability:
A key to successful care coordination is accountability. Clinics and systems that excel at care coordination take ownership and assume responsibility for care coordination activities. Examples of care coordination processes include development of infrastructure for care coordination, identification of staff responsibilities and relationship building with referral partners. Together, these actions create the ability to support referrals and transitions and track them to completion. - Patient support:
Referrals and transitions often raise questions for patients and families and can be a source of anxiety. Not only do the logistics of a referral or transition create questions, but patients and their families can experience anxiety regarding the outcome or purpose of a referral or transition. When a practice can dedicate staff time to addressing the needs of patients and families, referrals and transitions are most likely to accomplish intended goals. - Relationships and supports:
Referrals and transitions work best when all parties – patients, primary care providers, and consultants – agree on the purpose and importance of the referral, as well as the roles that each will play in providing care. - Connectivity:
Building relationships and agreements among providers (including community agencies) leads to shared expectations for communication and care. Connectivity includes developing referral relationships, accepting accountability and creating data flow.
In order to conceptualize how practices can coordinate with community-based agencies (housing, food, income support), hospitals and ERs, and specialists, refer to the visual depiction of the care coordination model by the Center for Accelerating Care Transformation (ACT Center).
Care coordination can benefit all patients in your practice. Care coordination processes, such as closed loop referrals, can be applicable to many practice activities (see examples below in figure 20). Common areas where care coordination can be enhanced include specialty referrals and referrals to social supports, such as transportation and housing assistance. Care coordination activities can also identify patients who need a higher level of support through a care management program (see Key Activity 21: Provide Care Management). Care management differs from care coordination in that a patient consents to and works directly with a care manager to create a care plan that is shared with an extended care team. While a practice can decide whether it has the resources to provide higher-level care management services, care coordination is a foundational activity of effective population health management.
Patients with Medi-Cal have access to many resources that can support improved health outcomes and address social needs. These Medi-Cal resources can be another opportunity to create care coordination processes in your practice; see Figure 18 for a partial list of Medi-Cal programs that involve care coordination. As of 2023, both doula care and community health worker services are benefits of the Medi-Cal program. Doulas provide evidence-based, culturally competent (racial, ethnic, linguistic) services aimed at preventing perinatal complications and improving health outcomes for birthing. The services of community health workers (also known as Promotores/Community Health Resources) can be highly effective in helping to connect patients to resources and educational materials that are community based and aligned with a patient’s values, language and cultural needs to further health equity. The California Health Care Foundation offers an overview of the community health worker program, including potential hurdles.
Medi-Cal patients with high medical, behavioral health and/or social needs may be eligible for ECM and Community Supports (see Key Activity 21: Provide Care Management for more information on these programs).
There are also a number of Medi-Cal programs that provide services and support to Medi-Cal patients who qualify. Care coordination between the practice and these programs can result in more integrated care for eligible patients. Long-term services and supports, which are available to support individuals in the community, are examples. These include skilled nursing facility services, personal care services, self-directed personal assistance services, in-home supportive services, and home and community-based services. Figure 18 provides a high-level overview of care coordination opportunities.
FIGURE 18: EXAMPLES OF MEDI-CAL PROGRAMS OR BENEFITS THAT INVOLVE CARE COORDINATION
- Enhanced Care Management
- Community Supports
- Community Health Workers
- Doula
- Long term services and supports (LTSS)
- California Children’s Services (CCS)
Effective care coordination helps your practice to better meet the broad range of patient needs and preferences. It helps ensure that each patient’s needs and preferences are known and communicated at the right time to the right people and that this information is used to guide the delivery of safe, appropriate and effective care.
Key outcomes of care coordination are:
- Greater patient participation and satisfaction.
- Closed gaps and inequalities in access to care addressed.
- Improved quality outcomes and potential to leverage quality financial incentives.
- Decreased staff burnout and duplication of services (i.e., “let the system do the work”).
Effective care coordination helps to reduce health inequities and address social needs among different populations by better identifying and then working to address a broad range of patient needs. When care coordination is effective, the patient is at the center of care and the patient's cultural, social and health needs are incorporated into a plan of care. By identifying outside clinical supports (e.g., hospital care, specialist care) and social supports (e.g., housing, transportation and food assistance) and creating pathways for coordination, the practice promotes equity by facilitating access to these services for all patients who need them. As part of a care coordination strategy, practices should consider the growing number of “aggregator” organizations (see the “Resources” section below) that partner with community-based programs and resources centered around addressing social needs, such as housing, food and community. Many of these community-based programs are tailored for specific demographic groups and can support patients in meeting their needs in a culturally competent way.
Technology can be used to streamline and enhance care coordination. Care coordination technology tools can support care coordination activities such as registry, clinical decision support, care gap reporting, and patient outreach and engagement. See additional considerations under the “Address connectivity” section below.
Practices can use a care coordination self-assessment tool, such as those referenced in the action steps below) to determine if additional technology support would be indicated.
Registry and care gap reporting
Practices can use an analytics platform to identify patients and group patients together who have similar needs. Your practice can then tailor interventions to meet the needs of a population. For example, a practice can use data to identify those people who have not had a visit in the past year or those who are due for colon cancer screening. Data can come directly from the medical records or from claims data that is submitted to the payor.
Care coordination software: clinical decision support
Many EHRs have care coordination modules that can be used to develop assessments and care plans. Alternatively, care coordination modules can be add-ons to EHRs. Care coordination software can support assessment, referral and coordination pathways (clinical decision-making support). Using a care coordination software module, a practice can develop an assessment with questions regarding a patient’s social health needs. If answers are positive, the software can be configured to provide referral pathways and prompt care coordination activities. For example, if a patient answers “yes” to questions on food insecurity, the assessment can prompt referral to local resources such as food banks, meal programs and nutritional supports. The system can also prompt the staff to reassess progress at the next visit.
Action steps and roles
The action steps and roles outlined below provide a framework for assessing current state of care coordination, developing a strategy, implementing care coordination, and monitoring and learning as you progress.
1. Establish a “call to action” for care coordination.
Suggested team member(s) responsible: medical lead or care coordination staff or QI staff.
To achieve effective care coordination, your practice needs to see itself as a “hub” or “center” for coordination of patient care.
- While all clinicians within a patient’s support network need to collaborate, your practice should view itself as accountable for care coordination for empaneled patients and patients who have been assigned to your practice by their MCP.
- Identify a care coordination team that will be responsible for leading the evaluation, assessment and implementation of care coordination activities.
- Share with the care coordination team why care coordination is important.
- Some areas to address:
- Discuss what care coordination is.
- Discuss why care coordination benefits staff and patients.
- Review proposed framework (assess, develop strategy, implement, monitor) to develop the care coordination activity.
- Identify and share some initial projects that are directed at enhancing care coordination.
- Invite and engage staff and patients to provide input on how they think care coordination can be enhanced.
- Discuss how best to incorporate feedback from patients.
Use feedback from this activity and incorporate it into an assessment.
2. Assess your practice’s current state of care coordination activities.
Suggested team member(s) responsible: panel manager and QI lead.
Begin by asking and answering the following questions:
- What does the practice hope to achieve by implementing interventions to change the care coordination process?
- Which patient needs are the responsibility of the practice to provide (care coordination within the practice)?
- Which patient needs will need to be addressed through external referral and collaboration (care coordination with entities outside the practice)?
What resources are needed to improve the current state (data; input from care team members; input from care partners such as hospitals, specialty, behavioral health, social needs)?
Gather stakeholder input.
- Conduct interviews or surveys with patients and community members to understand their perspectives on current care coordination processes, challenges and areas for improvement.
- Conduct interviews with your care team to understand their perspectives on current care coordination processes, challenges and areas for improvement.
Analyze existing systems and processes.
- Review existing care coordination protocols, technologies and resources utilized by health centers.
- Explore how technology is currently being used to support care coordination. Then explore how technology could be harnessed to streamline care coordination, improve data sharing and/or enhance communication among clinicians.
- Review existing formal and informal linkage agreements.
- Conduct an analysis to determine patient needs not yet fully addressed by existing agreements.
- Assess data on patient outcomes, patient satisfaction and any existing QI initiatives.
- The following resources can help your practice assess its current state:
- Population Health Management Capabilities Assessment Tool (PhmCAT): sections on population-based care, social health and behavioral health.
- Care Coordination Maturity Assessment: This resource addresses multiple domains that may be impacted as care coordination activities are undertaken.
3. Develop and implement a care coordination improvement strategy.
Suggested team member(s) responsible: panel manager and QI lead.
Develop your high-level care coordination improvement strategy.
- The high-level strategy is based on the results and insights from your Care Coordination Maturity Assessment and your practice’s capacity (bandwidth).
- Establish clear objectives.
- Define specific, measurable, achievable, relevant, time-bound, inclusive and equitable (SMARTIE) goals for enhancing care coordination.
- Ensure that these goals align with the overall mission and values of your practice.
- Prioritize areas for improvement: Identify a limited set of key focus areas based on the assessment findings and your practice’s bandwidth, such as communication protocols, technology integration, staff training or patient engagement strategies.
Identify resources and infrastructure.
- As part of the implementation of the strategy, identify the resources and infrastructure needed to support care coordination at your practice.
We have included in Figure 19 below some considerations, by resource, as you develop your care coordination implementation plan (some of the resources may not apply to your practice).
FIGURE 19: CONSIDERATIONS FOR IDENTIFYING CARE COORDINATION (CC) RESOURCES
Resource |
Considerations |
|---|---|
Staff |
Dedicated time for the development, training and implementation of CC activity. Defining ongoing staffing needs. |
Internal tools |
Electronic health record modifications. Data needs and technology needed to implement CC activity. |
Process |
Development of workflows, training materials, communication plan and job descriptions. Identification of what CC activities will be the responsibility of the practice staff. |
Funding and finance |
Explore benefits such as Enhanced Care Management or community health workers, as well as financial resources that may be available through external partners, such as health plans and hospitals. |
Clinical decision-making support |
Medical staff, behavioral health and social work and patients as subject matter experts (SMEs). |
External support and data |
Information and resources required from the entity with which the clinic is coordinating (e.g., hospital, specialist, social health provider). Data exchange requirements including the new California Data Exchange Framework (DxF). |
Develop staffing for care coordination.
Determine who at your practice will be involved in care coordination. The PHMI Care Teams and Workforce Guide Resource 1: Core and Expanded Care Team Functions, Team Members and Roles provides an overview on care coordination using a care coordinator or referral manager.
- Based on the population of focus and the intervention, develop staffing requirements and any job description changes to embed care coordination into your practice.
- The responsibilities of a person/people fulfilling care coordination roles should include, at a minimum:
- Manage the referral process.
- Assist patients with transitions, such as those to and from hospitals and other institutions.
- Help patients resolve logistical, financial and/or other barriers to a successful referral.
- Link patients with community resources.
- Follow up with patients within a few days of an emergency room visit, hospital discharge or discharge from a treatment facility.
- Ensure the safe transfer of patient data.
- Track progress (referral milestones).
- Assist patients who are having difficulties.
- Schedule follow-up and specialty appointments for/with patients
- Formalize the referral coordinator role through a job description or position description. Sample referral coordinator position description.
- Provide regular training and support to care coordinator/referral coordinator or similar.
Develop or refine your policies and procedures for care coordination. At a minimum, this should include all of the following:
- Identifying patients who are eligible for care coordination.
- Defining the activities that are associated with care coordination (outreach, engagement, assessment, desired outcome).
- Managing the referral process.
- Ensuring the safe transfer of patient data.
- Tracking progress – closed loop referral.
- Identifying patients who would benefit from higher levels of care coordination, such as care management interventions like ECM (see Key Activity 21: Provide Care Management.)
Develop or refine your referral protocols.
Develop clear guidelines for when and how to make clinical referrals.
- Include criteria for urgent versus nonurgent referrals.
For each clinician your practice will be referring to:
- Identify the information, format and process the clinician requires to receive a referral.
- Share the information you will need back from the clinician (when the referral has been successfully made and/or once the service or support has been provided) to ensure continuity of care and nonduplication of services.
- Formalizing this through a written agreement or compact is a good way to ensure expectations on both sides of a referral are understood.
In working with community agencies or organizations that provide social support, the specific information that can and should be shared will depend on the service. It is important to have a mutual understanding about that information, using a written agreement where possible. At minimum, if the referral did not include a warm handoff, there should be an expectation that the practice hears back from the organization to let them know whether the patient followed up on the referral. See: Sample primary care checklist suggestions for assessing referral process.
Address connectivity. For any clinicians that you are exchanging patient data with, your practice should develop formal agreements and processes. Below are some considerations to facilitate information sharing among clinicians involved in an individual’s care:
- Integrate documentation platforms where possible and standardize how documentation is included in patient records.
- Ensure that behavioral health records are integrated into the overall EHR system to the extent permitted by law.
- Enable clinicians to access comprehensive patient information.
- Identify and assess participation in health information exchanges and/or social health information exchange systems, where feasible, to facilitate seamless sharing of patient information. These exist in some communities and will develop over time. This explainer series from the California Health Care Foundation describes the new statewide health information exchange coming into effect in 2024.
- Understand when patient consent is required to ensure compliance with privacy regulations, such as the Health Insurance Portability and Accountability Act. Include consent processes in the referral protocols.
- Set expectations about the information that should be shared and develop processes for facilitating that exchange. As data that is used in a clinical setting will likely be different than information that is shared by community agencies or social support networks, it is imperative to have clear parameters around what types of information can be exchanged between your practice and your partners.
Provide care coordination to patients.
In accordance with your care coordination policies and procedures and referral protocols, provide care coordination to patients who need it.
Embed care coordination into your practice’s daily workflow, including PVP. See Key Activity 10: Develop or Refine and Implement a Pre-Visit Planning Process.
Provide referrals to care management (See: Key Activity 21: Provide Care Management) such as ECM for patients who require more intensive support.
Discuss each referral with the patient to ensure the patient understands the reason for the referral.
Below is an example of a care coordination QI strategy.
FIGURE 20: EXAMPLE OF A CARE COORDINATION QUALITY IMPROVEMENT STRATEGY
Area of Improvement |
Goal |
Why It Is Important |
|---|---|---|
Development of registries and process to outreach to empaneled patients who have not engaged in care. |
Bring individuals into care and screen for social health needs/barriers. |
Supports increased access to preventive medical care and addresses barriers related to social health. |
Development of a closed loop referral pathway for social services when social health barriers are identified. |
Support patients in receiving services that will be beneficial to addressing social health barriers, including those that are culturally aligned and based in communities where they live. |
Health outcomes, including health equity and access, are improved when social health needs are met. |
Development of a referral pathway to specialty clinicians and the creation of a pathway to receive consult results. |
Optimize access to specialty services, including urgent referral, and ensure consultation results are available to the PCP. |
Ensures timely access for services, including urgent referrals. Receipt of consult information saves time and prevents duplication of services. |
Development of a process to follow up with patients after transitions of care, posthospitalization. |
Support optimal outcomes for patients after hospitalization and decrease the chance of rehospitalization. |
The transition from the inpatient (hospital) setting back to home often results in poor care coordination, which can lead to medication errors, repeated or incomplete diagnostic work-up and lack of clarity regarding what a patient needs after hospitalization. |
The following resource can help your practice develop your care coordination improvement strategy:
4. Monitor continuous QI of care coordination
Suggested team member(s) responsible: QI lead.
Develop both formal and informal mechanisms to obtain feedback from clinicians, staff and patients on the effectiveness of your practice’s care coordination efforts and to identify areas for improvement.
Establish key performance indicators related to care coordination. Consider using AHRQ’s Care Coordination Quality Measures for Primary Care (CCQM-PC). Your performance indicators will vary based upon your improvement strategy and the needs of patients, but they may include metrics such as:
- Number of assigned patients engaged in care.
- Number of individuals with hypertension whose blood pressure is controlled.
- Percentage of closed loop referrals by referral entity. Monitor and analyze metrics to gauge the effectiveness of your internal systems and how well each referral partner is promoting coordination and collaboration.
Continue to build relationships with clinicians and community support agencies that are available to provide services to patients.
Consider developing and using a care coordination variance report. Here is a sample patient care coordination variance report.
Implementation tips
- An interoperable referral management system can help practices streamline the intake process, communicate with other clinicians and social service agencies, track the status and outcomes of referrals, and ensure that patients receive the appropriate level of care and support.
- Leverage community health information exchanges to gain access to admission, discharge and transfer information. Absent being able to access a health information exchange, establish relationships with your local hospitals to be able to gain daily notification of your patients being discharged.
Going Deeper Key Activities
These are more advanced activities that build off the foundational activities and that help ensure your practice can achieve equitable improvement in your patients’ management of chronic diseases, including diabetes and hypertension.
KEY ACTIVITY #19:
Provide Group Visits for Chronic Care Management
This key activity involves all seven elements of person-centered population-based care: operationalize clinical guidelines; proactive patient outreach and engagement; pre-visit planning and care gap reduction; behavioral health integration.
Overview
Group visits involve a healthcare team facilitating an interactive process of care delivery. A group visit allows patients to learn from each other while being supported and empowered with information and encouraged to make informed healthcare decisions by the care team.
A group visit requires coordination and advanced planning. It typically involves a group of eight to 15 patients, all of whom share a common condition. Patients are able to express a primary question or issue they hope to get addressed during their visit. The lead clinician will often provide general coaching and answer questions. Once a clinician has completed their initial portion of the visit, another care team member can take over the group visit, providing engagement, education and counseling. For example:
- A pharmacist might go over common medications and challenges patients face with their medications.
- A nutritionist can speak to dietary counseling and meal preparation for a healthy lifestyle.
- A behaviorist might address mindfulness practices.
While the general education time is underway, a clinician can see each patient individually and address specific questions or issues. While a face-to-face interaction with a medical clinician is necessary to bill for a group visit, in practice, different team members – such as a behaviorist, pharmacist or nurse – can and do take responsibility for developing and facilitating the group visit.
In a 90-minute visit, a clinician can see every patient individually while the patients benefit from the multidisciplinary care visit and peer learning and support. This visit model is more productive (even with no-shows) and frees up many individual slots for higher-intensity visits of other patients, thus improving access for the broader panel of patients.
Group visits are a powerful model to foster peer support and shared learning to help build patient self-efficacy. Peer support encourages patients and provides the opportunity to share lessons learned from life experience.
Group visits can be inclusive and offered to all patients. They break down social barriers that contribute to health inequities. Group visits also can result in new social bonds that result in strategies to address social needs (such as transportation issues through ride sharing). They help empower those who have not been able to develop the health literacy or self-activation skills necessary to be confident in managing their chronic condition.
Action steps and roles
1. Determine your group visit condition.
Suggested team member(s) responsible: clinical leadership.
Determine which condition you want to be the focus of your group visit. It is best to have group visits involving people with similar conditions who can share their own experiences and best practices in how they are adapting to their chronic condition.
2. Plan for group visits.
Suggested team member(s) responsible: LVN or MA.
Plan your group visit with a timed agenda outlining what will happen during the group visit (e.g., the educational component, nutrition counseling, when the clinician will see patients individually, any testing required during the visit, etc.). The Serve the People Community Health Center created a toolkit that provides guidance for planning and resourcing diabetes group medical visits, as well as flowsheets with roles and responsibilities outlined.
Pull charts three to five days before the group visit. As agreed upon by the team, perform chart review to identify specific patient needs to be accommodated and to identify gaps in care. Confirm whether you will have extended members of the care team participate, and recruit and prepare them for their roles (e.g., pharmacist, nutritionist, social worker, etc.). Staff should also prepare materials required for the visit (i.e., labels, education materials, etc.)
Remind the primary care clinician about the upcoming group visit. Ensure the room housing the group visit is ready and set up with all materials needed for the group visits. Community Medical Centers developed handouts for their group medical visits that address A1c, blood pressure, healthy eating and goal setting.
3. Determine how to bill for group visits.
Suggested team member(s) responsible: administration and billing staff.
Complete billing information as needed. Group visits should be billed as individual encounters as long as patients are seen one-on-one by the billing clinician during that visit. The level of complexity of the visit should include all services provided in this interdisciplinary shared medical appointment.
Billing is a common challenge for group visits. Keep in mind that during a group visit, the clinician sees every patient hands-on; therefore, this should be documented as a medical office visit and should follow traditional documentation for an individual visit. It is important to note that the physician's contact with the patient is longer than most routine office visits.
Since many other activities are happening during the group visit, you can add the appropriate modifiers to enable you to code at the correct level of intensity. For UDS purposes, the visit can be counted as an individual encounter as long as it meets the traditional criteria (each patient is seen one-on-one and the clinician is using individual clinical decision-making). See the UDS resources for more information.
4. Recruit patients for your pilot.
Suggested team member(s) responsible: clinicians and care team members.
Identify candidates and register them for a group visit after determining their level of interest. They should be identified based upon set criteria (i.e., current treatment adherence, care gap needs, treatment complexity, etc.).
5. Plan the visit with a clear understanding of the roles.
Suggested team member(s) responsible: Nursing Staff/Medical Providers
Circulate in the room during break, performing vital signs and identifying patients who need individual attention.
Provide a brief educational module and lead a discussion. An example would be for the physician/advanced practice professional to provide a five-minute brief education on what diabetes is and why complications arise. This might include visuals to help patients process the information. This would be followed up with a question-and-answer period where all patients benefit from questions from others.
During break, review individual needs and make one-on-one individual appointments for after the visit.
6. Evaluate and scale group visits.
Suggested team member(s) responsible: care team members.
A natural progression of group visits is to start with a single condition (such as diabetes) and an early adopter champion and then progressively scale your group visit model across your organization to be available for all eligible patients with that condition. Starting with a smaller group allows for challenges to be worked out before a larger rollout. This is not an insignificant challenge for health centers as it requires constant refreshing of the curriculum and updating information based on the latest evidence base.
A future activity is to expand your group visit model to other conditions, using what you have learned from your early pilots and scaling.
An advanced model for group visits incorporates your patients into the design and execution of the group visits. An example might be to include a patient with expertise in exercise and wellness as a future speaker for a module in a group visit.
Examples
In this quick video from a Canadian practice holding group visits for maternal health, the patients are empowered to do their own vitals. In this approach, an alternative clinician conducts the educational modules.
This alternative workflow from the University of Virginia focuses on women with cardiovascular disease.
The Group Visits Improve Diabetes Self-Management case study describes the implementation of diabetic group visits and the lessons learned at the East Valley Community Health Center.
Implementation tips
- Understand that group visits are not for every patient, condition or clinician. Like all new innovations, there will always be a small cohort that does not favor the group visit, and that is their prerogative. Some patients will not like group visits. Some clinicians are not suited for group visits. However, for certain populations, this visit model is highly effective.
- At the beginning of a group visit, remind participants of ground rules on confidentiality and respect.
- Encourage patient engagement during the group visit. Patients often comment that the peer support and what they learned from others were as valuable as the interaction with the care team.
- Inventory your staff to see if you have team members who have skills outside of work that can be leveraged for your group visits (e.g., personal trainers, yoga instructors, etc.).
- Consider teaching patients to do their own vital signs at the beginning of the group visits, thus positioning them to continue to do so at home and to take advantage of evolving remote monitoring technologies.
- Consider practical learning opportunities for patients, such as going to a grocery store to learn about reading nutrition labels and effective shopping techniques.
- Fully leverage your care team so that all documentation is completed by the end of the visit; this would relieve all from the burden of having to do documentation later.
- Consider using alternative staff (e.g., volunteers, AmeriCorps) to staff visits.
Evidence base for this activity
- Beck A., Scott J., Williams P. Robertson B., Jackson D., Gade G., Cowan P. A randomized trial of group outpatient visits for chronically ill elderly HMO members: The cooperative healthcare clinic. Journal of the American Geriatric Society 1997: 45;543-549.
- Masley S., Solokoff J., Hawes C. Planning for group visits with high-risk patients. Family Practice Management 2000; 7:33-38.
- McKenzie M., Scott J. “Cooperative healthcare clinics deliver primary care in a group setting.” Guide to Managed Care Strategies, Burns J & Northrup LM, Eds. New York: Faulkner and Gray, 1998.Noffsinger EB, Scott JC. Understanding today’s group visit models. Group Practice Journal 2000:48(2):46-8, 50, 52-4, 56-8.
- Sadur CN, Moline N., Costa M., Michalik D., Mendlowitz D., Roller S., Watson R., Swain B.E., Selby J.V., Javorski W.C. Diabetes management in a health maintenance organization. Efficacy of care management using cluster visits. Diabetes Care. 1999 Dec; 22(12):2011-7.
- Scott J., Robertson B. Kaiser Colorado’s cooperative healthcare clinic: A group approach to patient care. Managed Care Quarterly 1996:4(3);41-45.
- Scott J.C., Gade G., McKenzie M., Venohr I. Cooperative healthcare clinics: A group approach to individual care. Geriatrics 1998:53(5);68-81.
- Terry K. Should doctors see patients in group sessions? Medical Economics January 13, 1997;74-95.
- Thompson E. The power of group visits. Modern Healthcare June 5, 2000.
- Beck A., Scott J., Williams P. Robertson B., Jackson D., Gade G., Cowan P. A randomized trial of group outpatient visits for chronically ill elderly HMO members: The cooperative healthcare clinic. Journal of the American Geriatric Society 1997: 45;543-549.
KEY ACTIVITY #20:
Strengthen Community Partnerships
This key activity involves all seven elements of person-centered population-based care: proactive patient outreach and engagement; care coordination; address social needs.
Overview
Strengthening partnerships with other organizations – such as pharmacies, recreation centers, senior centers, local government, community based organizations (CBOs), etc. – that share the practice’s vision and goals for its patient population enables the practice to provide more holistic care to patients and leverage many of the strengths and resources available in the community. These partners provide various services and programs to the community, such as education, housing, food, transportation, employment and social support.
This activity provides considerations and tips for strengthening partnerships; although note that deep engagement in this work can require significant resources from your practice.
Many community-based organizations have a deep understanding of the needs and preferences of the specific subpopulations, as well as the resources and challenges that exist in the local context. They can support outreach and health literacy efforts, participate in collaborative design by providing insight around a particular patient population, and provide resources and support for patients.
Building and strengthening relationships with community-based partners can extend the reach and impact of practices by facilitating patient access to services that the practice is unable to provide directly. Through partnerships with organizations that provide housing supports, nutrition assistance, transportation and other social health supports, practices can play an active role in helping to address the social needs of their patients. The PHMI Equity Framework and Approach should inform partnership development to ensure the work of partnership building is prioritizing community groups that experience injustice and structural violence.
An additional aspect of whole-person healthcare is greater coordination and collaboration with existing community mental health supports. As with community partnerships, integration rests on enhanced relationships between organizations. This means going beyond simply being aware of community mental health organizations as receiving referral sites to reaching out to better understand the barriers to information sharing as well as community mental health agencies’ capacities and expertise.
Action steps and roles
1. Start by understanding the resources and partnerships available through Medi-Cal.
Suggested team member(s) responsible: clinic operations and leadership staff who will liaise with community partners.
Resources include supports that are available to all Medi-Cal patients (such as transportation to medical appointments) as well Medi-Cal Community Supports for eligible individuals with higher levels of social needs. The following is a list of social support resources that are available to Medi-Cal patients when eligibility criteria are met:
- Transportation to medical and other Medi-Cal-covered appointments.
- In-home supportive services – personal home care assistance for those who qualify.
- Community-based adult services – day programs outside the home for individuals who need assistance with activities of daily living.
For individuals with the highest needs, the14 Medi-Cal Community Supports are:
- Housing transition navigation services.
- Housing deposits.
- Housing tenancy and sustaining services.
- Short-term posthospitalization housing.
- Recuperative care (medical respite).
- Day habilitation programs.
- Caregiver respite services.
- Nursing facility transition/diversion to assisted living facilities.
- Community transition services/nursing facility transition to a home.
- Personal care and homemaker services.
- Environmental accessibility adaptations (home modifications).
- Medically supportive food/meals/medically tailored meals.
- Sobering centers.
- Asthma remediation.
Contact the provider services department of your Medi-Cal Managed Care Plan to learn more about the providers of these services and specific providers in your area. With a list of contracted community-based organizations, your practice can start to build relationships and support ongoing social needs for your patients.
For an overview of Community Supports in the state, DHCS has provided information about the current state of Enhanced Care Management and Community Supports in the Community Supports Year 1 Summary and the Enhanced Care Management Year 1 Summary.
2. Complete an environmental scan to understand who your patients identify as trusted messengers and resources in their community.
Suggested team member(s) responsible: health center leadership, community health workers and social work staff.
This can be completed by interviewing patients and families and by confirming existing partner relationships. This can be completed with the assistance of community health workers. After that, a stakeholder map and community profile of key current and prospective partners can be developed.
Practices should also partner with hospitals, community behavioral health centers, public health agencies and other key stakeholders to refine your community needs assessments.
3. Convene partners as a work group to develop strategies and interventions to address health-related social needs.
Suggested team member(s) responsible: health center leadership.
In some cases, your practice may serve as a convener, bringing partners together for collaboration to avoid relying on individual relationships with external organizations. Be clear on your “asks and offers” to ensure the relationship will be mutually beneficial.
Develop a shared aim statement with your partners as to why this work is important and your vision of what you hope to achieve. Following the aim statement, formalize your structure and system of collaboration and accountability to ensure progress. This may take the form of ongoing pacing of meetings on a regular basis rather than relying on transactional relationships. To ensure proper understanding of expectations, roles and commitments, memorandums of understanding should be developed.
4. Collaborate with your partners to develop a shared set of strategies on a community approach to address health-related social needs.
Suggested team member(s) responsible: health center leadership.
The practice should benchmark and collate approaches to identify potential interventions for addressing health-related social needs. CalAIM resources should be leveraged as part of your intervention plans.
A driver diagram should be developed to guide your efforts and to set priorities.
5. Collaborate with partners to collaboratively design and execute interventions and approaches to address health-related social needs.
Suggested team member(s) responsible: health center leadership.
Use workflow mapping tools, swim lane diagrams and checklists that clarify roles and plan initiatives. This allows the practice to develop clear action plans that clarify leaders of intervention strategies, timetables, and measures of progress and success.
Going deeper in strengthening partnerships: Addressing community needs requires sustainable and effective partnerships over time. A future activity includes your organization working with other community partners in an ongoing forum to address community needs. This often involves the health center as a backbone organization supporting a local collaboration governance structure for shared prioritization and action planning.
On the horizon in strengthening partnerships: A mature partnership system in a health center includes assessing the effectiveness of the partnerships and finding ways to continuously ensure alignment so that partnership remains a positive force for all participants. When possible, making adjustments that strengthen the partnerships can be explored (such as improving data sharing, pooling resources to increase leverage in the community, etc.).
Implementation tips
- Health centers are very adept at developing relationships in the community, but often they are challenged in nurturing partnerships. A partnership starts with relationships, moves beyond referral for resources or support, and results in co-ownership for addressing community challenges.
- Be clear on being able to have something to offer when approaching a prospective partner. Nurture the relationships and avoid becoming transactional, ensuring the partnership has value for all parties and helps others fulfill their mission.
- Seek to understand your partner’s needs for results, data and reporting. Explore how the partnership can help your partner meet a need or address a pain point in their core business mission.
- Learn what is in place for your county through the Medi-Cal program and your managed care plans. If resources are not available, explore technologies that facilitate community referrals, such as findhelp.org and Unite Us’ cross-sector collaboration software.
Resources
KEY ACTIVITY #21:
Provide Care Management
This key activity involves all seven elements of person-centered population-based care: operationalize clinical guidelines; proactive patient outreach and engagement; care coordination; behavioral health integration; address social needs.
Overview
What is care management? How does it differ from care coordination?
Led by a care manager (a licensed clinician or a non-licensed trained individual), care management is an intervention intended to support the highest-need individuals within your practice. The services are more focused, require the development of a person-centered care plan, and are of higher intensity than care coordination services. A patient must consent to participate in care management activities. A care manager works directly with the patient and multidisciplinary care team members to identify, plan and implement person-centered goals and care. The care manager supports the individual in identifying and coordinating resources and referrals as well as supporting self-management activities to attain optimal wellness.
Care management provides a higher level of support to individuals who have medical, behavioral health and/or social needs that impact their ability to access appropriate levels of care. Individuals may be receiving frequent emergency room and hospital care that could be avoided with care management activities, and/or patients may have significant social barriers (housing, food, substance use) that prevent them from accessing preventive and wellness care.
As part of care management, the patient’s medical, behavioral health and social health needs are directly addressed as part of their health assessment and prioritized according to the patient's goals. For example, supporting the patient's concerns around securing stable housing may be a first step to achieving better health. Addressing health-related social needs helps in reducing health inequities among different populations. Individuals with lower socioeconomic status or limited access to resources can be provided with resources to support these areas.
What type of patients are eligible for care management?
Individuals eligible for care management have high levels of need in one or more of the domains of medical, social or behavioral health. Some examples of populations who may be eligible for care management include:
- Individuals with complex medical needs (also known as complex care management).
- Example: a patient with congestive heart failure and advanced kidney disease with a history of frequent hospitalizations for shortness of breath.
- Goal of care management: support optimal diet and medication management to minimize hospitalization; address social needs that may impact the patient’s ability to manage their conditions, such as housing stability, food security, etc.
- Individuals who require intensive support after hospital discharge (care transitions).
- Example: a patient who had a stroke resulting in left-sided weakness and mobility issues. They will require additional support – including home nursing, physical therapy/occupational therapy, medical equipment and medication monitoring – as they make the transition to the home environment.
- Goal of care management: coordinate medications, medical equipment and follow-up care to support optimal recovery and minimize risk of rehospitalization.
CalAIM: ECM and Community Supports
In California, Medi-Cal beneficiaries who have high care management needs may be eligible for a Medi-Cal benefit known as Enhanced Care Management or ECM. ECM can be provided to eligible Medi-Cal beneficiaries at risk of poor outcomes due to high levels of medical, social and behavioral health needs. ECM delivers person-centered, trauma-informed care management services. Patients can also access additional services known as Community Supports to help achieve their medical and social health goals.
DHCS ECM and Community Supports[39] are foundational parts of the transformation of Medi-Cal, which focused on:
- Breaking down the traditional walls of healthcare, extending beyond hospitals and healthcare settings into communities.
- Introducing a better way to coordinate care.
- Providing high-need patients with in-person care management where they live.
If your practice has a lot of patients who are eligible for ECM (based on descriptions below), you can contact your Medi-Cal managed care plan (MCP). Your MCP can provide you with details on patient eligibility and the requirements needed to provide ECM services to your patients. Some clinics also provide Community Supports services depending on their patient population.
ECM is available to specific groups of Medi-Cal patients (called “ECM Populations of Focus”):[40]
- Adults, unaccompanied youth and children, and families experiencing homelessness.
- Adults, youth and children who are at risk for avoidable hospital or emergency department care.
- Adults, youth and children with serious mental health and/or Substance Use Disorder needs.
- Adults living in the community and at risk for long-term care institutionalization.
- Adult nursing facility residents transitioning to the community.
- Children and youth enrolled in California Children’s Services or its Whole Child Model with additional needs beyond their California Children’s Services condition(s).
- Children and youth involved in child welfare (foster care).
- Adults and youth who are transitioning from incarceration.
- Pregnant and postpartum individuals; birth equity population of focus (starting in 2024).
Medi-Cal patients can also be connected to Community Supports services to help address their health-related social needs, such as access to healthy foods or safe housing to help with recovery from an illness. If your clinic wants to provide Community Supports, contact your Medi-Cal managed care plan for information. Available Community Support Services include:
- Housing transition navigation services.
- Housing deposits.
- Housing tenancy and sustaining services.
- Short-term posthospitalization housing.
- Recuperative care (medical respite).
- Day habilitation programs.
- Caregiver respite services.
- Personal care and homemaker services.
- Nursing facility transition/diversion to assisted living facilities.
- Community transition services/nursing facility transition to a home.
- Environmental accessibility adaptations (home modifications).
- Medically tailored meals/medically supportive food.
- Sobering centers.
- Asthma remediation.
How does an eligible individual get connected to ECM and Community Supports services?
The Medi-Cal Managed Care health plans are responsible for identifying their patients who are candidates for ECM and meet eligibility requirements. In addition, practices, clinicians and community-based organizations have the ability to refer patients for ECM services. Community-based organizations, such as homeless services clinicians, are a particularly valuable source of referrals into ECM, as they often have trusted relationships with individuals who may not have sought or received medical care and are therefore not “known” to the MCP because they have had little or no utilization of healthcare services.
How do we refer a patient who we think would benefit from ECM?
If you have a patient who may be a candidate for ECM or Community Supports services, you should contact the Medi-Cal managed care plan to inquire about services available through the patient’s health plan.
Action steps and roles
How can we provide care management services, including ECM services, in our practice?
Community practices are often well situated to provide care management services as they are the site where patients seek or can be connected to care. Clinics may decide that they want to provide care management services, including ECM services. The following resources can help assess your capacity to provide care management services within your clinic structure.
Care management in primary care
This resource from AHRQ is a helpful guide when considering implementing a care management program. It addresses the following areas:
- What is care management and why would my practice want it?
- Selecting the right care manager and clarifying the care manager role.
- Training the care manager and practice team.
- Structuring care management.
- Implementation and sustainability issues: getting care management started and making it continue to work well.
- Resources.
- Data collection, management and analytics.
- Paying for care management.
- Evaluation: How is your care management program working?
Care management for complex populations
A resource on starting a care management program for individuals with multiple medical, behavioral health and social needs is available from the Camden Coalition. This resource addresses the following areas:
- Program design – tools to support the understanding and identification of a complex care population, plan a care model and workflow, and anticipate legal/business needs.
- Program operations – tools to support the implementation of a complex care model, including triage, outreach, engagement, intake and clinical support.
- Data and process improvement – tools to support metric identification, data collection and analysis, and process improvement.
- Team and leadership development – tools to support the recruitment, training and management of a complex care team.
- Community mapping and collaboration – tools to support multisector and community coordination.
- Communication and growth of success – tools to support broad communication and program scaling.
Care transitions
This Care Transitions Toolkit from the Indiana Hospital Association focuses on processes to support care management for individuals transitioning between healthcare settings.
ECM services
This Enhanced Care Management Provider Toolkit from DHCS provides a detailed description of the services that are required to become an ECM clinician. In this guide, the requirements of ECM clinicians are outlined in detail.
FIGURE 21: EXAMPLE OF HOW AN EHR CAN ASSIST WITH CARE MANAGEMENT
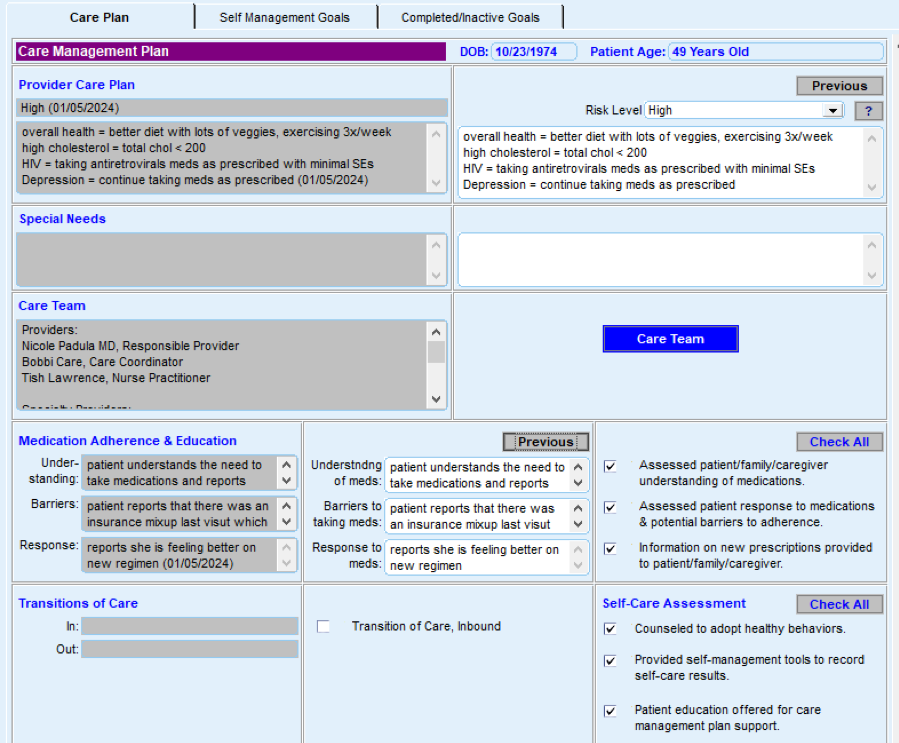
Resources
Evidence base for this activity
- Chuang E, Pourat N, Haley LA, O’Masta B, Albertson E, Lu C. Integrating Health And Human Services In California’s Whole Person Care Medicaid 1115 Waiver Demonstration. Health Affairs. 2020 Apr 1;39(4):639–48.
- Tomoaia-Cotisel A, Farrell TW, Solberg LI, Berry CA, Calman NS, Cronholm PF, et al. Implementation of Care Management: An Analysis of Recent AHRQ Research. Medical Care Research and Review. 2016 Oct 23;75(1):46–65.
KEY ACTIVITY #22:
Continue to Develop Referral Relationships and Pathways
This key activity involves all seven elements of person-centered population-based care: operationalize clinical guidelines; proactive patient outreach and engagement; care coordination; behavioral health integration; address social needs.
Overview
Delivery of primary healthcare encompasses not only preventive services and coordination of medical and behavioral healthcare but also referrals for social supports, dental care and other needs of patients, such as weight management or parenting programs. As a result, coordination of care is more complex and often involves referrals outside the practice structure. Examples include referrals from the practice to a clinician, such as medical specialty clinicians, or behavioral health and social service providers, such as the Supplemental Nutrition Program for Women, Infants, and Children; CalFRESH; CalEarn; the Employment Development Department for paid family leave; or to a program that will support health and well-being. A referral network also includes acute and subacute facilities, such as hospitals, emergency departments and residential treatment facilities where a patient may receive treatment and the outcome of treatment is necessary for the ongoing care of the patient in the practice.
This activity addresses common steps that your practice can take to optimize both the referral pathways and outcomes. The practice of closed loop referrals, in which there is a feedback mechanism to ensure that a referral made by one provider to another is completed and followed up appropriately, leads to greater patient and provider satisfaction. This activity builds on an inventory of existing referral services outside the clinic and identifies steps that can be taken to support the systematic management of the referral process.
When a patient requires a referral to obtain needed services outside the clinic, the process is a point of vulnerability. A significant percentage of specialty referrals are not completed, in part due to missing information, misguided referrals and faulty communications.[41][42] If a referral is not completed, patients may not receive needed services, which can lead to decreased quality of care, decreased patient and clinician satisfaction, and ultimately poorer health outcomes.[43] The National Committee for Quality Assurance (NCQA) recognizes the importance of referral networks and their management as a core component of Patient Centered Medical Home activities.[44] Building a reliable network of service partners and processes to provide information necessary to inform referrals as well as having mechanisms to track referral results are important parts of providing coordinated care that is person centered.
A contributor to inequity in health outcomes is unequal access to specialty services and resources to help patients with their condition.[45] The heart of this activity is to empower both the care team and patients through development and maintenance of a robust process to help patients access medical, behavioral health and community resources.
Many factors can impact whether or not a patient accesses a referral, including language, culture and lack of understanding of why referral is being requested. Lack of understanding of why a referral is being sought is often a barrier for patients to follow up with a referral, particularly if a patient is not experiencing symptoms.
When appropriate, referrals for social needs and to community health programs can help address barriers, including those around transportation, language, and basic needs of food and housing stability, all of which are associated with poorer health outcomes. Action steps and roles
Action steps and roles
1. Identify types of referral partners that your practice needs and gaps in resource availability.
- Some examples to consider: high-volume specialties such as ophthalmology, podiatry, dermatology, social services clinicians, substance use clinicians.
- In areas where you have gaps in referral clinicians, telehealth services may be an option. For further information on telehealth services – including e-consult and synchronous, asynchronous and e-visits – contact your MCP and/or refer to the Telehealth Reimbursement Guide for California (Pages 14 to 16). Referral processes and tracking are also important to establish for telehealth as well as in-person services.
- Note that there is a shortage of behavioral health clinicians in many parts of California. As you continue to expand your network of off-site behavioral health clinicians to meet pressing behavioral health needs, also consider behavioral health integration strategies, including expanding your practice’s capacity for providing integrated behavioral health services. See the PHMI People with Behavioral Health Conditions Guide for more about deepening and expanding integrated care.
- Work with the care teams for patients with diabetes and hypertension to identify gaps in referral resources that could enhance implementation of evidence-based care.
- Use social health screening results that have been disaggregated by REAL and SOGI alongside patient/family feedback to identify unmet needs for which resource relationships have not been established.
2. Assess what tools would be beneficial for the core elements of your referral process.
Examples include: (see resources below)
- Referral request form:
- Determine what information is required for the clinician who is receiving the referral. Information may include the requested service; timing (urgent vs. standard); minimum necessary information, such as patient contact information and applicable demographics; and appropriate clinical and social support questions.
- Referral tracking spreadsheet or software:
- Information in a tracking system can include date of referral, appointment status and whether follow-up is needed. Reach out to your Medi-Cal MCPs as you are developing referral tracking processes. The MCPs are required to show that Medi-Cal patients are being connected to the services that they are eligible for and referred to; this includes preventive services, specialty services and social services. The MCP may be a good resource for tools, such as those needed for tracking and reporting.
- Referral workflow diagram:
- A visual representation or workflow diagram can support staff in the referral process. The Institute for Healthcare Improvement’s Closing the Loop: A Guide to Safer Ambulatory Referrals in the EHR Era provides a visual nine-step closed loop referral process for specialty referrals as well as suggestions for improving the process.
3. Assess what tools would be beneficial in enhancing and tracking your referral process.
- Referral guidelines:
- For social services, positive responses to screening questions/tools may be the prompt for referral. Other types of referrals may be optimized by having documented referral guidelines, such as information needed by a specialty clinician in order to best answer a referral question.
- Communication templates:
- For high-volume or frequent referral types, a standardized template for communication between the clinic and referral staff can help ensure that essential information is conveyed efficiently. Examples may include referral letters, progress notes and post-visit summaries of plan of care.
- Patient education materials (develop in conjunction with referral network):
- Educational materials and resources for patients that explain the referral process and what to expect can enhance patient understanding and support referral completion. In addition, consider training MAs as well as any dedicated care coordination staff in evidence-based communication techniques, such as teach-back or motivational interviewing to leverage team-based care in supporting the patient to follow through with the referral after the visit.
4. Develop approaches to fill resource gaps.
Suggested team member(s) responsible: care team.
- Outreach to your Managed Care Plan (MCP) to understand what resources are available. MCPs are required to have online clinician directories that include specialists, which can be a resource used by a clinic to help find contracted specialists near the patient's home. In addition to comprehensive networks of over a dozen core specialty clinicians and information on behavioral health and substance use resources, many MCPs are building links to access community-based resources in addition to the 14 Medi-Cal Community Supports through referral platforms that act as a hub to coordinate social needs for patients.
- Identify external clinicians and community resources that can serve as partners in care, and use the established referral process to fill gaps in care they can address.
- Meet/schedule time with high-volume clinicians, including community-based organizations, to develop a mutual understanding of the goals of referrals and opportunities for development of a shared process (e.g., referral form).
- The American Academy of Pediatrics offers a sample tool to develop a resource list.
5. Regularly review and update the referral processes and network.
Suggested team member(s) responsible: clinic leadership.
- As new patient needs are identified, use that opportunity to identify potential resources and expand the referral network. If practices have trouble accessing a contracted specialist for their patient because of overly long wait times or because the specialist may not be accepting new patients, the MCP is required to approve an out-of-network referral to a specialist who is more available.
- On a periodic basis, review referral tracking reports to identify referral resources that are used most frequently, and use that information to reinforce the relationships and provide feedback on value.
- Review referral tracking reports to identify resources for which loop closure is lacking or from whom required information is not being received on a regular basis. Outreach to these organizations to reinforce expectations, or if necessary, identify a replacement resource for the network.
- For going deeper in tracking QI metrics, practices can develop metrics to assess the effectiveness of the referral network. This might include tracking referral completion rates, patient satisfaction and time from referral to specialist appointment.
Resources
KEY ACTIVITY #23:
Strengthen a Culture of Equity
This activity builds off of Key Activity 4: Use a Systematic Approach to Decrease Inequities Within the Population of Focus to provide strategies and in-depth resources that can help you create or strengthen a culture of equity in your practice. The PHMI Equity Framework and Approach emphasizes that achieving long-term and sustainable improvements to health and racial equity for patients and the broader ecosystem requires a transformational shift at the organizational level. The following strategies can help practices strengthen a culture of equity:
- Demonstrate senior leadership ownership for and commitment to improving health equity.
- Understand and address internalized, personally mediated and institutionalized racism.
- This should include ongoing learning and development activities on the full range of health equity topics (e.g., anti-bias, structural racism, race-based algorithms).
- Build organizational capacity to support efforts to improve health equity.
- Establish practices and policies to promote workforce diversity and provide culturally and linguistically appropriate care.
- Support policy efforts to eliminate inequities driven by health-related social needs.
This can take the form of joining advocacy efforts or participating in benefits created by recent policy reforms, such as connecting patients with Medi-Cal Community Supports for housing or medically tailored meals. See Key Activity 17: Use Social Needs Screening to Inform Patient Treatment Plans for a discussion on social needs.
Resources
On the Horizon Key Activities
Additional activities, including ideas worthy of testing that include the latest ideas and thinking on management of chronic diseases, including diabetes and hypertension.
KEY ACTIVITY #24:
Develop System to Provide Remote Monitoring
This key activity involves all seven elements of person-centered population-based care: operationalize clinical guidelines; proactive patient outreach and engagement; pre-visit planning and care gap reduction; care coordination.
Overview
Remote patient monitoring (RPM) is an innovation that allows for regular updates from patients to their clinician in order to real-time updates. It also allows clinicians to monitor the health and well-being of patients outside of a traditional clinic setting. RPM allows for a closer monitoring of patient’s conditions through regular updates, which can improve overall patient care. RPM devices typically include, but are not limited to:
- Blood pressure cuff.
- Weight scale.
- Thermometer.
- Glucometer.
- Pulse oximeter.
- ECG.
This activity provides an overview of infrastructure and processes required by practices to develop and implement remote patient monitoring programs.
RPM expands the reach of clinicians beyond a traditional clinic setting, which also improves the quality and consistency of care provided to patients.
Due to the geography of the location that the practice services, RPM may prove to be a valuable asset for patients who are unable to reach the clinic for regular monitoring.
RPM improves the equity of care provided by reducing unnecessary barriers to care while also providing real-time feedback to the patient and clinician regarding current health status. RPM also gives the ability to provide continuous data over time, rather than a quick snapshot during an in-person visit. This intervention also helps to improve the health literacy of patients and invites them to be a partner in their care.
RPM assists clinics in addressing social needs by removing potential barriers to accessing care in a traditional setting, such as lack of transportation or distance to the clinic. By making care more accessible, families and caregivers would be better able to monitor their current health status regularly while also receiving feedback from their clinician.
Action steps and roles
1. Determine which types of capabilities are most important for RPM devices.
Suggested team member(s) responsible: quality improvement staff, EHR specialist (or equivalent), medical director and practice administration.
When purchasing RPM devices, determine which types (if any) are compatible with your chosen EHR. This should allow information to be transcribed directly into the EHR. It is also an option to contract with an RPM company, which can assist with developing infrastructure.
2. Determine clinical protocols for determining if an RPM device is appropriate for the patients’ care.
Suggested team member(s) responsible: medical director (or equivalent) and quality improvement staff.
These protocols should be based upon clinical guidelines for diabetes and hypertension.
3. Determine how to properly code for RPM and train clinicians on how to execute proper billing practices.
Suggested team member(s) responsible: billing office and practice administration.
4. Train clinical staff and/or designate a staff member for each clinician to assist patients with setting up and linking RPM devices to the EHR.
Suggested team member(s) responsible: Quality Improvement staff and EHR specialist (or equivalent).
5. Provide the patient with instructions for how often to use the device to obtain the respective diagnostic and how to properly utilize the RPM device.
Suggested team member(s) responsible: medical staff.
Assist the patient with linking their RPM with the EHR to ensure a transfer of information.
The American Medical Association maintains a list of clinically validated blood pressure monitoring devices (see the article to access the list).
6. Assist the patient with understanding certain threshold diagnostics that they should be mindful of, which may warrant medical intervention.
Suggested team member(s) responsible: medical staff.
If practices identify that a patient has a diagnostic that warrants medical intervention, they should reach out to the patient to engage them in appropriate care. Such diagnostics may include, but are not limited to, critically high blood pressures, critically high glucose readings, etc.
7. Designate staff to troubleshoot and assist with RPM-related challenges.
Suggested team member(s) responsible: Quality Improvement staff, EHR specialist (or equivalent) and practice administration.
This can include staff who monitor outputs from remote monitoring to ensure threshold triggers are acted upon (such as high glucose or blood pressure).
8. Considerations for high-risk patients.
Suggested team member(s) responsible: core care team members, care coordinators and navigators, and community health workers.
An alternative that may be available for high-risk patients is to have a community care team, including a nurse and community health worker, that is able to go to the patient’s home on a regular basis and can assist with diagnostics.
An example is Neighborhood Healthcare, which did what many healthcare organizations did during the COVID-19 pandemic – it quickly pivoted to telemedicine. However, some of its ailing low-income patients lacked the technology or digital skills needed for virtual care, so Neighborhood Healthcare decided to bring it to them. This case study outlines how Neighborhood Healthcare accomplished this.
Example workflow
CCI’s RPM clinic workflow journey map: This is a collection of workflows from community health clinics in California that expanded their use of RPM for blood pressure measurements.
Evidence base for this activity
- Tucker KL, Sheppard JP, Stevens R, Bosworth HB, Bove A, Bray EP, et al. Self-monitoring of blood pressure in hypertension: A systematic review and individual patient data meta-analysis. Rahimi K, editor. PLOS Medicine. 2017 Sep 19;14(9):e1002389.
Appendices
APPENDIX A:
Sample Idealized System Diagram
WEAVING YOUR MEASUREMENT STRATEGY AND LEARNING SYSTEM INTO PRACTICE OPERATIONS
The below graphic provides an example to visualize the flow of information between a practice’s measurement strategy and actions at the practice and care team levels, including how to use the information for continual learning and improvement.
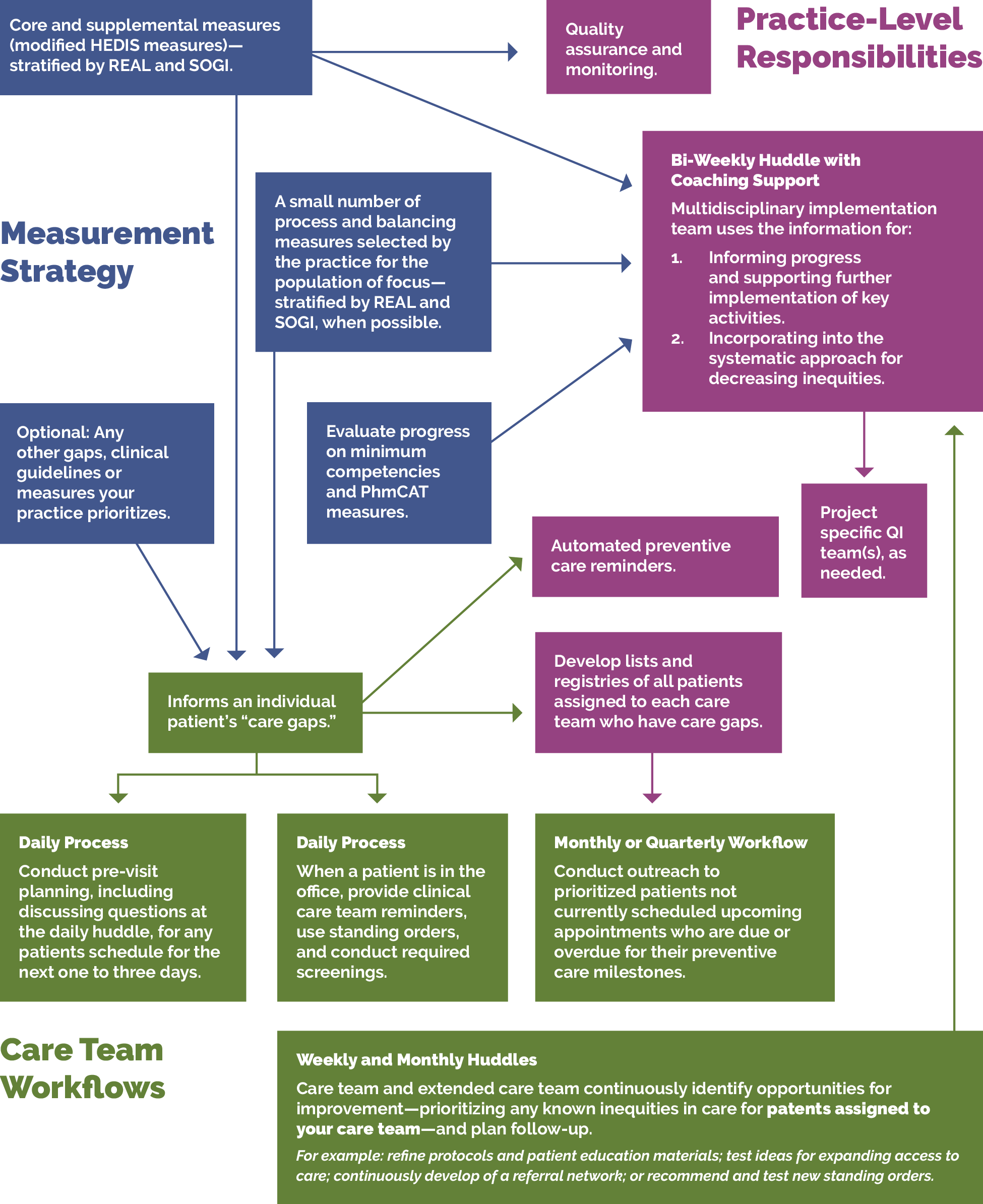
APPENDIX B:
Theory of Change
The key activities in this guide align with the PHMI theory of change for how practices can increase utilization of comprehensive care protocols for controlling high blood pressure and comprehensive diabetes care.
- Effective implementation of chronic care management protocols.
- Patients living with diabetes and hypertension have a care plan that effectively addresses their medical, behavioral and social health needs.
- Practices have needed resources and support.
FIGURE 22: PHMI PEOPLE WITH CHRONIC CONDITIONS DRIVER DIAGRAM.
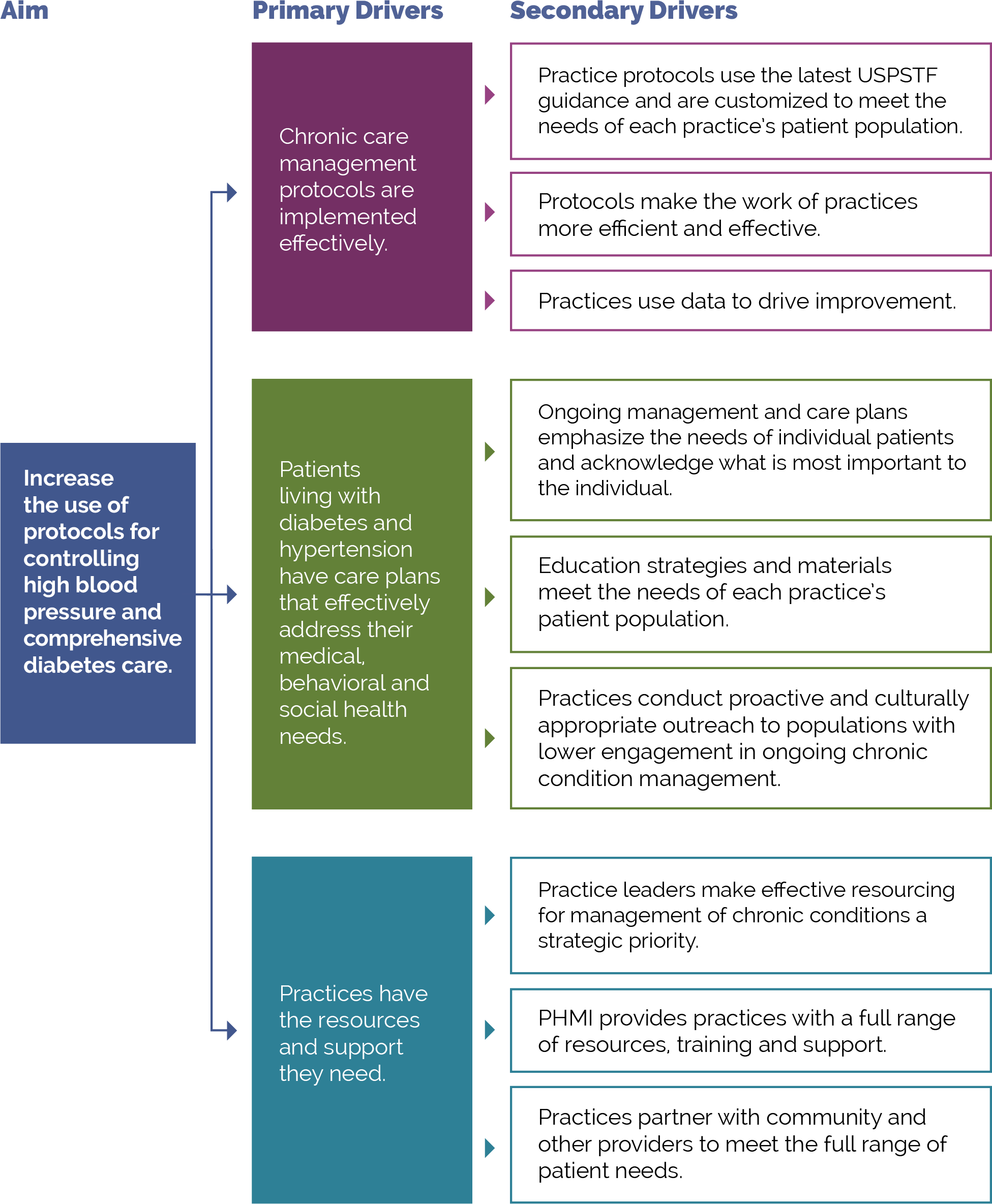
APPENDIX C:
C: Developing a Robust Measurement Strategy
FIGURE 23: DEVELOPING YOUR MEASUREMENT STRATEGY MILESTONES
The visual below illustrates the key milestones in the development of a robust measurement strategy.
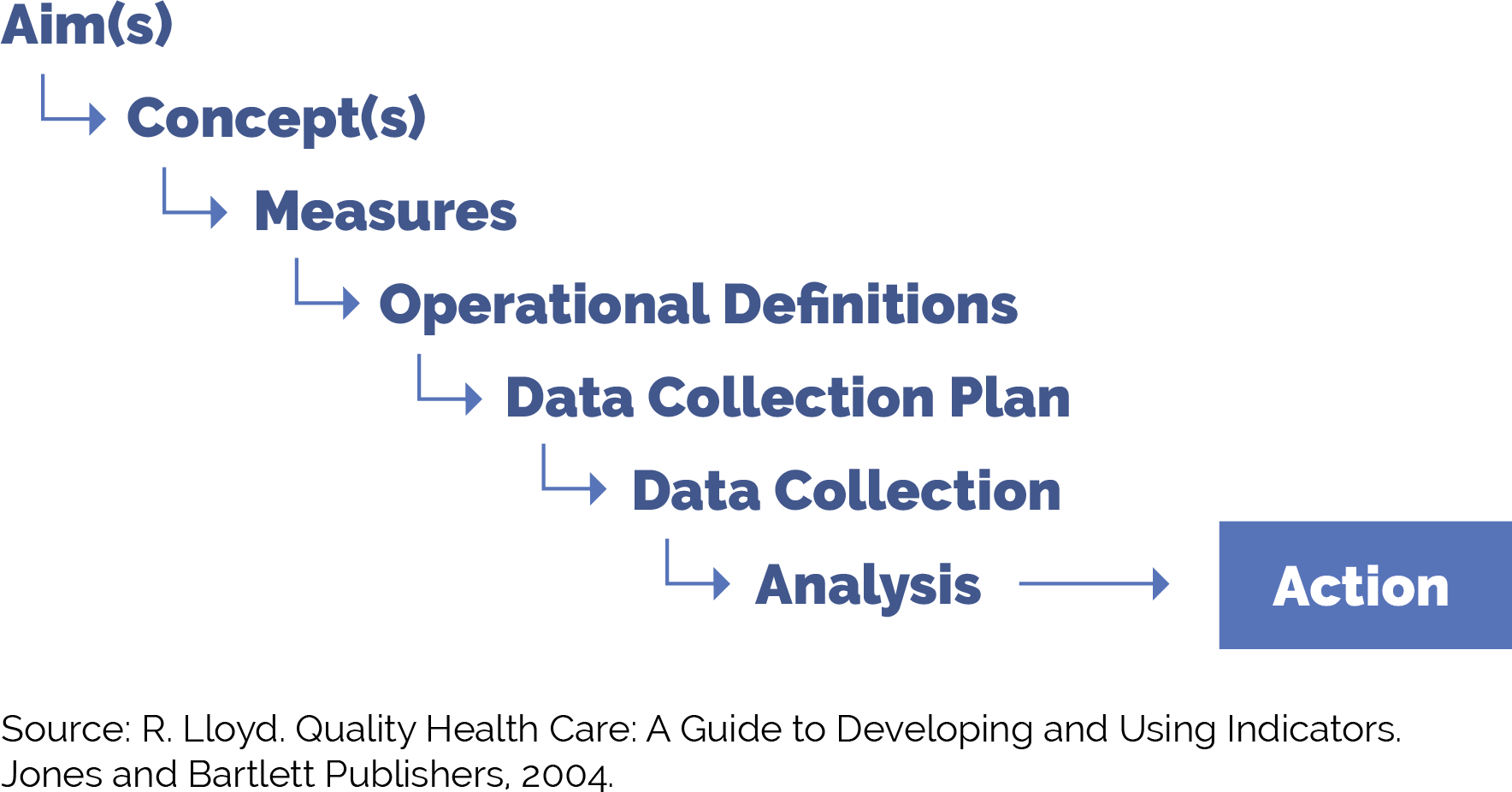
FIGURE 24: DEFINITION AND EXAMPLES FOR MEASUREMENT STRATEGY MILESTONES
Figure 24 provides guidance on each of these milestones as you work to put in place a robust yet practical measurement strategy.
Milestone |
Definition |
Example |
|---|---|---|
Aim(s) |
The overall goal(s) of the improvement effort. “What are we trying to accomplish?” We often recommend sub-aims to focus your team on intermediate goals. You can develop data-informed specific, measurable, achievable, relevant, time-bound, inclusive and equitable (SMARTIE) goals focused on increasing adherence to specific AAP preventive care guidelines year over year among attributed patients or subpopulations of patients. |
Adults who are diagnosed with diabetes will regularly monitor their hemoglobin A1c. Example sub-aim: The percentage of Black patients aged 18 years or older with elevated or hypertensive blood pressure who have a follow-up plan documented will increase from 60% to 90% by December 2025. |
Concept(s) |
A general abstract notion (approach, thought, belief or perception) related to the aim(s) of focus. |
Ensure adequate monitoring of diabetes management for patients. |
Measures |
Specific objective ways to determine the extent to which an aim has been met or to determine if there has been improvement in the concepts of focus. Measures help us to answer the second question in the model for improvement: “How will we know that a change is an improvement?” Measures generally fall into one of three types:
|
For the purpose of this example, we will examine the percentage of adults who regularly monitor their hemoglobin A1c. |
Operational definitions |
Detailed descriptions in quantifiable terms of what to measure and the steps to follow to do so consistently each time and over time. The operational definitions help make the measures clear and unambiguous and often contain criteria for inclusion and exclusion and numerator/denominator. |
Percentage of 18- to 75-year-old people with diabetes whose hemoglobin A1c was not under control (>9%). See CMS122v11 for more information on inclusion criteria. |
Data collection plan |
A detailed set of instructions that generally includes:
|
Percentage of 18- to 75-year-old people with diabetes whose hemoglobin A1c was not under control (>9%): Who:
How:
Where and how the data will be stored:
When the data will be collected:
How often:
|
Data collection |
The process of collecting the agreed upon measures in accordance with the relevant operational definitions and the agreed upon data collection plan. |
Data will be collected through automated EHR reports. |
Analysis and action |
The process of analyzing the data, including instructions for the analysis and visualization of the data, disseminating the data to relevant parties, and using the data to track progress and guide improvement efforts. |
The quality improvement team reviews the percentage of 18- to 75-year-old people whose hemoglobin A1c was not under control (>9%) on a monthly basis, and the care team and panel manager review the data subsequently once per quarter or every six months for ongoing monitoring. |
POPULATION HEALTH GUIDE FOR UNDERTAKING 3 PART DATA REVIEW
The three part data review is a tool that can be used to advance work related to population health. It draws on asset-based inquiry, to surface to identify needs and opportunities to understand the ways in which systems have discarded or undervalued the assets of individuals and communities. Groups can then work together to ensure that all can contribute to advancing population health and well-being and dismantling inequities. Access the full resource.
APPENDIX D:
Other Sources Reviewed in the Writing of This Guide
APPENDIX E:
Guidance on Technological Interventions
EHRs were primarily designed to manage individual patients rather than groups of patients. However, over time, EHRs have increasingly added functionality for population-level quality reporting and management, and for some degree of care planning and care coordination, especially to support value-based care tracking and reporting. Practices should evaluate your EHR capabilities against specifically designed population management applications. While these applications require interface with the EHR, they generally offer additional functionality. While EHR solutions are integrated with EHR data, they still usually require import of data from outside sources to be optimally useful. Managed care organizations may provide care coordination and population management applications, usually only for their own enrolled patients. EHR-based solutions may also pose challenges where groups of practices using different EHR solutions are collaborating in value-based care contracts.
In value-based care arrangements, practices are responsible for attributed patients who may have never been seen. Since these patients do not have records in the EHR, practices need to consider how they can manage these patients to engage them into care at the practice in the absence, at least initially, of the patients having records within the EHR. If your practice is using freestanding applications for this, it needs the capacity to handle these attributed patients who have not been registered as patients.
Figure 25 below includes the technical functionalities required to support population management for adults with chronic conditions. These requirements can guide the evaluation of existing solutions or guide the development of requirements in evaluating potential new applications. The figure also indicates the data sources required to enable the functionality.
FIGURE 25: CORE POPULATION HEALTH MANAGEMENT FUNCTIONALITY REQUIREMENT
Functionality |
Population Health Management Requirement Description |
Data Acquisition Dependency |
|---|---|---|
Care guidelines |
Identify care gaps for all adults with chronic conditions against care protocol. Care guidelines may be presentable to the clinical provider/support team at the point of care through the EHR, in the visit workflow as pre-visit prep/team huddle, through registries as above, and aspirationally as prompts to patients/caregivers. |
Commercial EHR-embedded guidelines provided by vendor or customized by practice. External source guidelines (clinical guidelines). Reference sites made available electronically. |
Registries |
Identify care gaps for all adults with chronic conditions against care protocol. Care guidelines may be presentable to the clinical provider/support team at the point of care through the EHR, in the visit workflow as pre-visit prep/team huddle, through registries as above, and aspirationally as prompts to patients/caregivers. Ability to produce registries (list/cohort of patients) organized to facilitate population management: Adults in age ranges relevant to measures and/or clinical standards. Adults sharing designated high-risk criteria (medical, behavioral, social needs) impacting their ability to achieve guidelines. These registries should consider the inclusion of functionality to trigger automated, predefined action(s) and/or human-initiated action(s) for all or a defined subset of patients comprising the registry. Suggested HIT assets that can be leveraged to achieve this function include: EHR – generates a list of patients who meet the criteria for inclusion in the population of focus. Track using an external database. Consider merging patients from an external data source, such as a payor, to have a complete roster. Population health management tool – specialized chronic disease management applications (some of which include patient-facing components). |
EHR:
External data sources, such as: reference labs, specialty care, immunization registries, social service clinicians’ data. Data from home devices such a glucometers and home blood pressure monitoring devices.
|
Clinical decision support (CDS) |
Care gaps should be displayed based on what is due, with insight into previous results, to support clinicians’ ability to make decisions at the point of care (POC) for the provider and care team members supporting non-POC management. Care guidelines may be presentable as clinical decision support to the clinical provider/support team at the point of care, in the visit workflow as pre-visit prep/team huddle, through registries as above, and aspirationally as prompts to patients/caregivers. While EHR-based prompts are usually thought of as ideal, team-based care presents an opportunity for clinical decision support to be presented to other members of the care team through other channels. The Five Rights Framework Clinical Decision Support: More Than Just ‘Alerts’ Tipsheet is a useful guidance to help health centers to support decision-making across a wider range of the care delivery life cycle, broader teams and technology other than the EHR to look beyond office visits and providers. This is especially important to avoid “alert fatigue” and burnout. |
Internal EHR data. External source clinical data. Claims data (clinical lag should be noted). Electronic guideline specifications. Patient-contributed data. |
Care dashboards and reports |
Adults with chronic conditions dashboard: population view by eligible study with sorting/filtering capability based on characteristics to be defined by the practice, with ability for care team/case managers to document the actions completed; ability to see care gaps at a patient level and population level according to health center-prioritized care guidelines. Note that to automate these reports, it is necessary to apply standardized data collection strategies against electronically specified protocols. |
Same as above (EHR data and external data sources. Data from other sources of care). Claims data. |
Quality reports |
Same as above by quality measures, as opposed to care guidelines; ability to track HEDIS as well as customized measures and UDS. |
Quality measure specifications. Same as above (EHR data and external data sources). Data from other sources of care. Claims data. |
Risk stratification |
Ability to categorize risk for patients and develop lists according to risk classification (tie to registry). Can be imported as externally generated risk score or calculated internally according to proprietary or customized risk algorithm. |
Data acquisition platform ingestion: already curated high-risk list ingested and utilized downstream in the journey and/or additional internal and external data sources to populate defined risk model. |
Outreach and engagement |
Allow for outreach to support previsit planning or post-visit care needs, such as assessments. Technology channels include population registry outputs; patient-facing applications, such as patient portals; freestanding text messaging; and self-assessment/self-management applications.
|
Same as above (clinical/EHR/etc.) Claims.
|
Care management |
Allow for management of specific and unique care needs for high-risk patients. Care management requires the ability for multiple members of the care team to contribute to and rack elements of the plan. Challenges with freestanding care management applications include access to data from other sources of care, including the ability to track referrals, and workflow burden of staff utilizing multiple applications. Ability of the care management application to draw from and “write back” to the EHR is desirable but difficult to achieve.
|
Care management protocols. Appointment data: internal/external. Clinical data from external service providers.
|
FIGURE 26: USE OF TECHNOLOGY FOR RECOMMENDED SCREENING FOR FOUNDATIONAL KEY ACTIVITIES
This figure identifies strategies for using digital tools to complete appropriate screeners as recommended by clinical guidelines. Using technology to facilitate screening may streamline the workflow and preserve patient confidentiality where necessary.
ID |
Focus Area |
Completion of Digital Screeners |
Data Acquisition Dependency |
|---|---|---|---|
1 |
Depression screening |
In-office tablet-based screening and/ or remote patient-facing application-based self-completed screening.
|
Population health and EHR integration of screener responses or, at minimum, scores. |
2 |
Anxiety screening |
In-office tablet-based screening and/ or remote patient-facing application-based self-completed screening.
|
Population health and EHR integration of screener responses or, at minimum, scores. |
3 |
Unhealthy substance use screening |
In-office tablet-based screening and/ or remote patient-facing application-based self-completed screening.
|
Population health and EHR integration of screener responses or, at minimum, scores. |
4 |
Social needs screening |
In-office tablet-based screening and/ or remote patient-facing application-based self-completed screening.
|
Population health and EHR integration of screener responses or, at minimum, scores. |
FIGURE 27: USE OF TECHNOLOGY FOR PATIENT OUTREACH AND PVP FOR FOUNDATIONAL KEY ACTIVITIES
This figure outlines the use of technology to facilitate specific activities and potential technology solutions that can optimize the uptake and efficiency of in-office visits.
ID |
Technology Focus |
Patient Outreach and Pre-Visit Planning |
Data Acquisition Dependency |
|---|---|---|---|
1 |
Portal-based communication |
|
EHR interface and integration. |
2 |
AI-enabled chatbots |
Identifying issues that need to be addressed before an office visit can be converted to telehealth visits. |
Population health and EHR incorporation of screening scores and responses. |
3 |
Text messaging |
Appointment reminders. |
EHR interface and integration. |
FIGURE 28: USE OF TECHNOLOGY FOR ENHANCED PATIENT ENGAGEMENT AND VIRTUAL CARE FOR GOING DEEPER ACTIVITIES
The figure identifies technology solutions to engage patients asynchronously from office visits for a variety of use cases to enhance care and patient experience.
ID |
Focus Area |
Patient Engagement and Mobile Technology |
Data Acquisition Dependency |
|---|---|---|---|
1 |
AI-enabled chatbots |
|
EHR integration. |
2 |
|
EHR and population health integration. |
FIGURE 29: USE OF TECHNOLOGY FOR INNOVATIONS IN CARE DELIVERY FOR ON THE HORIZON ACTIVITIES
The figure describes technology strategies that can enhance care delivery by using artificial intelligence and advanced technology tools.
ID |
Focus Area |
Artificial Intelligence and Innovation |
Data Acquisition Dependency |
|---|---|---|---|
1 |
Predictive analytics |
|
EHR integration, population health, and patient engagement application integration. |
2 |
Artificial intelligence (AI)- enabled diagnostics |
|
EHR integration and population health integration. |
RECOMMENDED CITATION AND ACKNOWLEDGEMENTS
Recommended citation:Burgess K, Brettler J, Roy B, Deane M, Baker L, Howard P, Donald F, Rachman F, Esmond W. Adults Living with Chronic Conditions Implementation Guide. In: Coleman K, Mital M, editors. Population Health Management Initiative Populations of Focus Implementation Guide Series. 1st ed. Oakland, CA: Kaiser Permanente; 2024.
Acknowledgments: We gratefully acknowledge the contributions of the many staff and representatives of the Institute for Healthcare Improvement (IHI), AllianceChicago, Center for Care Innovations (CCI), JSI Inc and the Center for Excellence in Primary Care at University of California, San Francisco along with Pyramid Communications and Kaiser Permanente’s Population Health Management Initiative (PHMI) team for crafting this work.
In addition, we are grateful for the partnership of the Department of Health Care Services (DHCS), Community Health Center partners in PHMI, representatives from the California Primary Care Association and the Regional Associations of California (RAC) along with the many other academic, health plan and consulting partners who shared their expertise and insights freely as we collaboratively designed the initiative and created these guides.
Special thanks to the individual reviewers of this first edition of the Populations of Focus Implementation Guide Series who significantly strengthened this work, including: Jeff Norris, Laura Miller, David Tian, Karen Mark, Palav Babaria (DHCS); Jennifer Sayles (Pop Health Learning Center); Roger Chaufournier, Christine St. Andre (IHI); Kathleen Figoni, Angela Sherwin (CCI).
Endnotes
- Chronic diseases in America [Internet]. Centers for Disease Control and Prevention; 2022 [cited 2023 Oct 23]. Available from: https://www.cdc.gov/chronic-disease/about/index.html
- Price JH, Khubchandani J, McKinney M, Braun R. Racial/ethnic disparities in chronic diseases of youths and access to healthcare in the United States. Biomed Res Int. 2013;2013:787616. doi: 10.1155/2013/787616. Epub 2013 Sep 23. PMID: 24175301; PMCID: PMC3794652.
- New Federal Resources for factoring social determinants of health into clinical practice [Internet]. Agency for Healthcare Research and Quality (AHRQ); 2023 [cited 2023 Dec 1]. Available from: https://integrationacademy.ahrq.gov/news-and-events/news/new-federal-resources-factoring-social-determinants-health-clinical-practice
- American Diabetes Association. Erratum: standards of care in diabetes—2023 abridged for Primary Care clinicians. Clin diabetes 2023;41:4–31. Standard of Care in Diabetes--2023. 2022 Dec 12;41(2):328–328. doi:10.2337/cd23-as01
- Clinical decision support [Internet]. 2018 [cited 2024 Jan 8]. Available from: https://www.healthit.gov/topic/safety/clinical-decision-support
- Institute of Medicine. 2003. Unequal Treatment: Confronting Racial and Ethnic Disparities in healthcare. Washington, DC: The National Academies Press. https://doi.org/10.17226/10260
- Improving Health Equity: Build Infrastructure to Support Health Equity. Guidance for Healthcare Organizations. Boston, Massachusetts: Institute for Healthcare Improvement; 2019. (Available at www.ihi.org)
- Chadha N, Lim B, Kane M, Rowland B. Institute for Healing and Justice in Medicine; 2020. https://belonging.berkeley.edu/race-medicine
- REAL Data Collection Toolbox [Internet]. KHA; 2022 [cited 2023 Dec 18]. Available from: https://www.khaquality.com/wp-content/uploads/2024/01/HQIC_REaL-Data_Collection_Toolbox.pdf
- McLean SM, Booth A, Gee M, Salway S, Cobb M, Bhanbhro S, Nancarrow SA. Appointment reminder systems are effective but not optimal: results of a systematic review and evidence synthesis employing realist principles. Patient Prefer Adherence. 2016 Apr 4;10:479-99. doi: 10.2147/PPA.S93046. PMID: 27110102; PMCID: PMC4831598.
- Perron NJ, Dao MD, Kossovsky MP, Miserez V, Chuard C, Calmy A, Gaspoz JM. Reduction of missed appointments at an urban primary care clinic: a randomised controlled study. BMC Fam Pract. 2010 Oct 25;11:79. doi: 10.1186/1471-2296-11-79. PMID: 20973950; PMCID: PMC2984453.
- McLean SM, Booth A, Gee M, Salway S, Cobb M, Bhanbhro S, Nancarrow SA. Appointment reminder systems are effective but not optimal: results of a systematic review and evidence synthesis employing realist principles. Patient Prefer Adherence. 2016 Apr 4;10:479-99. doi: 10.2147/PPA.S93046. PMID: 27110102; PMCID: PMC4831598.
- Leubner J, Wild S. Developing Standing Orders to Help Your Team Work to the Highest Level. Fam Pract Manag. 2018 May/Jun;25(3):13-16. PMID: 29989776.
- Standing orders [Internet]. [cited 2024 Jan 16]. Available from: https://cepc.ucsf.edu/standing-orders
- Bellows BK, Kazi DS. Ultralow-dose quadruple combination therapy: A cost-effective solution for hypertension control. Heart. 2023;109(22):1659–60. doi:10.1136/heartjnl-2023-323007
- Petrie JR, Guzik TJ, Touyz RM. Diabetes, hypertension, and cardiovascular disease: Clinical insights and vascular mechanisms. Canadian Journal of Cardiology. 2018;34(5):575–84. doi:10.1016/j.cjca.2017.12.005
- Derington CG, Bress AP, Herrick JS, Jacobs JA, Zheutlin AR, Berchie RO, et al. Antihypertensive medication regimens used by US adults with hypertension and the potential for fixed‐dose combination products: The National Health and Nutrition Examination Surveys 2015 to 2020. Journal of the American Heart Association. 2023 May 6;12(11). doi:10.1161/jaha.122.028573
- Mulvaney-Day N, Marshall T, Downey Piscopo K, Korsen N, Lynch S, Karnell LH, Moran GE, Daniels AS, Ghose SS. Screening for Behavioral Health Conditions in Primary Care Settings: A Systematic Review of the Literature. J Gen Intern Med. 2018 Mar;33(3):335-346. doi: 10.1007/s11606-017-4181-0. Epub 2017 Sep 25. PMID: 28948432; PMCID: PMC5834951.
- Hibbard JH, Greene J. What the evidence shows about patient activation: better health outcomes and care experiences; fewer data on costs. Health Aff (Millwood). 2013 Feb;32(2):207-14. doi: 10.1377/hlthaff.2012.1061. PMID: 23381511.
- AHRQ Health Literacy Universal Precautions Toolkit [Internet]. 2020 [cited 2024 Jan 12]. Available from: https://www.ahrq.gov/health-literacy/improve/precautions/index.html
- Equitably addressing social determinants of health and chronic diseases [Internet]. Centers for Disease Control and Prevention; 2022 [cited 2024 Jan 12]. Available from: https://www.cdc.gov/health-equity-chronic-disease/social-determinants-of-health-and-chronic-disease/index.html
- Alegría, M., NeMoyer, A., Falgàs Bagué, I., Wang, Y., & Alvarez, K. (2018). Social Determinants of Mental Health: Where We Are and Where We Need to Go. Current psychiatry reports, 20(11), 95. https://doi.org/10.1007/s11920-018-0969-9
- Ruiz Escobar E, Pathak S, Blanchard CM. Screening and Referral Care Delivery Services and Unmet Health-Related Social Needs: A Systematic Review. Preventing Chronic Disease. 2021 Aug 12;18.
- Chavez, L. J., Tyson, D. P., Davenport, M. A., Kelleher, K. J., & Chisolm, D. J. (2023). Social Needs as a Risk Factor for Positive Postpartum Depression Screens in Pediatric Primary Care. Academic pediatrics, S1876-2859(23)00095-5. Advance online publication. https://doi.org/10.1016/j.acap.2023.03.007
- Ruiz Escobar E, Pathak S, Blanchard CM. Screening and Referral Care Delivery Services and Unmet Health-Related Social Needs: A Systematic Review. Preventing Chronic Disease. 2021 Aug 12;18.
- Califf, R. M., Wong, C., Doraiswamy, P. M., Hong, D. S., Miller, D. P., Mega, J. L., & Baseline Study Group (2022). Importance of Social Determinants in Screening for Depression. Journal of general internal medicine, 37(11), 2736–2743. https://doi.org/10.1007/s11606-021-06957-5
- Food insecurity [Internet]. [cited 2024 Jan 12]. Available from: https://health.gov/healthypeople/priority-areas/social-determinants-health/literature-summaries/food-insecurity
- National Academies of Sciences, Engineering, and Medicine; National Academy of Medicine; Committee on the Future of Nursing 2020–2030; Flaubert JL, Le Menestrel S, Williams DR, et al., editors. The Future of Nursing 2020-2030: Charting a Path to Achieve Health Equity. Washington (DC): National Academies Press (US); 2021 May 11. 2, Social Determinants of Health and Health Equity. Available from: https://www.ncbi.nlm.nih.gov/books/NBK573923/
- Butler, AB ED, Morgan, MD, MSc, MSHP AU, Kangovi, MD, MS S. Screening for Unmet Social Needs: Patient Engagement or Alienation? NEJM Catalyst [Internet]. 2020 Jul 20; Available from: https://catalyst.nejm.org/doi/full/10.1056/CAT.19.1037
- Kaiser Permanente Research Affiliates Evidence-based Practice Center. Screening and Interventions for Social Risk Factors: A Technical Brief to Support the U.S. Preventive Services Task Force [Internet]. 2021. Available from: https://www.uspreventiveservicestaskforce.org/uspstf/sites/default/files/inline-files/Social%20Risk%20Factors%20Tech%20Brief_Assembled%20for%20Web_Sep%202021_1.pdf
- Rojas L, Project S. Accountable Health Communities (AHC) Model Evaluation Second Evaluation Report RTI Point of Contact [Internet]. 2023 [cited 2024 Jan 16]. Available from: https://www.cms.gov/priorities/innovation/data-and-reports/2023/ahc-second-eval-rpt
- Sınger A, Coleman K, Mahmud A, Holden E, Stefanik-Guizlo K. Assessing the Feasibility of an Empathic Inquiry Approach to Social Needs Screening in 10 Federally Qualified Health Centers. The Permanente Journal. 2023 Dec 15;27(4):136–42.
- Byhoff E, Gottlieb LM. When There Is Value in Asking: An Argument for Social Risk Screening in Clinical Practice. Ann Intern Med. 2022;175(8):1181-1182. doi:10.7326/M22-0147
- American College of Physicians. Closing-the-Loop. Baltimore: Transforming Clinical Practice Initiative--CMS; 2015.
- What We’re Learning About Delivering Whole-Person Care [Internet]. 2020. Available from: https://healthleadsusa.org/wp-content/uploads/2020/01/CASHI_Report_Final1.pdf
- Patel, M.P., Schettini, P., O’Leary, C.P. et al. Closing the Referral Loop: an Analysis of Primary Care Referrals to Specialists in a Large Health System. J GEN INTERN MED 33, 715–721 (2018). https://doi.org/10.1007/s11606-018-4392-z
- American College of Physicians. Transforming Clinical Practice Initiative SAN Power Packs: Closing the Loop. Centers for Medicare & Medicaid Services; 2019. Available from: https://www.cms.gov/priorities/innovation/files/x/tcpi-san-pp-loop.pdf
- Reducing Care Fragmentation: A Toolkit for Coordinating Care [Internet]. The Center for Accelerating Care Transformation. The Commonwealth Fund; 2010. Available from: https://www.act-center.org/application/files/7016/3112/2157/Toolkit_Reducing_Care_Fragmentation.pdf
- Enhanced Care Management and Community Supports [Internet]. [cited 2024 Jan 12]. Available from: https://www.dhcs.ca.gov/CalAIM/ECM/Pages/Home.aspx
- Medi-Cal Transformation: Enhanced Care Management [Internet]. DHCS; [cited 2024 Jan 12]. Available from: https://www.dhcs.ca.gov/CalAIM/Documents/CalAIM-ECM-a11y.pdf
- Weiner M, Perkins AJ, Callahan CM. Errors in completion of referrals among older urban adults in ambulatory care. J Eval Clin Pract. 2010;16(1):76-81. doi:10.1111/j.1365-2753.2008.01117.
- Mehrotra A, Forrest CB, Lin CY. Dropping the baton: specialty referrals in the United States. Milbank Q. 2011;89(1):39–68. doi: 10.1111/j.1468-0009.2011.00619.
- Mehrotra A, Forrest CB, Lin CY. Dropping the baton: specialty referrals in the United States. Milbank Q. 2011;89(1):39–68. doi: 10.1111/j.1468-0009.2011.00619.
- Transitions of care [Internet]. 2023 [cited 2024 Feb 8]. Available from: https://www.ncqa.org/hedis/measures/transitions-of-care/
- Cai C, Gaffney A, McGregor A, Woolhandler S, Himmelstein DU, McCormick D, et al. Racial and ethnic disparities in outpatient visit rates across 29 specialties. JAMA Internal Medicine. 2021 Nov 1;181(11):1525. doi:10.1001/jamainternmed.2021.3771